- Search
| Neurospine > Volume 18(2); 2021 > Article |
|
|
Abstract
Objective
The Patient Health Questionnaire-9 (PHQ-9) is a screening tool for evaluating depressive symptoms. Research is scarce regarding the validity and correlation of PHQ-9 scores with other patient-reported outcomes of mental health after minimally invasive lumbar discectomy (MIS LD). We aim to validate PHQ-9 as a metric for assessing mental health in MIS LD patients.
Methods
A database was retrospectively reviewed for patients who underwent elective, single-level MIS LD. Patients were excluded if they had incomplete preoperative PHQ-9, 12-item Short Form Health Survey (SF-12), or Veterans RAND 12-item health survey (VR-12). Survey scores were collected preoperatively and postoperatively through 1 year. Mean scores were used to calculate postoperative improvement from preoperative scores. Correlation of PHQ-9 with SF-12 mental composite score (MCS) and VR-12 MCS scores was also calculated. Correlation strength was assessed by the following categories: 0.1 Ōēż |r| < 0.3 = low; 0.3 Ōēż |r| < 0.5 = moderate; |r| Ōēź 0.5 = strong.
Results
A total of 239 patients underwent single-level MIS LD. PHQ-9, VR-12 MCS, and SF-12 MCS all demonstrated statistically significant increases from preoperative scores at all postoperative timepoints (p Ōēż 0.001). SF-12 MCS and VR-12 MCS were each observed to have strong and significant correlations with PHQ-9 at all timepoints when evaluated with both Pearson correlation coefficients and partial correlation coefficients.
Conclusion
We observed that PHQ-9, SF-12 MCS and VR-12 MCS all significantly improve following lumbar discectomy and that PHQ-9 scores strongly correlated with these previously established measures. Our results substantiate evidence from other surgical fields that PHQ-9 scores are a valid tool to evaluate pre- and postsurgical depressive symptoms.
According to a recent report by the National Center for Health Statistics, approximately 8.1% of United States adults experienced significant depressive symptoms lasting for at least 2 weeks between 2013 and 2016 [1]. Past studies have emphasized the prevalence of mental health disorders in spine patients, reporting that 59% of individuals with chronic low back pain presented with current symptoms of one or more psychiatric diagnoses [2]. These findings are especially important to note in the context of observations regarding the impact of depression on spine surgery outcomes. For example, Menendez et al. [3] reported that spine surgery patients with preoperative depression had a higher risk of perioperative adverse events over those without depressive symptoms. Another study by Miller et al. [4] demonstrated that higher preoperative depression was correlated with diminished improvement in quality of life following lumbar spine surgery. These studies emphasize the importance of a reliable and valid means of assessing depressive symptoms in the clinical spine setting.
Patient Health Questionnaire-9 (PHQ-9) is a self-reported questionnaire that quantifies depression severity using 9 questions based on the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV) criteria for major depressive disorder. Scores can range from 0 to 27, as each question is scored from 0 (not at all) to 3 (nearly every day), based on the frequency with which patients experience various effects of depressive symptoms. The PHQ-9 has been validated in a variety of clinical settings and has demonstrated several advantages over other mental health assessment tools, such as 12-item Short Form health survey (SF-12) and Beck Depression Inventory (BDI) [5]. For example, PHQ-9 may be less time consuming than SF-12 and BDI, which have 12 and 21 questions, respectively. Additionally, its frequency-based responses allow clinicians to assess severity of depressive symptoms, and its basis on DSM-IV diagnosis provides logical validity [6]. Furthermore, the widespread use of this survey in both primary care and spine surgery settings means this data may be readily available for many patients [7,8]. Patel et al. [9] utilized PHQ-9 scores to assess the relationship between preoperative depression and postoperative outcomes following transforaminal lumbar interbody fusion and found that patients experiencing depressive symptoms reported greater pain, higher narcotic consumption, and poorer postoperative improvement. As the use of PHQ-9 continues to expand, it is critical to validate this tool on a procedure-specific level against other empirically supported mental health measures.
