- Search
| Neurospine > Volume 18(4); 2021 > Article |
|
|
Abstract
Objective
The purpose of this study is to find the clinical and radiographic characteristics of traumatic craniocervical junction (CCJ) injuries requiring occipitocervical fusion (OC fusion) for early diagnosis and surgical intervention.
Methods
We retrospectively reviewed 12 patients with CCJ injuries presenting to St. Michaels Hospital in Toronto who underwent OC fusion and looked into the following variables; (1) initial trauma data on emergency room arrival, (2) associated injuries, (3) imaging characteristics of computed tomography (CT) scan and magnetic resonance imaging (MRI), (4) surgical procedures, surgical complications, and neurological outcome.
Results
All patients were treated as acute spinal injuries and underwent OC fusion on an emergency basis. Patients consisted of 10 males and 2 females with an average age of 47 years (range, 18–82 years). All patients sustained high-energy injuries. Three patients out of 6 patients with normal BAI (basion-axial interval) and BDI (basion-dens interval) values showed visible CCJ injuries on CT scans. However, the remaining 3 patients had no clear evidence of occipitoatlantal instability on CT scans. MRI clearly described several findings indicating occipitoatlantal instability. The 8 patients with normal values of ADI (atlantodens interval interval) demonstrated atlantoaxial instability on CT scan, however, all MRI more clearly and reliably demonstrated C1/2 facet injury and/or cruciate ligament injury.
Although advances in universal spine precautions and spine stabilization techniques have increased the number of patients surviving acute traumatic instability at the craniocervical junction (CCJ), a delay in diagnosis and mismanagement in the Emergency Department (ED) can have potentially devastating consequences [1]. Unfortunately, an accurate diagnosis is frequently not established at the time of initial evaluation because altered level of consciousness of patients due to the presence of head injury and multiple other life-threatening injuries could complicate the process of diagnosis [2]. Furthermore, difficulty and inexperience in radiological analysis of CCJ anatomical relationships is another possible cause for misdiagnosis [2]. Therefore, clarification of specific characteristics of trauma and imaging clues suggestive of CCJ injuries is extremely important to raise awareness for this pathology. The advent of magnetic resonance imaging (MRI) revolutionized the assessment of traumatic CCJ injuries by providing unique and accurate information about the integrity of the CCJ ligaments, based on which surgical indication could be determined [3].
The purpose of this study is to find the clinical and radiographic characteristics of traumatic CCJ injuries requiring occipitocervical fusion (OC fusion) for early diagnosis and surgical intervention.
We conducted a retrospective study of traumatic CCJ injury cases who required OC fusion at St. Michael’s Hospital in Toronto, from 2013 to 2018. All of these cases were preoperatively diagnosed with occipitoatlantal instability on computed tomography (CT) scan and MRI with radiological findings as follows; fracture dislocation and/or disruption of ligaments in the occipitoatlantal segment. Traumatic CCJ injuries requiring only C1–2 fusion were excluded. Following institutional review board approval, 12 consecutive cases were identified. All medical records and spinal imaging studies were retrospectively reviewed to identify the following variables: (1) initial trauma data on ED arrival, (2) associated injuries, (3) imaging characteristics of CT scan and MRI, (4) surgical procedures, surgical complications, and neurological outcome. Based on these data, key points leading to early identification of surgical candidates and surgical outcomes are investigated.
