- Search
| Neurospine > Volume 19(2); 2022 > Article |
|
|
Abstract
Objective
By using angulation of the axis itself, this study aims to define and analyze odontoid incidence (OI) and odontoid tilt (OT) as novel cervical alignment parameters and investigate their correlations with cervical alignment.
Methods
Novel and existing parameters were measured with whole-spine lateral plain radiographs and EOS images of 42 adults without cervical symptoms. The correlations of OI, OT, C2 slope (C2S), and T1 slope (T1S) were calculated.
Results
The OI, OT, and C2S showed significant correlations with C2–7 angle (r = 0.43, r = -0.42, r = 0.62, respectively) and C0–2 angle (r = -0.33, r = 0.48, r = -0.61, respectively). OI, OT, T1S were independent predictors of the C2–7 angle in univariate regression analysis (adjusted-R2 = 0.17, R2 = 0.15, R2 = 0.28, respectively). OI, OT, and T1S were independent predictors in the multivariable regression analysis with estimated standardized coefficients of 0.36, -0.67, -0.69, respectively (adjusted- R2 = 0.80, p < 0.001). Regarding the C0–2 angle, OI and OT were independent predictors in the univariate regression analysis (adjusted-R2 = 0.08, R2 = 0.21, respectively).
Conclusion
OI, OT, and C2S had significant correlations with cervical alignment. As the pelvic incidence, the OI is the only anatomical and constant parameter that could be used as a reference point related to the cervical spine from the rostral end. The study results may serve as baseline data for further studies on the alignment and balance of the cervical spine.
The cervical spine is dynamic in nature. Recent investigations have shown that the cervical alignment is affected by global sagittal alignment through compensatory mechanisms that maintain an upright posture and horizontal gaze [1-5]. Accordingly, the cervical parameters currently used are mostly positional variables, not constant parameters [6,7].
The compensatory mechanisms within the cervical spine are well established and have been proven by numerous studies. Kyphotic alignment of the subaxial cervical spine (C2–7) is compensated by a lordotic upper cervical spine (C0–2) and vice versa [6,8-10]. The C2 endplate (C2EP) is the border dividing the subaxial and upper cervical spine. It has long been speculated that the morphology of the odontoid process is somehow related to the sagittal alignment of the cervical spine [11-13]. However, no studies have been able to show a significant correlation [11,12]. On the basis of these studies, we postulated that the axis (C2 vertebra) acts as the base of the subaxial and upper cervical spine, and physiological sagittal alignment is based on its orientation and structural geometry.
A novel cervical parameter termed odontoid incidence (OI), which is a constant parameter, is proposed in this study as a critical factor regulating the sagittal alignment of the cervical spine. To the best of our knowledge, no studies have reported correlations between the structural geometry of the C2EP, the odontoid process, and the sagittal alignment of the cervical spine. The study aimed to analyze the relationship between the structural geometry of the odontoid process and the sagittal alignment of the cervical spine and to present these parameters from a different perspective that would aid in predicting physiological cervical lordosis (CL) in asymptomatic populations.
A retrospective analysis of clinical and radiographic data was performed after obtaining Institutional Review Board approval of Seoul National University Bundang Hospital, Seoul National University College of Medicine for the study (B-2111-723-102). From 2016 to 2020, 42 asymptomatic subjects (aged between 15 and 68 years old) without cervical symptoms including neck pain or radiculopathy were enrolled. Subjects were asymptomatic spinal subjects whom underwent spinal work up during a comprehensive health screening. We excluded individuals with diagnosed conditions, degenerative changes including decreased disc height or osteophyte formation, and treatment related to the cervical spine; a history of spinal surgery; and abnormal global sagittal alignment. Whole-spine lateral plain radiographs and EOS images were obtained with the subject in a comfortable upright position and an acceptable range of chin-brow vertical angle between -1.5° and 5.8° [14]. The scan was performed in a relaxed posture and the subjects were asked to look straight ahead.
OI was defined as the angle between the line perpendicular to the C2EP at its midpoint and the line connecting this point to the center of the odontoid process (the center of a circle with an anterior/posterior border and the apex of the dens as a tangent). Odontoid tilt (OT) was defined as the angle created by a line running from the C2EP midpoint to the center of the odontoid process and the vertical axis. C2 slope (C2S) was defined as the angle between the C2EP and a horizontal line (Fig. 1A). A geometric construction using complementary angles showed that OI is the algebraic sum of OT and C2S, similar to the formula stating that pelvic incidence (PI)= pelvic tilt (PT) + sacral slope (SS) (Fig. 1B, C) [15].