Parrish et al. [10] previously validated PHQ-9 in the cervical spine and reported strong correlations between PHQ-9, SF-12 mental composite score (MCS), and Veterans RAND 12-item health survey (VR-12) MCS in patients undergoing either anterior cervical discectomy and fusion or cervical disc replacement. While PHQ-9 has also been validated in lumbar fusions [11], the drastic differences in indications, duration of symptoms, and outcomes among different spinal procedures necessitates that its use be validated for the specific populations, pathologies, and techniques associated with additional procedures.
Minimally invasive lumbar discectomy (MIS LD) has been established as a reliable intervention with positive long-term results for the treatment of disc herniation [12], which is a common cause of lower back pain, sciatica, and neurological deficits [13]. However, depression may substantially interfere with this procedureŌĆÖs effectiveness and place patients at further risk for neurological complications. Additionally, Chaichana et al. [14] also demonstrated that patients with preoperative depression did not experience meaningful improvement in disability and quality of life at the same rates as others following LD. While the mental health psychometric SF-12 MCS has been extensively investigated for its validity in a wide variety of populations [15-18], there still a dearth of studies that validate the use of PHQ-9 in both pre- and postoperative settings. Moreover, due to the frequency with which LDs are performed and their relationship with preoperative depression, it is important to assess the validity of PHQ-9 in this procedure-specific manner. This study aims to validate PHQ-9 as an appropriate metric for assessing mental health in patients undergoing MIS LD.
Prior to study commencement, approval by the Institutional Review Board of Rush University Medical Center (ORA #1405-1301) and informed patient consent were obtained. A prospectively maintained surgical registry was retrospectively reviewed for patients who underwent primary, single-level MIS LD for degenerative spinal pathology from March 2016 until May 2019. Patients were excluded if they had not completed a PHQ-9, SF-12, or VR-12 survey at the preoperative timepoint or if their procedure was indicated due to trauma, malignancy, or infection. All MIS LD procedures were performed by the same fellowship-trained spine surgeon at a single academic institution.
Demographic and perioperative information was collected including age, sex, smoking status, body mass index categorized as < 30 kg/m2 (nonobese) or Ōēź 30 kg/m2 (obese), Charlson Comorbidity Index (CCI), operative duration (from incision to skin closure, in minutes), estimated blood loss (in mL), and postoperative length of stay (in hours). Patient mental health was assessed using PHQ-9, SF-12 MCS, and VR-12 MCS surveys at preoperative and postoperative (6 weeks, 12 weeks, 6 months, 1 year) timepoints. Surveys were completed either in the clinic using a provided tablet device or at the patientŌĆÖs home using a personal device. All surveys were administered and recorded through a secure, online Outcomes Based Electronic Research Database platform (OBERD, Columbia, MO, USA). Regular email-based reminders as well as outreach by clinical and/or research staff were utilized to maximize survey compliance.