On arrival at St. Michael’s Hospital, patients were evaluated according to standard Advanced Trauma Life Support protocol [4]. A cross-table lateral conventional radiograph of the spine was obtained as part of the initial trauma evaluation. Head and cervical CT scans (occiput-T3) were routinely obtained in all patients because of the high-energy mechanism of their injuries. Some patients had been seen at outside hospitals for triage and were re-evaluated as acute trauma patients in the aforementioned manner after transfer to St. Michael’s Hospital. Once traumatic CCJ injury was identified or suspected, patients were kept on spinal precautions and provisional stabilization secured by a rigid cervical collar or halo vest. Cervical spine MRI was then performed to evaluate the presence of hematoma, ligamentous disruption, facet injury, intervertebral disc injury, and spinal cord injury (SCI).
All cases underwent rigid OC fusion using occipital plates, rods, and screws as soon as the physiological general conditions of patients permitted and prepared for surgery. Surgical procedure was conducted in the operating room in the following sequence. We achieved a fiberoptic awake intubation in the supine position and checked the patient’s neurological status to confirm no neurological deterioration was caused by the intubation. The patient was then placed in the spine position on a spinal surgery operating table (Jackson Table; OSI, Union City, CA). At this point, we performed closed reduction and adjustment of cervical alignment under fluoroscopic guidance with great care before the patient was rotated 180°. Rigid titanium screws, rods, and plate devices (Stryker Spine, Allendale, NJ, USA) were used to fixate the affected segments with 3-dimensional navigation (Stryker Spine, Allendale, NJ, USA) or fluoroscopic guidance (Ziehm Vision FD vario 3D, Ziehm Imaging, Nuremburg, Germany). Arthrodesis was undertaken by putting local bone from spinous processes of the affected levels on the decorticated laminae and facet joints.
Postoperative external immobilization was achieved with a cervical brace. Postoperative cervical CT scans and radiographs were obtained to assess spinal alignment and the adequacy of screws and plates locations. After discharge, radiographic and clinical follow-up data were obtained at the outpatient clinic. Upright flexion-extension lateral radiograph was evaluated for assessment of spinal alignment in all patients on a periodic basis.
Table 1 provides a summary of initial trauma assessment data acquired in emergency room. All patients were treated as acute spinal injuries and underwent OC fusion on an emergency basis. Patients consisted of 10 males and 2 females with an average age of 47 years (range, 18–82 years). In all cases, the patients sustained high-energy injuries, such as motor vehicle collision (MVC) with ejection (4 patients) or without ejection (3 patients), fall from height (3 patients), or assault (2 patients). Eight patients exhibited transient or protracted loss of consciousness at the scene and reduced Glasgow coma scale (GCS) was noted in 7 cases on ED arrival including 3 cases of severely impaired consciousness (GCS 3 and 6).
Associated injuries were summarized in Table 2. Six cases with closed head injury (CHI) were noted on head CT scan. While only 1 case underwent emergency craniotomy, 5 other cases with CHI were treated conservatively. Seven cases sustained scalp injury or facial fracture, or facial laceration. Subaxial cervical spine injuries were detected in 5 cases, while thoracic or lumbar spine injury was seen in only 1 case. Carotid or vertebral artery injuries were found in 3 cases (1 case had coexisting carotid and vertebral artery injuries). Antiplatelet therapy was initiated following the surgical procedure and maintained throughout the acute critical management in all cases.
