- Search
|
|
||
This article has been corrected. See "Erratum: Reciprocal Changes Following Cervical Realignment Surgery" in Volume 20 on page 1091.
Abstract
Over the last few decades, the importance of the sagittal plane and its contour has gained significant recognition. Through full-body stereoradiography, the understanding of compensatory mechanisms, and the concept of global balance and reciprocal change has expanded. There have been a few reports describing how cervical realignment surgery affects global spinal alignment (GSA) and global balance. Despite the research efforts, the concept of reciprocal change and global balance is still perplexing. Understanding the compensatory status and main drivers of deformity in a patient is vital because the compensatory mechanisms may resolve reciprocally following cervical realignment surgery. A meticulous preoperative evaluation of the whole-body alignment, including the pelvis and lower extremities, is paramount to appreciate optimal GSA in the correction of spinal malalignment. This study aims to summarize relevant literature on the reciprocal changes in the whole body caused by cervical realignment surgery and review recent perspectives regarding cervical compensatory mechanisms.
Over the last few decades, the importance of the sagittal plane and its contour has gained significant recognition. Through full-body stereoradiography, the understanding of compensatory mechanisms in patients with spinopelvic imbalance has progressed rapidly, and the concept of global balance and reciprocal change has expanded to the field of the cervical spine and lower extremities [1]. The regions of the spine are intertwined through compensatory mechanisms. When a patient loses an adequate lumbar lordosis (LL), compensatory mechanisms are recruited to maintain an upright posture; cervical hyperlordosis, thoracic kyphosis (TK), pelvic retroversion, and knee flexion [2-7]. The sagittal alignment regarding spinopelvic parameters and reciprocal changes in the thoracolumbar spine has been well documented [8-12].
The essential function of global spinal alignment (GSA) is the maintenance of global balance, an upright posture, and a horizontal gaze [13]. Thus, in the setting of thoracolumbar spinal deformity, cervical alignment is the final piece affected by GSA through compensatory mechanisms to maintain a horizontal gaze [4,13-18]. Likewise, recent studies report that cervical kyphotic deformity showed compensatory changes in the thoracolumbar spine, analogous to the changes that occur in thoracolumbar deformity [19-23]. At the regional level, the upper cervical spine compensates for C2–7 angle through the extension of C0–2, thereby maintaining the patient’s horizontal gaze [22-27].
Understanding the compensatory status of a patient is vital because the compensatory mechanisms may resolve reciprocally following cervical realignment surgery which correlates with improved patient outcome [19,23]. Despite the efforts, understanding and anticipating the reciprocal changes that occur following realignment surgery is perplexing. Further, a new approach should be taken into account to comprehend reciprocal changes. This study aims to summarize relevant literature on the reciprocal changes in the whole body caused by cervical realignment surgery and review recent perspectives regarding cervical compensatory mechanisms.
It is critical to understand the compensatory mechanisms and global balance of the spine beforehand as reciprocal change is a dynamic phenomenon. The sagittal balance reflects the spine’s shape, allowing individuals to maintain a standing position with minimal muscle force. The spine adapts to different changes in order to stay in balance. The normal aging process induces truncal stooping [28,29]. To adapt to morphological variations that occur in the spine, several compensatory mechanisms are implemented to maintain optimal GSA (Fig. 1) [7]. The aging-related deterioration of the GSA is compensated by supportive functions of the spine, pelvis, and lower limbs [17]. The compensations happen to refrain from the anterior shifting of the gravity line (GL). The compensatory mechanisms do not occur simultaneously but are closely associated depending on the stiffness of the spine, musculature status, painful phenomena, and severity of the imbalance [7]. All mechanisms integrate with different ways depending on each individual.