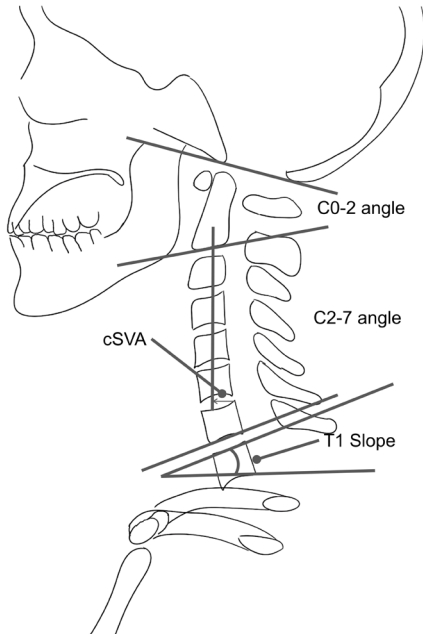
The Cobb angle at C0–2, C2–3, C2–4, C2–5, C2–6 C2–7, T1 slope (T1S), C2–7 sagittal vertical axis (cSVA), and T1S minus CL (C2–7) were measured. For the C0–2 angle, an angle between the C2EP and the McRae line was measured. T1S was defined as an angle formed between the T1 upper endplate and the horizontal plane. cSVA was defined as the distance between a plumb line from the centroid of C2 and the posterosuperior aspect of C7 (Fig. 2).
A picture archiving and communication system (p view, Infinitt, Seoul, Korea) was used for measurements. Test for normality was done using Shapiro-Wilk test. The correlations between the parameters were analyzed using Pearson correlation coefficients and univariable/multivariable linear regression analysis. The statistical analysis was conducted using the R&R Studio software (ver. 1.4.1717), and a p-value < 0.05 was considered to indicate statistical significance.
The mean values and the standard deviations for the studied parameters and subject demographics are reported in Table 1. No significant difference between male and female groups except cSVA and PI were noted. The odontoid parameters showed significant correlations with the established cervical parameters (Table 2). The OI showed significant correlations with the C0–2 angle (r= -0.33) and C2–7 angle (r= 0.43), but not with cSVA or T1S. The OI had a significant correlation with C2S (r= 0.52), but not OT. However, OT was significantly correlated with all cervical parameters: C0–2 angle (r= 0.48, p< 0.001), C2–7 angle (r= -0.42, p< 0.01), cSVA (r= -0.57, p< 0.001), T1S (r= -0.32, p< 0.05), and T1S-CL (r= -0.78, p< 0.001). Strong correlations were found between pelvic parameters, but the odontoid parameters did not show significant correlations with global sagittal parameters (Table 2).
Using linear regression, the odontoid parameters were matched to established cervical parameters (Table 3). OT and C2S matched all cervical parameters. OI matched the C0-2 angle (r2= 0.08) and C2–7 angle (r2= 0.17). T1S matched C2–7 (r2= 0.28), T1S–CL (r2= 0.10), and cSVA (r2= 0.19).
Multivariable analysis was used to identify predictive variables for each cervical parameter (Table 4). The predictive formulas of the C2–7 angle, C0–2 angle, T1S–CL, and cSVA were established with stepwise regression analysis. OI, OT, and T1S were identified as 3 important predictive variables for the C2–7 angle: CL = 0.36 × OI – 0.67 × OT – 0.69 × T1S (r2= 0.79). OI, OT, and PT were important predictors of C0–2 angle: C0–2= -0.45 × OI+0.57 × OT – 0.28 × PT (r2= 0.40). OI, OT, and the C5–T3 angle were important factors for T1S-CL: T1S–CL = 0.42× OI – 0.83× OT – 0.19× C5–T3 angle (r2= 0.75). OT, C5–T3 angle, and TK were key factors for cSVA: cSVA= -0.43× OT + 0.34× C5-T3 angle+0.40× TK (r2= 0.51).
Since the first introduction of pelvic parameters, the sequential correlations of PI, PT, LL, and TK have been well documented [16]. Likewise, attempts have been made to discover novel measurement parameters correlating with cervical alignment over the last decade. Since the advent of thoracic inlet measurements, including T1S [17], multiple innovative radiographic parameters have been described. Despite these efforts, however, only T1S, T1S–CL, cSVA, and C2S have shown correlations with health-related quality of life (HRQoL) [6,18-22].
T1S has been suggested as the key to understanding CL [23]. It is an important factor influencing spinal alignment, and an increase in T1S leads to larger CL in order to maintain head balance [17,23-25]. Staub et al. [26] proposed that as PI can be used to determine the optimal LL, T1S can also be used to predict CL. Previous research has shown that patients with greater T1S are likely to have underlying thoracolumbar deformity [27]. However, T1S is not a constant parameter and can be influenced by aging or posture [17]. As cervical alignment is well known to be affected by global sagittal alignment through compensatory mechanisms [1-5,28], the positional variance of a patient makes it troublesome to determine the adequate CL.
Nevertheless, the T1S-CL has been proposed as a parameter analogous to PI–LL to better define cervical alignment [29,30]. As with PI and LL, the greater the T1S, the larger CL is necessary in order to balance the head for harmonious alignment [17,23,24,31]. Therefore, T1S–CL describes the compensation between the cervical alignment and upper thoracic alignment [19]. If there is insufficient CL to match a given T1S in a patient, C2 will tilt forward to increase C2S [19]. Additionally, C2S has been shown to correlate with patient-reported outcomes and with T1S–CL, C0–2 angle, cSVA, CL, and T1S [19,31].