The abnormal imaging findings that suggested the presence of traumatic CCJ injury are summarized in Table 3. Head and cervical spine CT scans (Occipital bone to T3) was obtained in all patients because of the high-energy mechanism of their injuries after patients were optimized hemodynamically. All but 1 case (case 1) underwent both of cervical spine CT scan and MRI. Case 1 was in a state of deep coma with unilateral blown pupil due to CHI (GCS 3) on arrival and emergency decompressive craniectomy and OC fusion was performed without obtaining MRI. Bony displacement and malalignment were measured and reported in all patients on CT scans. Overall, 6 patients (cases 1, 5, 7, 8, 10, 11) had values of basion-axial interval (BAI; normal < 12 mm) and/or basion-dens interval (BDI; normal < 10 mm) outside of normal limits and 4 patients (cases 1, 8, 10, 12) showed abnormal values of atlanto-dens interval (ADI; normal < 3 mm), respectively. Three patients (cases 2, 3, 9) out of 6 patients (cases 2, 3, 4, 6, 9, 12) with normal BAI and BDI values showed visible occipitoatlantal facet joint dislocation or diastasis based on CT scans. However, the remaining 3 patients (cases 4, 6, 12) had no clear evidence of occipitoatlantal instability on CT scans. MRI clearly described several findings indicating occipitoatlantal instability, such as anterior longitudinal ligament injury, cruciate ligament injury, or occipitoatlantal facet injury. The 8 patients (cases 2, 3, 4, 5, 6, 7, 9, 11) with normal values of ADI demonstrated atlantoaxial malalignment and facet diastasis on CT scan and a diagnosis of atlantoaxial instability was established on CT scans. However, all MRI more clearly and reliably demonstrated C1/2 facet injury and/or cruciate ligament injury. No patient had an isolated occipitoatlantal dislocation without atlantoaxial instability.
There were no cases of occipitocervical and occipitothroacic pseudoarthrosis or hardware failure. A postoperative surgical site infection occurred in 1 patient (case 5), who was successfully treated with irrigation and debridement, revision of hardware, and antibiotic agents. One patient (case 7) was complicated by postoperative deep venous thrombosis, which was also successfully treated with anticoagulation therapy. Another patient (case 11) who developed hydrocephalus following CHI received ventriculoperitoneal shunt successfully. The mean follow-up duration was 12 months (range, 6–24 months). No patients experienced worsening of neurological symptoms postoperatively. Seven patients (58%) exhibited normal neurological functions (American Spinal Injury Association impairment scale [AIS] grade E) and 5 (42%) suffered incomplete SCI preoperatively. The severity of SCI was AIS grade C (3 patients) and AIS grade D (2 patients). All SCI patients (AIS grade C–D) made improvement by at least one AIS grade postoperatively (Tables 4, 5).
The patient was an 18-year-old man who was involved in an MVC. He was initially taken to an outside hospital and subsequently transferred to St. Michael's Hospital. There was no loss of consciousness. Head CT and CT angiography showed no evidence of CHI or craniocervical vessel injury. He was found to have right lung pneumothorax and a nondisplaced mandible fracture, both of which were managed conservatively. He had avulsion fractures of anterior arch of C1 with widening of the BAI and BDI. There was posterior widening of the occipitoatlantal facet joints and atlantoaxial facet joints (Fig. 1A, B). Cervical spine MRI showed severe injury of ALL, the tectorial membrane, and cruciate ligament (Fig. 1C) with apparent distraction of the occipitoatlantal and atlantoaxial facet joints with interfacet fluid signal (Fig. 1D). Preoperative diagnosis was occipitoatlantal and atlantoaxial instability with C1 fracture. OC3 fusion was performed (Fig. 1E), however, he developed surgical site infection, which was successfully cured by wound reopening, irrigation, and debridement. He made significant recovery without any neurological symptoms at follow-up in the outpatient clinic.