In patients with spinal pathologies, compensatory mechanisms from the thoracolumbar to the cervical spine and lower extremities occur in a staged fashion to maintain horizontal gaze and global balance [30]. In patients with spinal deformity at any level, initial compensatory mechanisms usually initiate adjacent to the deformity. After the exhaustion of the adjacent compensatory reservoir, the next adjacent segments are subsequently recruited to maintain an erect posture and balance [7]. Roussouly and Pinheiro-Franco [31] hypothesized the following sequential mechanism of compensation of progressive kyphosis: (1) a normal stage with slight pelvic retroversion and the C7 plumb line (C7PL) over the sacral endplate, (2) a compensated stage, with a progressive loss of LL and pelvic retroversion to maintain the C7PL posterior to the femoral heads; and (3) a decompensated stage, wherein hip extension limits pelvic retroversion, which is compensated by knee flexion, and the C7PL passes forward to the femoral heads. With the hips maximally extended and the knees flexed, the last posture is well-known in severe kyphosis and is very uncomfortable and uneconomical [31]. Accordingly, patients with thoracolumbar malalignment exhibit compensatory changes in the form of cervical hyperlordosis, posterior pelvic shift, ankle dorsiflexion, knee flexion, hip extension, and pelvic retroversion [3-7]. In addition, recent investigations have shown that cervical alignment is also affected by GSA through compensatory mechanisms to maintain an upright posture and horizontal gaze [4,13-18]. Changes in cervical kyphosis (CK) reduce TK to correct alignment and maintain cone of economy of global spinal balance. To compensate for CK, posterior shifting of the C7PL, a decrease in T1 slope (T1S), and an increase in LL occurs [5,32]. Therefore, to truly understand a patient’s state of balance, it is necessary to evaluate GSA because the compensatory mechanism for global malalignment is present [30].
For an overall assessment of a patient with spinal imbalance, radiography of the entire spine with a standardized position (hands resting on collar bones) is mandatory [33,34]. Radiographs to analyze the overall sagittal balance including the lower limbs can be made with the EOS imaging system (EOS Imaging, Paris, France). The EOS system was developed to overcome the limitations of conventional radiography by interdisciplinary investigators [1]. Using the 3-dimensional bone external envelope technique, EOS allows bilateral long-length images (whole-body or localized) in either the standing or seated position, with overall enhanced image quality and a lower radiation dose for the patient [35,36]. Through whole-body radiographs, our understanding of the global balance and reciprocal changes in the cervical spine and the lower extremities became more profound.
Global balance can be determined by the position of the GL, defined as a plumb line from the center of the acoustic meatus (CAM) [14,37]. The normal location of bony landmarks in standing whole-body radiographs in reference to the GL has been reported using the EOS imaging system (Fig. 2) [17]. It has been proposed that the optimal goal of a truly balanced spine is to maintain the head over femoral heads, suggesting that the position of the head is an important driver of true spinal balance [38]. Recent investigations revealed that the mean offset distance from the center of gravity (COG) to the CAM was 0, and was not affected by aging [17]. It suggests that when the global alignment gradually deteriorates with age as aging induces truncal stooping (Fig. 1) [17], the change is compensated in order to maintain both horizontal gaze and global balance [39]. Loss of lordosis and an increase in pelvic tilt were induced by the posterior shift of the lower lumbar vertebrae and sacrum, to maintain optimal positioning of the GL above the COG [17].