Cervical alignment is influenced by global sagittal alignment through compensatory mechanisms [1-5,28]. But what limits the alignment in the rostral end? If the foundation is identical, is the ceiling predetermined? In the present study, we evaluated associations between odontoid and cervical parameters. The close relationship between the odontoid and cervical parameters is evident from the regression coefficients. All odontoid parameters showed significant correlations with the C0–2 and C2–7 angles (OI, r= 0.43; OT, r= -0.42; C2S, r= 0.62). The C0–2 and C2–7 angles are both closely related to the structural geometry and orientation of the axis, as the axis is at the base of the upper CL. OT showed a significant correlation with all cervical parameters, including T1S and T1S–CL (r= -0.32, r= -0.78, respectively). C2S did not show a correlation with T1S, unlike a previous study [19]. Significant interdependence was also noted between the odontoid parameters. The C2S, like the SS, is a horizontal parameter. OT, like the PT, denotes the spatial orientation of the dens, which may vary according to the balance of the cranium and horizontal gaze. Adding OT into the picture could aid in a 2-dimensional analysis of the cervical alignment and balance, with the OI as a fixed reference point.
Through multivariable regression analysis, predictive variables for CL based on odontoid parameters were postulated. Linear regression showed a significant correlation of CL with OI, OT, and T1S (r2= 0.80). Since the T1S regulates physiological CL, it can be assumed that the odontoid parameters determine CL from the top, modulating the ideal head position. T1S is a reflection of underlying thoracolumbar alignment, and T1S–CL is a result of the balance between cervical and thoracolumbar alignment [19]. C5–T3 has been proposed as an ideal parameter assessing the cervicothoracic junction [32]. The regression models demonstrated that T1S–CL (r2= 0.75) and cSVA (r2= 0.51) were strongly correlated not only with the odontoid parameters, but also with cervicothoracic alignment (C5–T3, cervicothoracic) as previously reported [19,32].
T1S–CL shows whether a patient has a harmonious cervical alignment regarding upper thoracic alignment, and C2S is a mathematical approximation of T1S–CL [19]. If the CL is insufficient to match a given T1S, the axis tilts forward, increasing C2S [19]. As C2S increases, the vertical axis from the center of the odontoid is placed anterior to C2EP, resulting in a negative OT value (Fig. 3). C2S increases, thereby causing a decrease in OT. Similarly, in adult spinal deformity patients, individuals attempt to compensate through pelvic retroversion, which causes an increase in PT and subsequent decrease in SS [33]. Protopsaltis et al. [19] showed that cervical deformity is present if T1S–CL exceeds 17°, similar to the average OI shown in the present study (17.7°). Although the authors did not report OI values in the study, the predicted OT value in cervical deformity patients is assumed to be below zero. In addition, modified cervical deformity classification concerning T1S–CL has been proposed [21]. Some tolerate a larger T1S–CL than others. 16 out of 42 subjects in the present study showed T1S–CL exceeding 15°. As OI is the sum of OT and C2S, and OI correlates with C2S, OI could be interpreted as a compensatory reservoir of each individual. Regarding these facts, we anticipate that the value of OT might somehow be related to cervical deformity.
The utilization of the odontoid parameters has some advantages. OI, as proposed in this study, is an independent and individual parameter not affected by any external factors. By measuring an angle within a single bony structure, we were able to define an angle devoid of muscles or other factors of mobility. We hypothesized that OI is an important parameter influencing cervical alignment from the rostral portion and can be used as a fixed reference point in understanding the physiological alignment of the cervical spine. The relationship between the odontoid parameters is also similar to that between the pelvic parameters [15], which provides a better understanding of the concept and more straightforward clinical discussions. Though the correlation shown in the regression analysis is not strong, a significant chain of correlation is observed between previously reported cervical parameters and the odontoid parameters (Fig. 4). Although the correlation coefficients between established sagittal parameters are similar to previous report [23], the