The difficulties in prompt diagnosis of traumatic CCJ injury were highlighted and recognized over the past decade [1,5-11]. As mortality rates are reportedly extremely low in patients who are correctly diagnosed with CCJ injury on initial trauma evaluation [12-14], we need to identify the characteristics of the trauma and imaging clues serving as warning signs for CCJ injury at the initial trauma assessment. In the present study, all patients were involved in high-energy injuries mainly affecting head and face. Eight patients had transient or protracted loss of consciousness on arrival, indicating severe blow to the brain. Closed head injuries were present in 6 patients (50%) and impaired consciousness with reduced GCS was noticed in 6 cases (50%). Altered level of consciousness due to brain injury, hemodynamic instability, or alcoholic consumption as well as severe pain that distracts from traumatic CCJ injuries contributed to diagnostic difficulties. We also found high rate of scalp or facial injuries, which are suggestive of CCJ injury. Spinal cord deficits were identified in 5 patients on initial evaluation (42%) in the present study; which were AIS grade C or D deficits. Neurological symptoms caused by SCI could facilitate the identification of CCJ injury.
In recent years, the preference of initial imaging has shifted from x-ray to CT scans, since CCJ injuries are often overlooked in x-ray imaging [15]. The analysis of the present study demonstrated generally accepted indexes (BAI, BDI, and ADI) on CT scans were not reliable enough and other CT scan findings such as facet diastasis and facet dislocation were particularly useful findings. Facet diastasis and facet dislocation are closely related to the damage of ligaments [15,16]. Several important ligaments hold bony structures and facet joints in the CCJ, including the cruciate ligament, the paired alar ligaments, the tectorial membrane, the apical ligament, and the anterior and posterior atlantooccipital membranes [17-19]. Although these ligaments play pivotal roles for stabilization, traumatic CCJ injuries have historically been recognized as osseous fractures [20,21]. Ligamentous injuries at the CCJ can cause bony dislocations and facet diastasis leading to severe and insidious instability without associated fractures. We encountered several cases with obvious bony dislocations and facet diastasis on CT scans, however, we should emphasize the existence of cases with the ligamentous injuries without clear evidence of osseous displacements on CT scans. Atlantoaxial instability could be made diagnosis solely by detailed analysis of CT scans based on facet dislocations and facet diastasis even with normal values of ADI though the diagnosis should be confirmed using MRI, which more clearly and reliably demonstrated atlantoaxial facet injury and/or cruciate ligament injury. On the other hand, several reports emphasized the existence of trauma patients of occipitoatlantal instability with normal or near-normal CT scans, which were narrowly diagnosed on MRI [22,23]. It is extremely difficult to detect occipitoatlantal instability solely by CT scans in patients who demonstrate normal values of the BAI, BDI with no clear evidence of occipitoatlantal malalignment or diastasis of the occipitoatlantal facet. These clear differences in the process of diagnosis between occipitoatlantal and atlantoaxial instability may come from the differences of function and range of motion between these facet joints. Atlantoaxial facet joints are structurally more complicated and more mobile with wide range of axial rotation (48.53° on average) than occipitoatlantal facet joints with flexion-extension motion (18.7° on average) [24]. Therefore, diastasis of the occipitoatlantal facet joints occurring after traumatic CCJ injury may be more likely to spontaneously reduce with normal joint heights even as the patient has significant occipitoatlantal instability. Therefore, CT measurements alone can overlook purely ligamentous injuries, and additional MRI analysis is essential particularly in occipitoatlantal instability. This is especially true of unconscious patients who cannot complain of any subjective symptoms and cannot take neurological assessment [25,26]. The present study showed occipitoatlantal injury was accompanied by concomitant atlantoaxial injury even as isolated atlantoaxial injury is frequently observed [20]. This unique traumatic relationship was clearly verified by MRI assessment. In this context, the possible coexistence of occipitoaxial instability should be born in mind once atlantoaxial dislocation is suspected. MRI is currently an integral part of diagnostic process in CCJ injuries, however, Dyas et al. [27] indicated the disruption of alar ligaments, one of the main ligamentous stabilizers in CCJ, was difficult to be recognized on MRI. The whole ligamentous structure of CCJ needs to be evaluated because identification of individual ligament may be difficult. The ability of MRI to detect the integrity of the ligaments is not always perfect depending on the imaging quality of MRI [27,28], therefore comprehensive assessment of mechanism of injury, associated injury, neurological symptoms, and consciousness status is essential to accurately reach the diagnosis.