In patients with spinal deformity, initial compensatory mechanisms usually initiate adjacent to the deformity. The next adjacent segments will be subsequently recruited after the exhaustion of adjacent compensatory reservoir to maintain an erect posture and balance [7]. Sequential linkage of correlation has been demonstrated in asymptomatic subjects between C0–2 angle, C2–7 angle, and T1S; C2–7 angle showed a negative correlation with both C0–2 and T1S [40]. In CK patients, the upper cervical spine is recruited to maintain balance. Thus, at the regional level, kyphotic alignment of the subaxial cervical spine is known to be compensated by a lordotic upper cervical spine and vice versa, which illustrates a regional compensatory mechanism [24,26,27,41]. The upper cervical spine is the most mobile segment, hence the compensatory mechanism of the upper cervical spine would allow a patient to maintain horizontal gaze [42].
After cervical realignment surgery, reciprocal changes ensue. If the alignment is inadequate, it intensifies the compensatory mechanisms. When realignment surgery is adequately performed, it often leads to the relaxation of compensatory mechanisms [43]. Hyperlordotic positioning of the upper cervical spine leads to a kyphotic alignment of the subaxial spine to maintain balanced cervical alignment [41]. After a patient recovers optimal cervical lordosis (CL), C0–2 angle reciprocally decreases [22]. Concurrently, Lafage et al. [23] reported that correction of sagittal cervical deformity (CD) led to reciprocal relaxation of the established CD compensatory mechanisms such as C0–2 hyperlordosis and thoracic hypokyphosis [23]. Furthermore, the preoperative Neck Disability Index (NDI) had a significant correlation with preoperative C0–2 range of motion (ROM) and reserve of extension (ROE). Relaxation of compensatory mechanisms was found to be associated with improvement in patients’ reported clinical outcomes. The inclusion of ROM and ROE, as it is associated with patient-reported outcomes, can help to better understand this complex condition at a regional level.
Traditionally, a balanced spine is defined as whether spinopelvic parameters, including the C7PL, are adequate. The C7PL was used to measure sagittal trunk balance as a virtual COG rather than GL, as it is generally concordant with GL in general populations and is a pragmatic tool to estimate sagittal trunk balance [44,45]. However, the spine can be in balance (compensated), but spinopelvic parameters can be inadequate [33]. Even though C7PL is an easy method to estimate sagittal balance, its discordance with the GL has been widely recognized [29,44]. When the distance between the GL and C7PL exceeds 30 mm, it is defined as occiput-trunk (OT) discordance [44]. True GSA cannot be assessed using C7PL when there is OT discordance [38]. Patients with CD are unable to accomplish OT concordance by extending the cervical segment. A posterior shifting of C7PL is therefore necessary for optimal positioning of the head. Following C7PL posterior shifting, subsequent thoracolumbar alignment compensation takes place [21]. Hence, the concept of global balance utilizing GL was implemented to assess patients undergoing cervical realignment surgery.
Only a handful of research has been conducted regarding how cervical realignment surgery reciprocally affects GSA [19-21,32,46]. It has first been reported that surgical correction of CK leads to an increase in preoperatively decreased T1S and TK, but did not influence lumbar or pelvic parameters.32 However, a recent study reported 2 different groups of CD patients with different compensatory mechanisms based on the preoperative location of the C7PL (Fig. 3); the head-balanced type and the trunk-balanced type [21]. According to the C7PL value, the former was balanced globally while the latter was balanced below the trunk. In detail, the head-balanced patients were those with a posterior shifting of the C7PL but with optimal GL location. The head-balanced group is balanced globally, including the head, with hyper-lumbar lordosis, and a low T1S. Trunk-balanced patients are unable to shift the C7PL posteriorly, have upper-limit pelvic incidence–LL values, and have normal T1S.