correlation cannot be said strong to say the parameters are interconnected. However, as most parameters show, the more cranial the parameter is, they tend to show less correlation coefficients [16]. The global spinal and thoracic sagittal alignment strongly influence cervical parameters [34]. In addition, regarding the cone of economy, the cervical spine show larger zone of balance. Thus, other factors may contribute to the overall alignment of the cervical spine more compared with the most cranial odontoid parameters, resulting in moderate correlation coefficients. Larger capacity to compensate cause weaker correlation, which also makes the cervical spine harder to analyze. Using both established and odontoid parameters will aid in providing a more detailed analysis of the cervical alignment.
Though the parameters cannot explain all clinical findings, the pelvic parameters are currently widely used. Due to a small number, subgroup analysis based on global sagittal alignment was note performed. However, multivariable regression analysis indicated that T1S with OI and OT were significant predictors of CL. Moreover, the axis is always visible on plain lateral radiographs, unlike either C7 or T1, which may provide more reliability [35].
This study has several limitations. First, it is a retrospective study; therefore, there were minor variations in subjects’ positions in radiographic images, leading to a possibility of selection bias. Secondly, there was an uneven distribution of sex and there is a wide age range of the examined subjects. Third, the number of cases is small for an anatomical study, and a clinical and prognostic postoperative correlation was not demonstrated. Subgroup analysis regarding global alignment, age, and sex was not performed due to a small number of patients.
Despite the small number of subjects and limitations, this study provides a comprehensive review of the global sagittal alignment using whole-spine radiographs. As the cervical alignment is strongly influenced by the global thoracic and spinal sagittal alignment, the study may provide the bases of utmost importance in future research. The wide age range, not limited to a particular generation, and normal age distribution show the sample’s representativeness of the population. The results of the present study demonstrated that the odontoid parameters influence the alignment subaxial CL from the rostral end and serve as the foundation of upper CL. The structural characteristics of the axis represented by the OI could serve as a reference point assessing cervical spine as it is a fixed value. Despite the limitations, the present study may outline the possible role of the odontoid parameters and provide a fresh perspective of the spinal alignment. It will lead to future research regarding the relationship between the odontoid parameters and clinical outcomes. Further studies should ensue to define the relationship between the odontoid parameters and the global alignment, HRQoL, and its contribution to the cervical sagittal balance with a larger number of cases. The present study results may serve as baseline data for further studies on the alignment and balance of the cervical spine in clinical conditions.
The evidence of this study implies that OI is an essential factor in regulating the physiological sagittal alignment of the cervical spine from the top. OI, OT, and C2S had significant correlations with cervical alignment. Like PI, OI could be a promising parameter since it is the only anatomical and constant parameter related to the cervical spine, and therefore, OI could be a reliable parameter to evaluate interindividual variations of cervical alignment. The pelvic parameters provide a firm foundation from the caudal end, the odontoid parameters might be the cherry on top. Altogether, OI, OT, C2S, and T1S can be used to assess normal cervical alignment, and the results of the study may serve as baseline data for further studies on the alignment and balance of the cervical spine.
NOTES
Fig. 1.
Schematic drawing of the odontoid parameters. (A) Odontoid incidence (OI): the angle between the line perpendicular to the C2 endplate at its midpoint and the line connecting this point to the center of the odontoid process (the center of a circle with an anterior/posterior border and the apex of the dens as a tangent). Odontoid tilt (OT): the angle created by a line running from the C2 endplate midpoint to the center of the odontoid process and the vertical axis (VRL) C2 slope (C2S): the angle between the C2 endplate and a horizontal line (HRL). (B) Inverse illustration demonstrating similarity with the pelvic parameters. (C) The “geometric proof” demonstrates the mathematical association of odontoid parameters. Mathematically, OI was defined as the sum of OT and C2S.