All calculations and statistical analyses were performed using Stata 16.1 (StataCorp, College Station, TX, USA). Descriptive statistics were performed for all demographic and perioperative variables (Table 1). Mean scores were calculated for PHQ-9, SF-12 MCS, and VR-12 MCS at all timepoints and used to determine the mean change from baseline for each survey at each postoperative timepoint (Table 2). A paired Student t-test assessed improvements in each postoperative survey from preoperative baseline. Pearson correlation coefficient and time-controlled partial correlation coefficient were used to evaluate the relationship of PHQ-9 with SF-12 MCS and VR-12 MCS scores at each timepoint (Table 3). Correlation strength was assessed by the following categories: 0.1Ōēż |r|< 0.3 = low; 0.3Ōēż |r|< 0.5 = moderate; |r| Ōēź 0.5 = strong. Scatterplots were constructed to demonstrate relationships of PHQ-9 with SF-12 MCS and VR-12 MCS. PHQ-9 was further evaluated for discriminant validity using a 1-way analysis of variance. The threshold value for depression was set at 41.4 for SF-12 MCS based on prior clinical validity studies [17]. A p-value of < 0.05 was considered the threshold for statistical significance in all analyses.
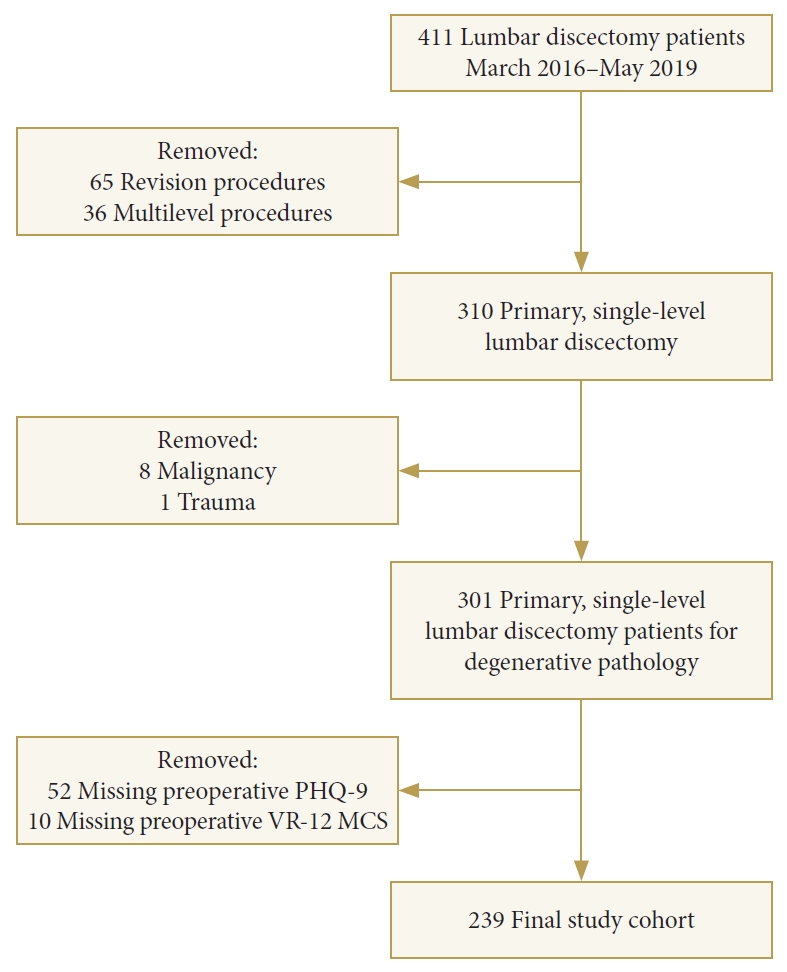
A total of 310 patients who underwent primary, single-level MIS LD were initially identified. Of these, 239 met full inclusion/exclusion criteria, as outlined in Fig. 1. The patient cohort had an average age of 42.4 years, 32% were female, 39% were obese, and mean CCI was 0.8 (Table 1). Mean operative duration was 41 minutes, mean estimated blood loss was 25.8 mL, and mean postoperative length of stay was 5.3 hours (Table 1).
A summary of postoperative changes in all PROMs is found in Table 2. A total of 58 patients had completed one or more surveys at the final, 1-year timepoint. Mean baseline preoperative scores were 6.7 ┬▒ 6.0 for PHQ-9, 47.9 ┬▒ 11.2 for SF-12 MCS, and 50.0 ┬▒ 10.05 for VR-12 MCS. Following lumbar discectomy, PHQ-9 mean values demonstrated a significant improvement from baseline values at the 6-week (3.6 ┬▒ 4.8), 12-week (3.8 ┬▒ 5.5), 6-month (3.8 ┬▒ 5.0), and 1-year (4.1 ┬▒ 6.1) postoperative timepoint (p < 0.001, all). This corresponded to a mean postoperative change in PHQ-9 which ranged from 3.0 ┬▒ 5.8 at 12 weeks to 3.6 ┬▒ 6.8 at 1 year.
For SF-12 MCS, mean values significantly improved from baseline at the 6-week (53.3 ┬▒ 10.0), 12-week (53.8 ┬▒ 10.3), 6-month (53.6 ┬▒ 9.1), and 1-year (51.5 ┬▒ 11.2) postoperative timepoint (p < 0.001). This also corresponded to changes in SF-12 MCS that ranged from the smallest change of 5.3 ┬▒ 11.0 at 6-week to the largest change of 7.0 ┬▒ 11.0 at 6-month.
Lastly, for VR-12 MCS, a significant improvement in postoperative values was demonstrated at the 6-week (56.0 ┬▒ 10.2), 12-week (57.0┬▒10.4), 6-month (56.6┬▒10.0), and 1-year (54.4┬▒12.9) timepoint (p < 0.001, all). These improvements in VR-12 MCS ranged from 6.0 ┬▒ 10.1 at its smallest and 7.3 ┬▒ 10.4 at its largest.
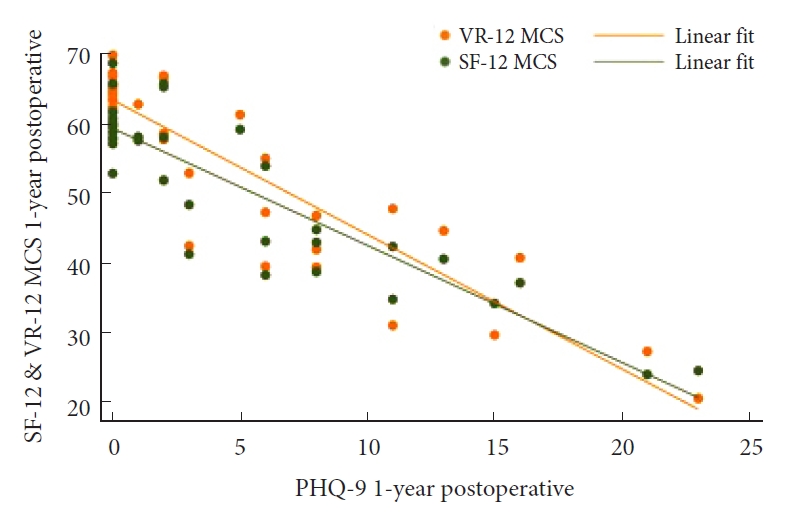
Pearson correlation coefficient and time-controlled partial correlation both demonstrated statistically significant correlations of PHQ-9 with SF-12 MCS at the preoperative (Fig. 2), 6-week (Fig. 3), 12-week (Fig. 4), 6-month (Fig. 5), and 1-year (Fig. 6) postoperative timepoints (p < 0.001, all) with all coefficients categorized as strong (|r|Ōēź 0.647, all). A similar result was observed for the relationship between PHQ-9 and VR-12 MCS with both Pearson correlation coefficient and time-controlled partial correlation demonstrating significant (p < 0.001, all) and strong (|r|Ōēź 0.778, all) at the preoperative (Fig. 2), 6-week (Fig. 3), 12-week (Fig. 4), 6-month (Fig. 5), and 1-year (Fig. 6) timepoints. A summary of these relationships can be found in Table 3.
Discriminant validity was established for PHQ-9 at all timepoints (p < 0.001, all) (Table 4). At the preoperative timepoint, PHQ-9 values demonstrated a sig nificant difference in mean values between depressed and non-depressed groups (4.3 ┬▒ 4.2 vs. 11.5 ┬▒ 6.3). Again, PHQ-9 mean values demonstrated a significant difference at the 6-week (2.1 ┬▒ 3.0 vs. 11.3 ┬▒ 5.9), 12-week (1.4 ┬▒ 2.2 vs. 10.8 ┬▒ 6.9), 6-month (2.3 ┬▒ 3.4 vs. 10.4 ┬▒ 5.9), and 1-year (1.8 ┬▒ 2.9 vs. 12.9 ┬▒ 6.7) postoperative timepoints.