The primary goal of cervical realignment surgery is to achieve OT concordance [20]. Once OT concordance is achieved, subsequent thoracolumbar alignment changes occur to harmonize GSA, showing that cervical reconstruction can restore both cervical deformities and GSA [20]. Subsequently, thoracolumbar alignment changed to harmonize the entire spinal alignment. Although mild CD affects adjacent segments, a severe CD can alter even the lumbar segments. Cervical realignment surgery induces reciprocal changes and restores both cervical and global balance. Correction in the head-balanced group resulted in anterior shifting of C7PL, a subsequent increase in T1S and TK, and a decrease in LL.
A significant chain of correlation has been demonstrated in asymptomatic subjects between C0–2 angle, C2–7 angle, and T1S [40]. T1S has been suggested as a key factor in understanding cervical alignment [40]. In a given T1S, an adequate C2–7 angle is necessary in order to maintain optimal head balance. If CL is insufficient to match a given T1S, the dens tilts forward, resulting in an increase in C2 slope (C2S) (Fig. 4) [47].
Lee et al. [27] introduced a novel concept of odontoid parameters, similar to the inverted pelvic parameters (Fig. 5). A significant chain of correlation is noted between cervical and odontoid parameters. Linear regression analysis demonstrated a significant correlation of C2–7 angle with odontoid incidence (OI), OT, and T1S, which suggests that in a given T1S, the structural characteristics of the dens affect optimal cervical alignment in each individual. They indicated a large OI decreased C2–7 angle to preserve the optimal head position and horizontal gaze. As OI is a constant and fixed value, the odontoid parameters could provide a concrete anatomical base for understanding cervical alignment from the cephalad end.
To understand the clinical role of the odontoid parameters, we analyzed the correlation between patient-reported health-related quality of life and odontoid parameters in patients who underwent a multilevel posterior cervical fusion. First of all, the postoperative NDI showed a significant correlation with both OT (r = -0.37, p < 0.05) and OI (r = -0.40, p < 0.05). Secondly, a cutoff value of 20° for the T1S-CL corresponds to OT of 0° in a linear regression model (r2 = 0.702, p < 0.001). Lastly, a significant correlation between OI and ROM of both C1–2 (r = 0.37, p < 0.05) and C0–2 (r = 0.46, p < 0.01) has been observed.
Based on these results, we postulated that depending on OI of a patient, the clinical impact of anterior tilting of the dens may differ as the resulting OT is distinct [27]. At a given C2S, patients with a larger OI have a larger OT, which helps to retain the COG of the odontoid process more posteriorly, withholding it from losing balance (Fig. 4). It can be assumed that the threshold of imbalance differs in each individual. Also, ROM and ROE of the upper cervical spine are associated with improved clinical outcomes [23]. OI is positively correlated with C1–2 extension angle, C1–2 ROM, and C0–2 ROM, concurrent with a previous biomechanical study [48]. The reserve to extend the upper cervical spine is related to the anatomical characteristics of the dens. A patient with a larger OI can be assumed to have a larger compensatory reservoir or ROE. As a result, a patient with a larger OI can maintain a positive OT, which is significantly correlated with an improved NDI score. Therefore, implementing the odontoid parameters will aid in a better understanding of the reciprocal changes in the cervical spine in the future.