Rigid cervical orthosis or halo immobilization should be continued until the patient is prepared for surgical intervention. The most appropriate preoperative provisional stabilization has to be decided considering the timing of surgery, the degree of instability, and the patient’s general condition, neurological status, and other spine injuries. Traumatic CCJ injury mainly comprises ligamentous disruption and could lead to significant neurological deterioration without surgical intervention [29]. Posterior OC fusion is the treatment of choice in most cases [30] and the development of plate, rod, and screw system has allowed us to attain successful outcomes without the need for postoperative halo immobilization [31,32] with high bony fusion rate of more than 90% [31].
In summary, as CCJ stability is largely dependent on ligamentous integrity [33,34], MRI has greater sensitivity for detecting CCJ instability by analysis of disc disruption, facet injuries, and ligament injuries than CT scans or x-ray alone [1] and the addition of MRI to CT scans can alter patient management [25,35-37]. The classification system where MRI findings are fully integrated needs to be developed particularly for occipitoatlantal instability.
We advocate measures to help recognize CCJ injury at an early stage in the present study. Firstly, these measures have put emphasis on the identification of clinical clues (high-energy trauma, transient or protracted loss of consciousness, reduced consciousness level, CHI, scalp, or facial injury). Secondly, careful imaging assessment is necessary based on both CT scan and MRI. Occipitoatlantal instability is carefully investigated on MRI in addition to CT scan with special attention to facet joint and ligament integrity. OC fusion using occipital plate, rod, and screws in a timely manner brings great outcomes. We found that following these measures give great chances to functionally improve even patients with severe neurological symptoms. More cases with CCJ injury are needed to be accumulated to investigate and establish correct diagnostic criteria for CCJ instability.
Fig. 1.
(Case 5) Preoperative computed tomography scan (A, B), preoperative magnetic resonance imaging (C, D), postoperative x-ray (E). Avulsion fractures of anterior arch of atlas with widening of BDI (A; arrow), cephalad displacement of atlas (A; arrowhead), malalignment of the atlantooccipital joints with posterior widening of the O/C1 facet joints (B; arrow) and C1/2 facet joints. Severe injury of anterior longitudinal ligament and anterior atlantooccipital membrane (C; arrow), tectorial membrane and cruciate ligaments (C; arrowhead). There was apparent distraction of the O/C1 (D; arrow) and C1/2 facet joints with interfacet fluid signal. OC3 fusion was successfully performed (E).
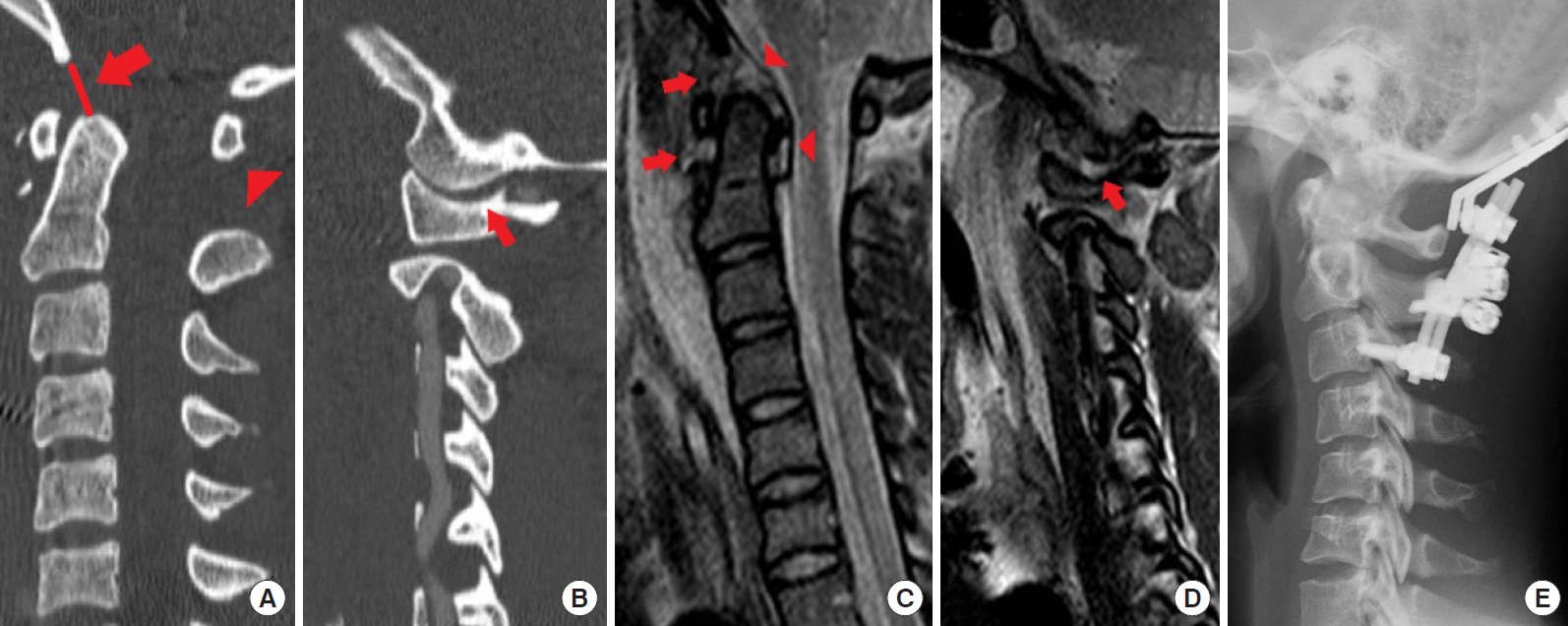
Table 1.
Summary of initial trauma data
| Variable | Value |
|---|---|
| Sex, male:female | 9:3 |
| Age (yr), mean (range) | 47 (18–82) |
| Injury mechanism | |
| MVC | 7 |
| Fall down | 3 |
| Assault | 2 |
| Ejection from vehicle | |
| Yes | 4 |
| No | 3 |
| NA | 5 |
| GCS score, mean ± SD | 11.6 ± 1.3 |
| LOC | |
| Yes | 8 |
| No | 4 |
Table 2.
Summary of associated injuries
Table 3.
Imaging characteristics of CT scan and MRI
Table 4.
Surgical procedures and surgical complications
REFERENCES
1. Bellabarba C, Mirza SK, West GA, et al. Diagnosis and treatment of craniocervical dislocation in a series of 17 consecutive survivors during an 8-year period. J Neurosurg Spine 2006 4:429-40.