Psychiatric disorders are highly prevalent among patients living with spinal pathology, with rates of depression ranging from 21.5% to 49.3% reported in those undergoing LD [19]. Depression has previously been associated with worse outcomes for lumbar spine surgery [4,9], and correlated with decreased rates of meaningful improvement in disability specifically for patients undergoing LD [14]. The PHQ-9 offers a number of advantages as a tool for assessing depression [5,6] and has previously been validated for use in the cervical spine [10] and for lumbar fusion surgeries [11]. The robust relationship between depressive symptoms and LD surgery makes validation of PHQ-9 a priority for this patient population.
The influence of depressive symptoms on postoperative outcomes of lumbar spine surgery has been well described in the literature. Patel et al. [9] used preoperative PHQ-9 scores to categorize patients undergoing transforaminal lumbar interbody fusions based on their level of depressive symptoms. The authors reported that patients with more severe depression not only reported greater levels of pain and increased narcotic consumption in the immediate postoperative period, but also demonstrated reduced improvement in pain, disability, and physical function 6-months after surgery. Similarly, in a study of LD patients, Chaichana et al. [14] also observed an association of depressive symptoms with poorer outcomes in terms of quality of life and disability.
Lumbar discectomy has demonstrated clear clinical benefits for patients with disc herniations and low back pain, in terms of both physical and mental health outcomes [20]. Lebow et al. [20] studied 100 patients undergoing microdiscectomy for lumbar disc herniation resulting in radiculopathy and found that depression, as measured by the Zung Self-Rating Depression Scale, significantly improved following surgery. Patients in our study demonstrated significant improvements in depression as measured by PHQ-9, as well as SF-12 and VR-12 MCS scores at 6-week through 1-year follow-up. In contrast, while LD patients in the study of Lebow et al. [20] did demonstrate improvements in depressive symptoms, these changes required 12-months following surgery to reach statistical significance.
Jenkins et al. [11] have previously validated PHQ-9 for use in patients undergoing lumbar fusion surgeries and found that PHQ-9 was strongly correlated with SF-12 and VR-12 MCS scores at all timepoints through 1 year. However, given possible differences in indications, symptomatology, and underlying spinal pathology associated with lumbar fusion, it is important to provide separate validation of PHQ-9ŌĆÖs utility for assessment of LD patients. LD is typically performed to correct herniations of the nucleus pulposus, which can result in acute radicular pain and neurological deficits [21]. While lumbar fusion can be indicated for recurrent herniations, it can also be indicated for a wider variety of structural issues of the spine which may be chronic and progressive in nature, such as spondylolisthesis and scoliosis [22]. Furthermore, time courses for these disorders can differ significantly. Lumbar disc herniations may present rather acutely, with rapid onset of pain and neurological symptoms and LD may be indicated for these patients after just a few weeks of failed conservative therapy [21]. In contrast, degenerative pathology such as spondylolisthesis may develop more chronically over the course of a patientŌĆÖs life and fusion surgery may not be recommended until the patient has participated in conservative treatment for at least several months [23]. These differences may be especially important to consider for the usage of PHQ-9 as they may relate to substantial differences in the way patientsŌĆÖ spinal pathologies and treatments interplay with depressive symptoms.