Fig. 3.
Schematic illustration showing that an increase in C2 slope leads to a decrement in the odontoid tilt and anterior shifting of the vertical axis from the center of the odontoid process. The sum of C2 slope and the odontoid tilt is a constant.

Fig. 4.
Schematic illustration of the chain of correlation of cervical and odontoid parameters. The correlation from the caudal end to the rostral end (blue arrow) and from the rostral to caudal end (orange arrow) is illustrated.

Table 1.
Mean sagittal parameters and demographics
| Variable | Total (n = 42) | Male (n = 15) | Female (n = 27) | p-value |
|---|---|---|---|---|
| Age (yr) | 49.4 (15–68)† | 44.5 ± 16.2 | 52.2 ± 11.0 | 0.11 |
| Odontoid parameters | ||||
| Odontoid incidence (°) | 17.7 ± 3.7 | 17.5 ± 4.3 | 17.7 ± 3.4 | 0.84 |
| Odontoid tilt (°) | 6.7 ± 5.3 | 4.7 ± 4.5 | 7.8 ± 5.4 | 0.06 |
| C2 slope (°) | 10.9 ± 6.2 | 12.8 ± 5.1 | 9.9 ± 6.6 | 0.15 |
| Cervical sagittal parameters | ||||
| C0–2 angle (°) | -25.6 ± 8.8 | -27.4 ± 8.9 | -24.6 ± 8.7 | 0.31 |
| C2–3 angle (°) | -0.4 ± 3.8 | -1.5 ± 3.7 | 0.1 ± 3.8 | 0.21 |
| C2–4 angle (°) | -3.1 ± 5.1 | -3.9 ± 4.0 | -2.6 ± 5.6 | 0.41 |
| C2–5 angle (°) | -4.3 ± 6.6 | -4.5 ± 4.5 | -4.2 ± 7.6 | 0.92 |
| C2–6 angle (°) | -6.2 ± 6.2 | -5.4 ± 5.2 | -6.7 ± 6.8 | 0.53 |
| C2–7 angle (°) | -10.4 ± 7.3 | -9.5 ± 6.7 | -11.0 ± 7.7 | 0.54 |
| C2–7 SVA (mm) | 17.8 ± 6.8 | 20.8 ± 6.2 | 16.1 ± 6.6 | 0.03* |
| T1 slope (°) | 23.1 ± 6.3 | 24.1 ± 5.7 | 22.6 ± 6.6 | 0.45 |
| T1 slope – C2–7 angle (°) | 12.7 ± 6.5 | 14.6 ± 6.0 | 11.6 ± 6.6 | 0.15 |
| Global sagittal parameters | ||||
| C5–T3 angle (°) | -0.3 ± 6.3 | -0.5 ± 5.4 | -0.2 ± 6.8 | 0.88 |
| Thoracic kyphosis (°) | 29.6 ± 10.4 | 27.6 ± 8.7 | 30.8 ± 11.2 | 0.37 |
| Lumbar lordosis (°) | -48.1 ± 10.3 | -44.8 ± 8.7 | -50.0 ± 1.8 | 0.12 |
| Pelvic tilt (°) | 13.4 ± 7.2 | 11.2 ± 7.8 | 14.6 ± 6.6 | 0.14 |
| Sacral slope (°) | 33.2 ± 6.9 | 31.6 ± 7.7 | 34.1 ± 6.3 | 0.27 |