2. DiBenedetto T, Lee CK. Traumatic atlanto-occipital instability. A case report with follow-up and a new diagnostic technique. Spine 1990 15:595-7.


3. Nidecker AE, Shen PY. Magnetic resonance imaging of the craniovertebral junction ligaments: normal anatomy and traumatic injury. J Neurol Surg B Skull Base 2016 77:388-95.



4. Ali J, Howard M. The Advanced Trauma Life Support course for senior medical students. Can J Surg 1992 35:541-5.

5. Martinez-Del-Campo E, Kalb S, Soriano-Baron H, et al. Computed tomography parameters for atlantooccipital dislocation in adult patients: the occipital condyle-C1 interval. J Neurosurg Spine 2016 24:535-45.


6. Fisher CG, Sun JC, Dvorak M. Recognition and management of atlanto-occipital dislocation: improving survival from an often fatal condition. Can J Surg 2001 44:412-20.


7. Gerrelts BD, Petersen EU, Mabry J, et al. Delayed diagnosis of cervical spine injuries. J Trauma 1991 31:1622-6.


8. Jonsson H Jr, Bring G, Rauschning W, et al. Hidden cervical spine injuries in traffic accident victims with skull fractures. J Spinal Disord 1991 4:251-63.


9. Bucholz RW, Burkhead WZ. The pathological anatomy of fatal atlanto-occipital dislocations. J Bone Joint Surg Am 1979 61:248-50.


10. Chan RN, Ainscow D, Sikorski JM. Diagnostic failures in the multiple injured. J Trauma 1980 20:684-7.


11. Davis JW, Phreaner DL, Hoyt DB, et al. The etiology of missed cervical spine injuries. J Trauma 1993 34:342-6.


12. Mendenhall SK, Sivaganesan A, Mistry A, et al. Traumatic atlantooccipital dislocation: comprehensive assessment of mortality, neurologic improvement, and patient-reported outcomes at a Level 1 trauma center over 15 years. Spine J 2015 15:2385-95.


13. Guigui P, Milaire M, Morvan G, et al. Traumatic atlantooccipital dislocation with survival: case report and review of the literature. Eur Spine J 1995 4:242-7.


14. Horn EM, Feiz-Erfan I, Lekovic GP, et al. Survivors of occipitoatlantal dislocation injuries: imaging and clinical correlates. J Neurosurg Spine 2007 6:113-20.


15. Jung MK, Hörnig L, Stübs MMA, et al. Analysis of diagnostics, therapy and outcome of patients with traumatic atlantooccipital dislocation. Spine J 2021 21:1513-9.