Reciprocal changes following cervical realignment surgery in CD patients exhibit different patterns depending on whether they have an adequate compensatory reservoir in the thoracolumbar spine [19]. In our practice, we divide patients into 2 CD subgroups; compensated and decompensated (Fig. 6). In patients with compensated CK (i.e., head-balanced, Fig. 4A, B), the posteriorly shifted C7PL before surgery shifts anteriorly after correction. Subsequently, TK and T1S increase while LL decreases. In contrast, no significant changes in thoracolumbar alignment occur in patients with decompensated patients (i.e., trunk-balanced, Fig. 6C, D) following realignment surgery. While T1S and TK decrease, spinopelvic and lower extremity parameters remain constant. In a previous study of these 2 groups, patients with decompensated CK showed decreases in T1S and TK, but no changes occurred in spinopelvic and lower extremity parameters. In addition, the C0–1 and C1–2 angles became kyphotic and less lordotic, respectively, after surgery [19]. No changes were observed in the pelvic and lower extremity parameters in both groups [19]. As specific implications, a selective cervical correction would be possible for the compensated subtype, whereas both cervical and thoracic correction would be necessary for the decompensated subtype [19].
The cervical spine is still one of the most understudied and least understood parts of the spine. It is crucial to identify the drivers of CD and each compensatory mechanism connected with the deformity. Analyzing the compensatory mechanisms such as C0–2 hyperlordosis, posterior thoracolumbar malalignment, or thoracic hypokyphosis in isolation can be mistaken for a surgical indication or even a sign of deformity. Spine surgeons should recognize and accurately address the regional drivers of the deformities for optimal treatment. A meticulous preoperative evaluation of the whole-body alignment, including the pelvis and lower extremities, is paramount to appreciate optimal GSA in the correction of spinal malalignment. This study adds to the literature by advocating whole-body analysis for all CD patients. The proverb, “Do not miss the forest for the trees.” is helpful to understand the malalignment of the spine. Furthermore, it has been challenging for spine surgeons and researchers to predict reciprocal changes following realignment surgery. Expanding our ability to not only simulate postoperative alignment of the fused segments but also methodically and systematically predict reciprocal changes in the unfused segments is crucial. A future approach to CD needs to take reciprocal changes in the thoracolumbar spine, as well as the cervical spine to provide optimal planning of realignment surgery and achieve ideal cervical alignment.
NOTES
Fig. 1.
Compensatory mechanisms for age-related progressive kyphosis. This schematic illustration demonstrates the same person aging from left to right. When he ages, lumbar lordosis decreases, which results in a combination of different compensatory mechanisms to maintain horizontal gaze and global balance. TK, thoracic kyphosis.
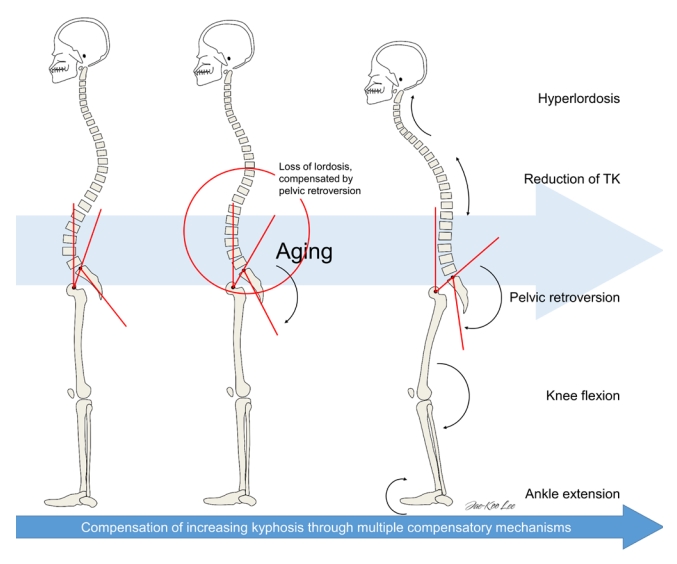
Fig. 2.
Normative offset distances between bony landmarks and the gravity line. Positive values denote locations anterior to the gravity line and negative values indicate locations posterior to the gravity line. CAM, center of the acoustic meatus; CI, confidence interval.
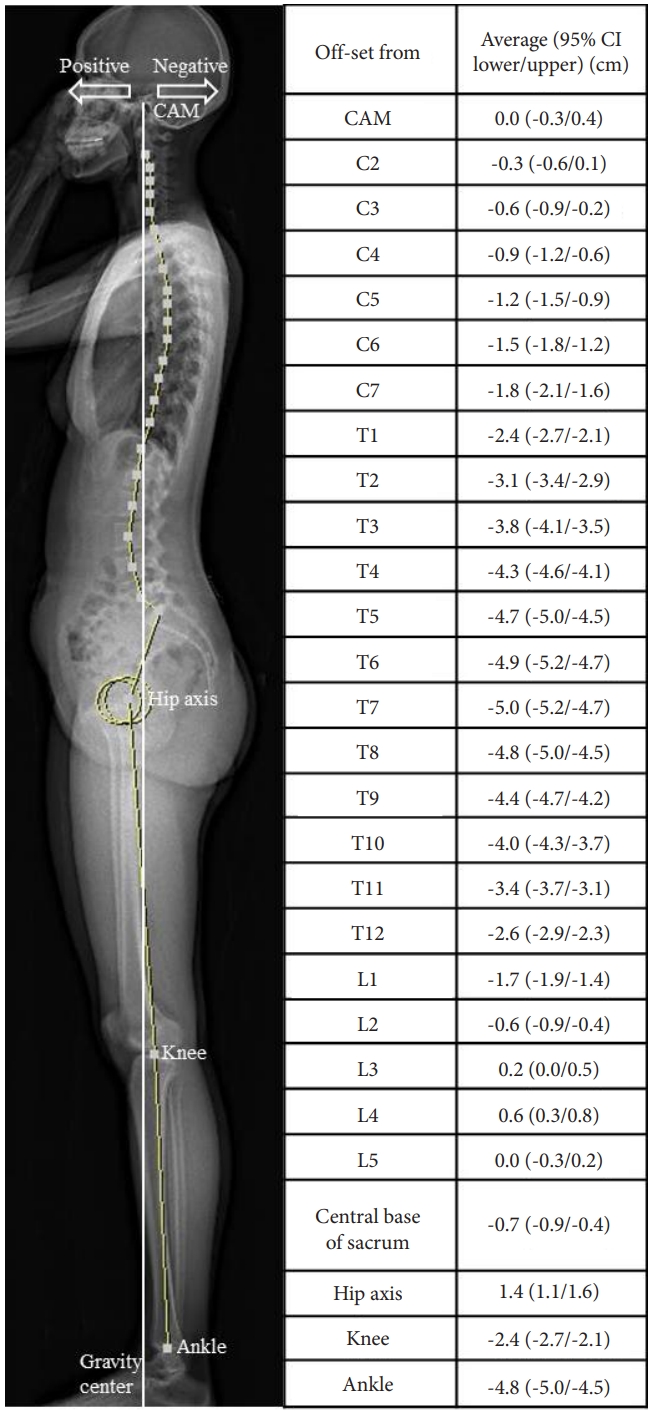
Fig. 3.
Compensatory mechanisms in patients with symptomatic cervical kyphosis. PL, plumb line; CK, cervical kyphosis; LL, lumbar lordosis; PI, pelvic incidence; TK, thoracic kyphosis.
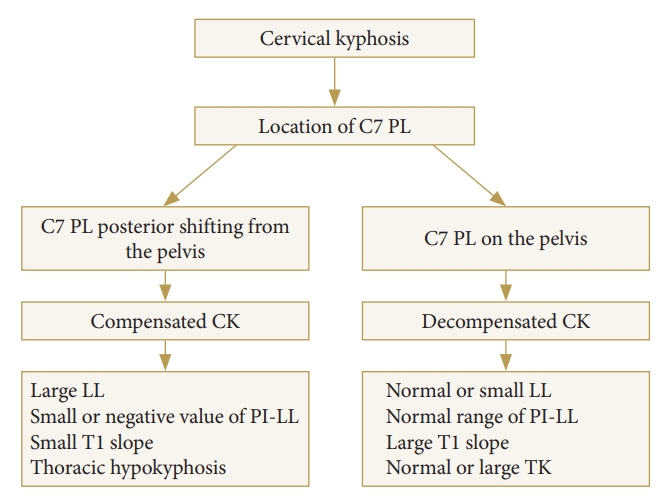
Fig. 4.
Schematic drawings illustrating the different spatial orientations of the dens with an identical C2 slope and different odontoid incidence values. (A) A dens with a straight curvature is conducive to a small odontoid incidence, prone to anterior tilting of the center of the dens. (B) A dens with a lordotic curvature can maintain the center of the dens more posteriorly.
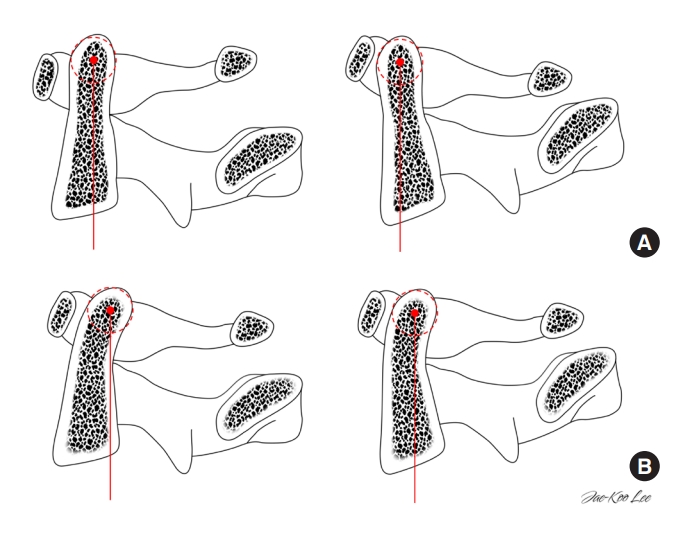
Fig. 5.
Schematic drawing of the odontoid parameters. (A) Odontoid incidence (OI): the angle between the line perpendicular to the C2 endplate at its midpoint and the line connecting this point to the center of the odontoid process (the center of a circle with an anterior/posterior border and the apex of the dens as a tangent). Odontoid tilt: the angle created by a line running from the C2 endplate midpoint to the center of the odontoid process and the vertical axis (VRL) C2 slope: the angle between the C2 endplate and a horizontal line (HRL). (B) Inverse illustration demonstrating similarity with the pelvic parameters.