| Pelvic incidence (°) | 46.6 ± 8.6 | 42.9 ± 9.1 | 48.7 ± 7.7 | 0.03* |
| C7–S1 SVA (mm) | 4.4 ± 28.2 | 7.1 ± 26.5 | 2.8 ± 29.5 | 0.65 |
Table 2.
Pearson correlation coefficients of the odontoid and cervical, and global parameters
| Variable |
Odontoid parameter |
Cervical parameter |
||||||
|---|---|---|---|---|---|---|---|---|
| OI | OT | C2S | C0–2 | C2–7 | cSVA | T1S | T1S–CL | |
| OI | X | |||||||
| OT | 0.09 | X | ||||||
| C2S | 0.52*** | -0.8*** | X | |||||
| C0–2 | -0.33* | 0.48*** | -0.61*** | X | ||||
| C2–7 | 0.43** | -0.42*** | 0.62*** | -0.28 | X | |||
| cSVA | 0.14 | -0.57*** | 0.57*** | -0.24 | 0 | X | ||
| T1S | -0.2 | -0.32* | 0.16 | -0.15 | -0.55*** | 0.46** | X | |
| T1S–CL | 0.3 | -0.78*** | 0.84*** | -0.46*** | 0.59*** | 0.44** | 0.35* | X |
| C5–T3 | 0.26 | -0.08 | 0.22 | -0.04 | 0.16 | 0.33* | -0.21 | -0.02 |
| TK | 0.1 | -0.29 | 0.31* | -0.19 | -0.33* | 0.48** | 0.69** | 0.3 |
| TL | -0.3 | -0.43** | 0.19 | -0.21 | 0.04 | 0.25 | 0.21 | 0.25 |
| LL | -0.09 | 0.2 | -0.23 | 0.13 | 0.07 | -0.26 | -0.36* | -0.27 |
| PT | -0.25 | 0.16 | -0.28 | -0.08 | -0.17 | -0.09 | -0.03 | -0.22 |
| SS | -0.07 | -0.03 | -0.01 | 0.02 | -0.08 | 0.01 | 0.15 | 0.06 |
| PI | -0.26 | 0.11 | -0.25 | -0.05 | -0.2 | -0.06 | 0.09 | -0.14 |
| SVA | -0.33* | 0.02 | -0.21 | 0.14 | -0.34* | 0.03 | 0.22 | -0.17 |
Table 3.
Adjusted r2 between parameters matched with established cervical alignment parameters using a linear regression model
| Variable | OI | OT | C2S | T1S |
|---|---|---|---|---|
| C0–2 angle | 0.08* | 0.21** | 0.35** | -0.01 |
| C2–7 angle | 0.17** | 0.15** | 0.36** | 0.28** |
| T1S–CL | 0.06 | 0.59** | 0.70** | 0.10* |
| cSVA | -0.01 | 0.30** | 0.30** | 0.19** |
Table 4.
Parameter estimates of multivariable linear regression models
REFERENCES
1. Le Huec JC, Saddiki R, Franke J, et al. Equilibrium of the human body and the gravity line: the basics. Eur Spine J 2011;20 Suppl 5(Suppl 5):558-63.