16. Campo EMD, Kalb S, Baron HS, et al. Computed tomography parameters for atlantooccipital dislocation in adult patients: the occipital condyle-C1 interval. J Neurosurg Spine 2016 24:535-45.


17. Tubbs RS, Hallock JD, Radcliff V, et al. Ligaments of the craniocervical junction. J Neurosurg Spine 2011 14:697-709.


18. Havrda JB, Paterson E. Imaging atlantooccipital and atlantoaxial traumatic injuries. Radiol Technol 2017 89:27-41.

19. Dickman CA, Sonntag VK. Injuries involving the transverse atlantal ligament: classification and treatment guidelines based upon experience with 39 injuries. Neurosurgery 1996 38:44-50.


20. Radcliff K, Kepler C, Reitman C, et al. CT and MRI-based diagnosis of craniocervical dislocations: the role of the occipitoatlantal ligament. Clin Orthop Relat Res 2012 470:1602-13.


21. Collalto PM, DeMuth WW, Schwentker EP, et al. Traumatic atlanto-occipital dislocation. Case report. J Neurosurg 1986 65:863-70.


22. Souslian FG, Patel PD, Elsherif MA. Atlanto-occipital dissociation in the setting of relatively normal radiologic findings. World Neurosurg 2020 143:405-11.


23. Tobert DG, Ferrone ML, Czuczman GJ. Traumatic atlantooccipital dissociation and atlantoaxial instability: concomitant ligamentous injuries without neurologic deficit: a case report. JBJS Case Connect 2018 8:e62.


24. Siccardi D, Buzzatti L, Marini M, et al. Analysis of three-dimensional facet joint displacement during two passive upper cervical mobilizations. Musculoskelet Sci Pract 2020 50:102218.


25. Roy AK, Miller BA, Holland CM, et al. Magnetic resonance imaging of traumatic injury to the craniovertebral junction: a case-based review. Neurosurg Focus 2015 38:E3.


26. Siddiqui J, Grover PJ, Makalanda HL, et al. The spectrum of traumatic injuries at the craniocervical junction: a review of imaging findings and management. Emerg Radiol 2017 24:377-85.


27. Dyas AR, Niemeier TE, Mcgwin G, et al. Ability of magnetic resonance imaging to accurately determine alar ligament integrity in patients with atlanto-occipital injuries. J Craniovertebr Junction Spine 2018 9:241-5.



28. Schmidt P, Mayer TE, Drescher R. Delineation of alar ligament: morphology: comparison of magnetic resonance imaging at 1.5 and 3 tesla. Orthopedics 2012 35:e1635-9.


29. Kasliwal MK, Fontes RB, Traynelis VC. Occipitocervical dissociation-incidence, evaluation, and treatment. Curr Rev Musculoskelet Med 2016 9:247-54.



30. Theodore N, Aarabi B, Dhall SS, et al. The diagnosis and management of traumatic atlanto-occipital dislocation injuries. Neurosurgery 2013 72 Suppl 2:114-26.


31. Garrido BJ, Puschak TJ, Anderson PA, et al. Occipitocervical fusion using contoured rods and medial offset connectors: description of a new technique. Orthopedics Oct;2009 32(10):orthosupersite.com/view.asp?rID=43769. https://doi.org/10.3928/01477447-20090818-11.

32. Lu DC, Roeser AC, Mummaneni VP, et al. Nuances of occipitocervical fixation. Neurosurgery 2010 66(3 Suppl):141-6.


33. Debernardi A, D'Aliberti G, Talamonti G, et al. The craniovertebral junction area and the role of the ligaments and membranes. Neurosurgery 2015 76 Suppl 1:S22-32.


34. Debernardi A, D’Aliberti G, Talamonti G, et al. Traumatic injuries to the craniovertebral junction: a review of rare events. Neurosurg Rev 2014 37:203-16.


35. Menaker J, Stein DM, Philp AS, et al. 40-slice multidetector CT: is MRI still necessary for cervical spine clearance after blunt trauma? Am Surg 2010 76:157-63.