Fig. 6.
(A) Compensated cervical kyphosis patient with the COG PL located on the femoral head, but the C7 PL located markedly posteriorly. Cervical malalignment was corrected to achieve global sagittal balance and OT concordance. However, the lower-extremity alignment parameters did not change significantly. (B) Decompensated cervical kyphosis patient with the COG PL located markedly anteriorly, but the C7 PL located on the femoral head. Sagittal PLs indicated cervical sagittal imbalance and OT discordance before surgery. No significant changes were found in lumbopelvic alignment or the lower-extremity alignment parameters. COG, center of gravity; PL, plumb line; OT, occiput-trunk.

REFERENCES
1. Lee JK, Hyun SJ, Kim KJ. Reciprocal changes in the wholebody following realignment surgery in adult spinal deformity. Asian Spine J 2022 May 10 https://doi.org/10.31616/asj.2021.0451. [Epub].

2. Iyer S, Lenke LG, Nemani VM, et al. Variations in sagittal alignment parameters based on age: a prospective study of asymptomatic volunteers using full-body radiographs. Spine (Phila Pa 1976) 2016;41:1826-36.

3. Day LM, Ramchandran S, Jalai CM, et al. Thoracolumbar realignment surgery results in simultaneous reciprocal changes in lower extremities and cervical spine. Spine (Phila Pa 1976) 2017;42:799-807.