We were able to demonstrate significant, strong correlations of PHQ-9 with SF-12 and VR-12 MCS scores at all timepoints through 1-year in our cohort of patients undergoing MIS LD. Our use of a time-controlled partial correlation allows us increased confidence that these strong correlations represent true relationships between measures and were not simply related to the temporal proximity of survey completion. Additionally, PHQ-9 scores differed significantly between patients categorized as ŌĆ£depressedŌĆØ vs ŌĆ£not depressedŌĆØ, as measured by SF-12 MCS, at all timepoints, confirming strong discriminant validity for PHQ-9 to differentiate between patients with differing mental health status. These findings are in line with those of previous studies validating the use of PHQ-9 and provide further support for its utility as a measure of depressive symptoms for this patient population [10,11].
Originally adapted from their longer, 36-item predecessor, SF-12 and VR-12 MCS have been validated by a number of previous studies for the assessment of spine patients as well as the general population [17,24,25]. In particular, the ability of SF-12 MCS to demonstrate postoperative changes in patients undergoing LD surgery was verified by Vishwanathan and Braithwaite [26]. However, while these measures have demonstrated strong internal validity and responsiveness to change, their question designs lend themselves more to a general assessment of mental well-being. Conversely, the PHQ-9 is designed based on the DSM-IV and DSM-V to specifically assess patients for symptoms of major depression. Given the clear importance of understanding and quantifying depression in spine patients, the use of such a focused measure may be preferable.
Although our results allow us to confidently recommend the use of PHQ-9 to quantify depressive symptoms, our methodology is not without limitations. First, all procedures were performed by a single attending surgeon with extensive experience in MIS procedures at a single academic institution. This may limit the generalizability of our validation of PHQ-9 to other surgeons and patient populations. A follow-up study utilizing similar methodology, but with a multicenter design could significantly enhance the generalizability of these results. Additionally, our cohort was subject to significant attrition by the 1-year timepoint which may introduce an element of bias to our results if patients who continued to follow up significantly differed from those who did not. Furthermore, depressive symptoms were only characterized in terms of self-reported survey data. Diagnosis by a licensed mental health professional is considered the gold-standard for classification of depression and could have provided additional validity to our analysis. Finally, the power of our analysis was limited by lower survey completion rates at long-term follow-up.
Significant improvements in mental health were demonstrated in all 3 included measures through 1-year following MIS LD. Scores for PHQ-9 were strongly correlated with those of SF-12 and VR-12 MCS from the preoperative timepoint through 1 year. These results, considered alongside those of previous studies examining the use of PHQ-9 in spine surgery, allow us to confidently substantiate the validity of this measure to quantify depressive symptoms in patients undergoing MIS LD.
Fig.┬Ā2.
Correlation of PHQ-9 with both SF-12 MCS and VR-12 MCS at the preoperative timepoint. PHQ-9, Patient Health Questionnaire-9; SF-12 MCS, 12-item Short Form health survey mental composite score; VR-12 MCS, Veterans RAND 12-item health survey mental composite score.
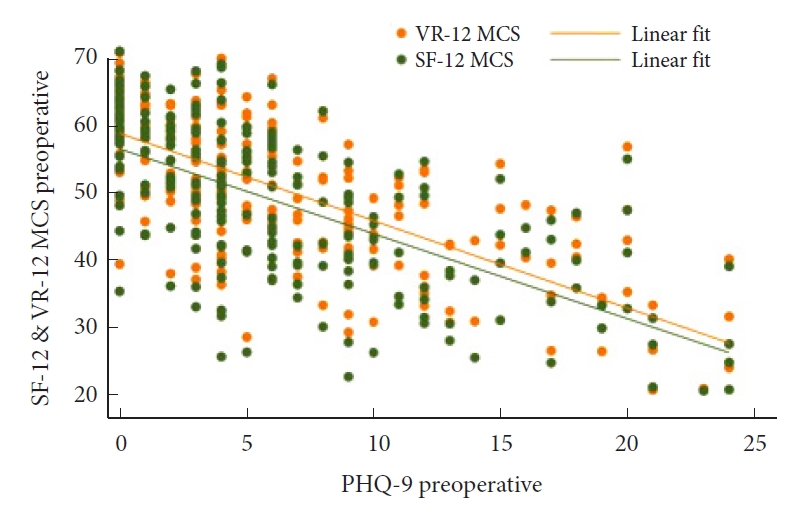
Fig.┬Ā3.
Correlation of PHQ-9 with both SF-12 MCS and VR-12 MCS at the 6-week postoperative timepoint. PHQ-9, Patient Health Questionnaire-9; SF-12 MCS, 12-item Short Form Health Survey mental composite score; VR-12 MCS, Veterans RAND 12-item health survey mental composite score.