2. Ha Y, Schwab F, Lafage V, et al. Reciprocal changes in cervical spine alignment after corrective thoracolumbar deformity surgery. Eur Spine J 2014;23:552-9.




3. Diebo BG, Challier V, Henry JK, et al. Predicting cervical alignment required to maintain horizontal gaze based on global spinal alignment. Spine (Phila Pa 1976) 2016;41:1795-800.



4. Hyun SJ, Kim KJ, Jahng TA. The differential effect of cervical kyphosis correction surgery on global sagittal alignment and health-related quality of life according to head- and trunk-balanced subtype. J Neurosurg Spine 2021 Apr 2:1-10. https://doi.org/10.3171/2020.9.SPINE201309. [Epub].


5. Lafage R, Challier V, Liabaud B, et al. Natural head posture in the setting of sagittal spinal deformity: validation of chinbrow vertical angle, slope of line of sight, and McGregor’s slope with health-related quality of life. Neurosurgery 2016;79:108-15.

6. Lee SH, Hyun SJ, Jain A. Cervical sagittal alignment: literature review and future directions. Neurospine 2020;17:478-96.




7. Scheer JK, Lau D, Smith JS, et al. Alignment, classification, clinical evaluation, and surgical treatment for adult cervical deformity: a complete guide. Neurosurgery 2021;88:864-83.



8. Yoshimoto H, Ito M, Abumi K, et al. A retrospective radiographic analysis of subaxial sagittal alignment after posterior C1-C2 fusion. Spine (Phila Pa 1976) 2004;29:175-81.


9. Kim JT, Lee HJ, Choi DY, et al. Sequential alignment change of the cervical spine after anterior cervical discectomy and fusion in the lower cervical spine. Eur Spine J 2016;25:2223-32.



10. Protopsaltis TS, Lafage R, Vira S, et al. Novel angular measures of cervical deformity account for upper cervical compensation and sagittal alignment. Clin Spine Surg 2017;30:E959-67.


11. Harrison DE, Harrison DD, Haas JW, et al. Do sagittal plane anatomical variations (angulation) of the cervical facets and C2 odontoid affect the geometrical configuration of the cervical lordosis? Clin Anat 2005;18:104-11.


12. Johnson GM. The correlation between surface measurement of head and neck posture and the anatomic position of the upper cervical vertebrae. Spine (Phila Pa 1976) 1998;23:921-7.


13. Koebke J. Morphological and functional studies on the odontoid process of the human axis. Anat Embryol (Berl) 1979;155:197-208.



14. Yan YZ, Shao ZX, Pan XX, et al. Acceptable chin-brow vertical angle for neutral position radiography: preliminary analyses based on parameters of the whole sagittal spine of an asymptomatic chinese population. World Neurosurg 2018;120:e488-96.