4. Diebo BG, Ferrero E, Lafage R, et al. Recruitment of compensatory mechanisms in sagittal spinal malalignment is age and regional deformity dependent: a full-standing axis analysis of key radiographical parameters. Spine (Phila Pa 1976) 2015;40:642-9.

5. Lamartina C, Berjano P. Classification of sagittal imbalance based on spinal alignment and compensatory mechanisms. Eur Spine J 2014;23:1177-89.



6. Shimizu T, Lehman RA Jr, Sielatycki JA, et al. Reciprocal change of sagittal profile in unfused spinal segments and lower extremities after complex adult spinal deformity surgery including spinopelvic fixation: a full-body X-ray analysis. Spine J 2020;20:380-90.


7. Barrey C, Roussouly P, Le Huec JC, et al. Compensatory mechanisms contributing to keep the sagittal balance of the spine. Eur Spine J 2013;22(Suppl 6):S834-41.




8. Ames CP, Blondel B, Scheer JK, et al. Cervical radiographical alignment: comprehensive assessment techniques and potential importance in cervical myelopathy. Spine (Phila Pa 1976) 2013;38(22 Suppl 1):S149-60.

9. Roussouly P, Pinheiro-Franco JL. Sagittal parameters of the spine: biomechanical approach. Eur Spine J 2011;20(Suppl 5):578-85.




10. Dumpa SR, Shetty AP, Aiyer SN, et al. Reciprocal changes in sagittal alignment in adolescent idiopathic scoliosis patients following strategic pedicle screw fixation. Asian Spine J 2018;12:300-8.




11. Nakashima H, Kanemura T, Satake K, et al. Changes in sagittal alignment following short-level lumbar interbody fusion: comparison between posterior and lateral lumbar interbody fusions. Asian Spine J 2019;13:904-12.




12. Kim KR, Le Huec JC, Jang HJ, et al. Which is more predictive value for mechanical complications: fixed thoracolumbar alignment (T1 pelvic angle) versus dynamic global balance parameter (Odontoid-Hip Axis Angle). Neurospine 2021;18:597-607.




13. Lafage R, Challier V, Liabaud B, et al. Natural head posture in the setting of sagittal spinal deformity: validation of chinbrow vertical angle, slope of line of sight, and McGregor’s slope with health-related quality of life. Neurosurgery 2016;79:108-15.

14. Le Huec JC, Saddiki R, Franke J, et al. Equilibrium of the human body and the gravity line: the basics. Eur Spine J 2011;20(Suppl 5):558-63.




15. Ha Y, Schwab F, Lafage V, et al. Reciprocal changes in cervical spine alignment after corrective thoracolumbar deformity surgery. Eur Spine J 2014;23:552-9.




16. Smith JS, Shaffrey CI, Lafage V, et al. Spontaneous improvement of cervical alignment after correction of global sagittal balance following pedicle subtraction osteotomy. J Neurosurg Spine 2012;17:300-7.


17. Hasegawa K, Okamoto M, Hatsushikano S, et al. Standing sagittal alignment of the whole axial skeleton with reference to the gravity line in humans. J Anat 2017;230:619-30.




18. Protopsaltis TS, Scheer JK, Terran JS, et al. How the neck affects the back: changes in regional cervical sagittal alignment correlate to HRQOL improvement in adult thoracolumbar deformity patients at 2-year follow-up. J Neurosurg Spine 2015;23:153-8.


19. Hyun SJ, Kim KJ, Jahng TA. The differential effect of cervical kyphosis correction surgery on global sagittal alignment and health-related quality of life according to head- and trunkbalanced subtype. J Neurosurg Spine 2021 Apr 2:1-10. https://doi.org/10.3171/2020.9.SPINE201309. [Epub].



20. Mizutani J, Strom R, Abumi K, et al. How cervical reconstruction surgery affects global spinal alignment. Neurosurgery 2019;84:898-907.



21. Mizutani J, Verma K, Endo K, et al. Global spinal alignment in cervical kyphotic deformity: the importance of head position and thoracolumbar alignment in the compensatory mechanism. Neurosurgery 2018;82:686-94.



22. Park EJ, Chung S, Min WK. Reciprocal change of occipitocervical parameters after anterior cervical discectomy and fusion. Sci Rep 2021;11:5744.




23. Lafage R, Smith JS, Fong AM, et al. Proximal and distal reciprocal changes following cervical deformity malalignment correction. J Neurosurg Spine 2022 May 6:1-8. https://doi.org/10.3171/2022.2.SPINE211316. [Epub].

24. Khalil N, Bizdikian AJ, Bakouny Z, et al. Cervical and postural strategies for maintaining horizontal gaze in asymptomatic adults. Eur Spine J 2018;27:2700-9.



25. Pan Z, Xi Y, Huang W, et al. Independent correlation of the C1-2 Cobb angle with patient-reported outcomes after correcting chronic atlantoaxial instability. Neurospine 2019;16:267-76.