Fig.┬Ā4.
Correlation of PHQ-9 with both SF-12 MCS and VR-12 MCS at the 12-week postoperative timepoint. PHQ-9, Patient Health Questionnaire-9; SF-12 MCS, 12-item Short Form Health Survey mental composite score; VR-12 MCS, Veterans RAND 12-item health survey mental composite score.
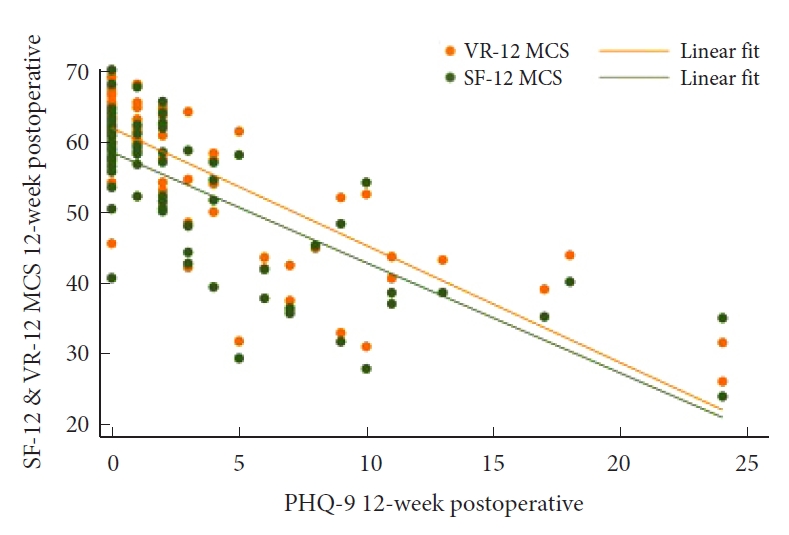
Fig.┬Ā5.
Correlation of PHQ-9 with both SF-12 MCS and VR-12 MCS at the 6-month postoperative timepoint. PHQ-9, Patient Health Questionnaire-9; SF-12 MCS, 12-item Short Form health survey mental composite score; VR-12 MCS, Veterans RAND 12-item health survey mental composite score.