15. Legaye J, Duval-Beaupere G, et al. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J 1998;7:99-103.




16. Ames CP, Blondel B, Scheer JK, et al. Cervical radiographical alignment: comprehensive assessment techniques and potential importance in cervical myelopathy. Spine (Phila Pa 1976) 2013;38:S149-60.

17. Lee SH, Kim KT, Seo EM, et al. The influence of thoracic inlet alignment on the craniocervical sagittal balance in asymptomatic adults. J Spinal Disord Tech 2012;25:E41-7.


18. Divi SN, Bronson WH, Canseco JA, et al. How do C2 tilt and C2 slope correlate with patient reported outcomes in patients after anterior cervical discectomy and fusion? Spine J 2021;21:578-85.


19. Protopsaltis TS, Ramchandran S, Tishelman JC, et al. The importance of C2 slope, a singular marker of cervical deformity, correlates with patient-reported outcomes. Spine (Phila Pa 1976) 2020;45:184-92.


20. Iyer S, Nemani VM, Nguyen J, et al. Impact of cervical sagittal alignment parameters on neck disability. Spine (Phila Pa 1976) 2016;41:371-7.


21. Hyun SJ, Han S, Kim KJ, et al. Assessment of T1 slope minus cervical lordosis and C2-7 sagittal vertical axis criteria of a cervical spine deformity classification system using longterm follow-up data after multilevel posterior cervical fusion surgery. Oper Neurosurg (Hagerstown) 2019;16:20-6.


22. Massaad E, Hadzipasic M, Kiapour A, et al. Association of spinal alignment correction with patient-reported outcomes in adult cervical deformity: review of the literature. Neurospine 2021;18:533-42.




23. Lee SH, Son ES, Seo EM, et al. Factors determining cervical spine sagittal balance in asymptomatic adults: correlation with spinopelvic balance and thoracic inlet alignment. Spine J 2015;15:705-12.


24. Scheer JK, Tang JA, Smith JS, et al. Cervical spine alignment, sagittal deformity, and clinical implications: a review. J Neurosurg Spine 2013;19:141-59.

25. Sivaganesan A, Smith JS, Kim HJ. Cervical deformity: evaluation, classification, and surgical planning. Neurospine 2020;17:833-42.




26. Staub BN, Lafage R, Kim HJ, et al. Cervical mismatch: the normative value of T1 slope minus cervical lordosis and its ability to predict ideal cervical lordosis. J Neurosurg Spine 2018;30:31-7.


27. International Spine Study G; Klineberg EO, Carlson BB, et al. Can measurements on cervical radiographs predict concurrent thoracolumbar deformity and provide a threshold for acquiring full-length spine radiographs? The Spine Journal 2015;15:S146.

28. Kim CW, Hyun SJ, Kim KJ. Surgical impact on global sagittal alignment and health-related quality of life following cervical kyphosis correction surgery: systematic review. Neurospine 2020;17:497-504.




29. Protopsaltis T, Terran J, Soroceanu A, et al. T1 slope minus cervical lordosis (TS-CL), the cervical answer to PI-LL, defines cervical sagittal deformity in patients undergoing thoracolumbar osteotomy. Int J Spine Surg 2018;12:362-70.



30. Ames CP, Smith JS, Eastlack R, et al. Reliability assessment of a novel cervical spine deformity classification system. J Neurosurg Spine 2015;23:673-83.


31. Pierce KE, Passias PG, Brown AE, et al. Prioritization of realignment associated with superior clinical outcomes for cervical deformity patients. Neurospine 2021;18:506-14.




32. Lee SH, Raad M, Neuman BJ, et al. Friday, September 28, 2018 4:05 PM–5:05 PM abstracts: cervical myelopathy and deformity: 258. The C5-T3 angle: a novel parameter of the cervicothoracic junction. Spine J 2018;18(8 Suppl):S127-8.
33. Makhni MC, Shillingford JN, Laratta JL, et al. Restoration of sagittal balance in spinal deformity surgery. J Korean Neurosurg Soc 2018;61:167-79.