26. Kim JT, Lee HJ, Choi DY, et al. Sequential alignment change of the cervical spine after anterior cervical discectomy and fusion in the lower cervical spine. Eur Spine J 2016;25:2223-32.



27. Lee JK, Hyun SJ, Kim KJ. Odontoid incidence: a novel cervical parameter influencing cervical alignment from top to bottom. Neurospine 2022;19:463-71.




28. Kang KB, Kim YJ, Muzaffar N, et al. Changes of Sagittal spinopelvic parameters in normal koreans with age over 50. Asian Spine J 2010;4:96-101.



29. Schwab F, Lafage V, Boyce R, et al. Gravity line analysis in adult volunteers: age-related correlation with spinal parameters, pelvic parameters, and foot position. Spine (Phila Pa 1976) 2006;31:E959-67.

30. Ferrero E, Liabaud B, Challier V, et al. Role of pelvic translation and lower-extremity compensation to maintain gravity line position in spinal deformity. J Neurosurg Spine 2016;24:436-46.


31. Roussouly P, Pinheiro-Franco JL. Biomechanical analysis of the spino-pelvic organization and adaptation in pathology. Eur Spine J 2011;20(Suppl 5):609-18.




32. Lee DH, Ha JK, Chung JH, et al. A retrospective study to reveal the effect of surgical correction of cervical kyphosis on thoraco-lumbo-pelvic sagittal alignment. Eur Spine J 2016;25:2286-93.



33. Le Huec JC, Thompson W, Mohsinaly Y, et al. Sagittal balance of the spine. Eur Spine J 2019;28:1889-905.



34. Faro FD, Marks MC, Pawelek J, et al. Evaluation of a functional position for lateral radiograph acquisition in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2004;29:2284-9.


35. Deschenes S, Charron G, Beaudoin G, et al. Diagnostic imaging of spinal deformities: reducing patients radiation dose with a new slot-scanning X-ray imager. Spine (Phila Pa 1976) 2010;35:989-94.

36. Dubousset J, Charpak G, Dorion I, et al. Le systeme EOS. Nouvelle imagerie osteo-articulaire basse dose en position debout. e-Mém Acad natl chir 2005;4:22-7.
37. Kuntz C 4th, Shaffrey CI, Ondra SL, et al. Spinal deformity: a new classification derived from neutral upright spinal alignment measurements in asymptomatic juvenile, adolescent, adult, and geriatric individuals. Neurosurgery 2008;63(3 Suppl):25-39.

38. Sugrue PA, McClendon J Jr, Smith TR, et al. Redefining global spinal balance: normative values of cranial center of mass from a prospective cohort of asymptomatic individuals. Spine (Phila Pa 1976) 2013;38:484-9.

39. Hasegawa K, Okamoto M, Hatsushikano S, et al. Normative values of spino-pelvic sagittal alignment, balance, age, and health-related quality of life in a cohort of healthy adult subjects. Eur Spine J 2016;25:3675-86.



40. Lee SH, Son ES, Seo EM, et al. Factors determining cervical spine sagittal balance in asymptomatic adults: correlation with spinopelvic balance and thoracic inlet alignment. Spine J 2015;15:705-12.


41. Yoshimoto H, Ito M, Abumi K, et al. A retrospective radiographic analysis of subaxial sagittal alignment after posterior C1-C2 fusion. Spine (Phila Pa 1976) 2004;29:175-81.


42. Protopsaltis TS, Lafage R, Vira S, et al. Novel angular measures of cervical deformity account for upper cervical compensation and sagittal alignment. Clin Spine Surg 2017;30:E959-67.


43. Protopsaltis TS, Stekas N, Smith JS, et al. Surgical outcomes in rigid versus flexible cervical deformities. J Neurosurg Spine 2021 Feb 12:1-9. https://doi.org/10.3171/2020.8.SPINE191185. [Epub].



44. Yagi M, Takeda K, Machida M, et al. Discordance of gravity line and C7PL in patient with adult spinal deformity--factors affecting the occiput-trunk sagittal discordance. Spine J 2015;15:213-21.


45. Lafage V, Schwab F, Patel A, et al. Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine 2009;34:E599-606.


46. Miyamoto H, Hashimoto K, Ikeda T, et al. Effect of correction surgery for cervical kyphosis on compensatory mechanisms in overall spinopelvic sagittal alignment. Eur Spine J 2017;26:2380-5.



