Fig.┬Ā6.
Correlation of PHQ-9 with both SF-12 MCS and VR-12 MCS at the 1-year postoperative timepoint. PHQ-9, Patient Health Questionnaire-9; SF-12 MCS, 12-item Short Form Health Survey mental composite score; VR-12 MCS, Veterans RAND 12-item health survey mental composite score.
Table┬Ā1.
Baseline characteristics of study population
Table┬Ā2.
Postoperative changes in survey scores
| Variable | Score | Change | p-valueŌĆĀ | |
|---|---|---|---|---|
| PHQ-9 | ||||
| ŌĆā | Preoperative | 6.7 ┬▒ 6.0 (239) | - | - |
| 6 Weeks | 3.6 ┬▒ 4.8 (177) | -3.2 ┬▒ 5.3 (177) | < 0.001* | |
| 12 Weeks | 3.8 ┬▒ 5.5 (101) | -3.0 ┬▒ 5.8 (101) | < 0.001* | |
| 6 Months | 3.8 ┬▒ 5.0 (82) | -3.5 ┬▒ 4.9 (82) | < 0.001* | |
| 1 Year | 4.1 ┬▒ 6.1 (51) | -3.6 ┬▒ 6.8 (51) | < 0.001* | |
| SF-12 MCS | ||||
| Preoperative | 47.9 ┬▒ 11.2 (239) | - | - | |
| 6 Weeks | 53.3 ┬▒ 10.0 (166) | 5.3 ┬▒ 11.0 (166) | < 0.001* | |
| 12 Weeks | 53.8 ┬▒ 10.3 (90) | 5.6 ┬▒ 11.3 (90) | < 0.001* | |
| 6 Months | 53.6 ┬▒ 9.1 (72) | 7.0 ┬▒ 11.0 (72) | < 0.001* | |
| 1 Year | 51.5 ┬▒ 11.2 (49) | 5.9 ┬▒ 12.8 (49) | < 0.001* | |
| VR-12 MCS | ||||
| Preoperative | 50.0 ┬▒ 10.5 (239) | - | - | |
| 6 Weeks | 56.0 ┬▒ 10.2 (166) | 6.0 ┬▒ 10.1 (166) | < 0.001* | |
| 12 Weeks | 57.0 ┬▒ 10.4 (90) | 6.5 ┬▒ 11.1 (90) | < 0.001* | |
| 6 Months | 56.6 ┬▒ 10.0 (72) | 7.3 ┬▒ 10.4 (72) | < 0.001* | |
| 1 Year | 54.4 ┬▒ 12.9 (49) | 6.5 ┬▒ 13.2 (49) | 0.001* | |
Table┬Ā3.
Correlation of PHQ-9 with SF-12 and VR-12 MCS for MIS lumbar discectomy
| Variable | Pearson, r | p-valueŌĆĀ | Partial, r | p-valueŌĆĪ | |
|---|---|---|---|---|---|
| PHQ-9 vs. SF-12 MCS | |||||
| ŌĆā | Preoperative | -0.647 | < 0.001* | -0.658 | < 0.001* |
| 6 Weeks | -0.728 | < 0.001* | -0.734 | < 0.001* | |
| 12 Weeks | -0.761 | < 0.001* | -0.765 | < 0.001* | |
| 6 Months | -0.756 | < 0.001* | -0.755 | < 0.001* | |
| 1 Year | -0.898 | < 0.001* | -0.898 | < 0.001* | |
| PHQ-9 vs. VR-12 MCS | |||||
| Preoperative | -0.702 | < 0.001* | -0.778 | < 0.001* | |
| 6 Weeks | -0.776 | < 0.001* | -0.778 | < 0.001* | |
| 12 Weeks | -0.796 | < 0.001* | -0.802 | < 0.001* | |
| 6 Months | -0.842 | < 0.001* | -0.842 | < 0.001* | |
| 1 Year | -0.909 | < 0.001* | -0.908 | < 0.001* | |
Table┬Ā4.
Discriminant validity of PHQ-9
| PHQ-9 | Not depressedŌĆĀ SF-12 MCS Ōēź41.4 | DepressedŌĆĀ SF-12 MCS <41.4 | p-valueŌĆĪ |
|---|---|---|---|
| Preoperative | 4.3 ┬▒ 4.2 (171) | 11.5 ┬▒ 6.3 (68) | < 0.001* |
| 6 Weeks | 2.1 ┬▒ 3.0 (129) | 11.3 ┬▒ 5.9 (25) | < 0.001* |
| 12 Weeks | 1.4 ┬▒ 2.2 (67) | 10.8 ┬▒ 6.9 (16) | < 0.001* |
| 6 Months | 2.3 ┬▒ 3.4 (56) | 10.4 ┬▒ 5.9 (10) | < 0.001* |
| 1 Year | 1.8 ┬▒ 2.9 (33) | 12.9 ┬▒ 6.7 (9) | < 0.001* |
Values are presented as mean┬▒standard deviation (number).
PHQ-9, Patient Health Questionnaire-9; SF-12 MCS, 12-item Short Form health survey mental composite score.
ŌĆĀ Threshold for depression was set using an SF-12 MCS value reported by Vilagut et al. [17]
REFERENCES
1. Brody DJ, Pratt LA, Hughes JP. Prevalence of depression among adults aged 20 and over: United States, 2013-2016. NCHS Data Brief 2018 (303):1-8.
2. Polatin PB, Kinney RK, Gatchel RJ, et al. Psychiatric illness and chronic low-back pain. The mind and the spine--which goes first? Spine 1993 18:66-71.


3. Menendez ME, Neuhaus V, Bot AGJ, et al. Psychiatric disorders and major spine surgery: epidemiology and perioperative outcomes. Spine 2014 39:E111-22.


4. Miller JA, Derakhshan A, Lubelski D, et al. The impact of preoperative depression on quality of life outcomes after lumbar surgery. Spine J 2015 15:58-64.


5. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001 16:606-13.



6. Inoue T, Tanaka T, Nakagawa S, et al. Utility and limitations of PHQ-9 in a clinic specializing in psychiatric care. BMC Psychiatry 2012 12:73.



7. Mulvaney-Day N, Marshall T, Downey Piscopo K, et al. Screening for behavioral health conditions in primary care settings: a systematic review of the literature. J Gen Intern Med 2018 33:335-46.


8. Tuck AN, Scribani MB, Grainger SD, et al. The 9-Item Patient Health Questionnaire (PHQ-9): an aid to assessment of patient-reported functional outcomes after spinal surgery. Spine J 2018 18:1398-405.


9. Patel DV, Yoo JS, Khechen B, et al. PHQ-9 score predicts postoperative outcomes following minimally invasive transforaminal lumbar interbody fusion. Clin Spine Surg 2019 32:444-8.


10. Parrish JM, Jenkins NW, Nolte MT, et al. A validation of Patient Health Questionnaire-9 for cervical spine surgery. Spine (Phila Pa 1976) 2020 45:1668-75.


11. Jenkins NW, Parrish JM, Brundage TS, et al. Validity of Patient Health Questionnaire-9 in minimally invasive lumbar interbody fusion. Spine 2020 45:E663-9.


12. Benzakour A, Benzakour T. Lumbar disc herniation: longterm outcomes after mini-open discectomy. Int Orthop 2019 43:869-74.


13. Kanno H, Aizawa T, Hahimoto K, et al. Minimally invasive discectomy for lumbar disc herniation: current concepts, surgical techniques, and outcomes. Int Orthop 2019 43:917-22.


14. Chaichana KL, Mukherjee D, Adogwa O, et al. Correlation of preoperative depression and somatic perception scales with postoperative disability and quality of life after lumbar discectomy. J Neurosurg Spine 2011 14:261-7.


15. Hayes CJ, Bhandari NR, Kathe N, et al. Reliability and validity of the medical outcomes study Short Form-12 version 2 (SF-12v2) in adults with non-cancer pain. Healthcare (Basel) 2017 5:22.



16. Huo T, Guo Y, Shenkman E, et al. Assessing the reliability of the short form 12 (SF-12) health survey in adults with mental health conditions: a report from the wellness incentive and navigation (WIN) study. Health Qual Life Outcomes 2018 16:34.



17. Vilagut G, Forero CG, Pinto-Meza A, et al. The mental component of the short-form 12 health survey (SF-12) as a measure of depressive disorders in the general population: results with three alternative scoring methods. Value Health 2013 16:564-73.


18. Luo X, George ML, Kakouras I, et al. Reliability, validity, and responsiveness of the short form 12-item survey (SF-12) in patients with back pain. Spine 2003 28:1739-45.


19. Zieger M, Schwarz R, K├Čnig HH, et al. Depression and anxiety in patients undergoing herniated disc surgery: relevant but underresearched - a systematic review. Cent Eur Neurosurg 2010 71:26-34.


20. Lebow R, Parker SL, Adogwa O, et al. Microdiscectomy improves pain-associated depression, somatic anxiety, and mental well-being in patients with herniated lumbar disc. Neurosurgery 2012 70:306. -11. discussion 311.


21. Jacobs WCH, van Tulder M, Arts M, et al. Surgery versus conservative management of sciatica due to a lumbar herniated disc: a systematic review. Eur Spine J 2011 20:513-22.


22. Mobbs RJ, Phan K, Malham G, et al. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg 2015 1:2-18.


23. Faldini C, Pagkrati S, Acri F, et al. Surgical treatment of symptomatic degenerative lumbar spondylolisthesis by decompression and instrumented fusion. J Orthop Traumatol 2007 8:128-33.


24. Gornet MF, Copay AG, Sorensen KM, et al. Assessment of health-related quality of life in spine treatment: conversion from SF-36 to VR-12. Spine J 2018 18:1292-7.