 |
 |
- Search
|
|
||
Abstract
Objective
The objective of this study is to assess differences in complication profiles between 3-level posterior column osteotomy (PCO) and single-level pedicle subtraction osteotomy (PSO) as both are reported to provide similar degrees of sagittal correction.
Methods
The PearlDiver database was queried retrospectively using International Classification of Disease, 9th and 10th edition and Current Procedural Terminology codes to identify patients who underwent PCO or PSO for degenerative spine disease. Patients under age 18 or with history of spinal malignancy, infection, or trauma were excluded. Patients were separated into 2 cohorts, 3-level PCO or single-level PSO, matched at a 1:1 ratio based on age, sex, Elixhauser comorbidity index, and number of fused posterior segments. Thirty-day systemic and procedure-related complications were compared.
Results
Matching resulted in 631 patients for each cohort. PCO patients had decreased odds of respiratory (odds ratio [OR], 0.58; 95% confidence interval [CI], 0.43–0.82; p = 0.001) and renal complications (OR, 0.59; 95% CI, 0.40–0.88; p = 0.009) compared to PSO patients. There was no significant difference in cardiac complications, sepsis, pressure ulcer, dural tear, delirium, neurologic injuries, postoperative hematoma, postoperative anemia, or overall complications.
Conclusion
Patients who undergo 3-level PCO have decreased respiratory and renal complications compared to single-level PSO. No differences were found in the other complications studied. Considering both procedures achieve similar sagittal correction, surgeons should be aware that 3-level PCO offers an improved safety profile compared to single-level PSO.
Adult spinal deformity (ASD) is a complex condition that may be disabling and have a negative impact on quality of life, especially when severe. Spinal deformity may present with pathological curvature in both sagittal and coronal planes, and the thoracolumbar spine is most frequently impacted. Symptoms and treatment goals may vary with patient age, with older patients often presenting with pain and neurologic symptoms and younger patients often presenting with primarily cosmetic concern. The goal of treatment for all patients is to achieve balance in all planes, alleviate pain, and prevent further deformity or recurrence [1,2].
Fortunately, when a deformity cannot be treated by standard approaches such as instrumentation and ligament release, osteotomies provide an effective form of surgical intervention. Vertebral osteotomies can be performed via anterior approach, combined anteriorposterior approach, or posterior only approach, the latter of which has gained greater popularity in recent years [1,2].
Two of the most commonly used posteriorapproach osteotomy techniques are the posterior column osteotomy (PCO) and the pedicle subtraction osteotomy (PSO). The PCO was first described by Smith-Petersen in 1945 as a 1- to 2-level osteotomy treatment for ankylosing spondylosis [3]. Ponte et al. and several others then began advocating for the use of multilevel PCO in the treatment of ankylosing spondylitis induced kyphosis, as well as Scheuermann’s kyphosis [1,4]. PCO allows for both sagittal and coronal correction and involves removal of all posterior ligaments as well as facetectomy in order to allow for posterior compression of the osteotomy. For each level of the spinal column an PCO is performed on, a range of 9.3° to 10.7° of correction is achieved, with a ratio of approximately 1° of correction for every 1 mm of bone resected [2,5,6].
PSO is a transpedicular wedge osteotomy that may also provide significant sagittal and coronal correction in spinal deformity. The PSO was first described by Thomasen in 1985 for correction of ankylosing spondylosis-induced kyphosis, though Heining et al. described a variant of the PSO in the same year [7,8]. In the PSO, after the transpedicular wedge is removed, the posterior spine is shortened using the anterior spine as a hinge to close the osteotomy and correct the deformity. Depending on the level of resection, a single-level of PSO results in 30° to 40° of correction [5,6,9].
Comparisons between any level PCO and PSO have had mixed results, with one meta-analysis reporting a similar therapeutic ability for the correction of thoracolumbar deformity, and another meta-analysis reporting a mean of 8.74° greater corrective ability of PSO [10,11]. However, considering that single and double level PSO’s were included, this finding is understandable. In terms of complications, PCO is a generally simpler and less labor-intensive procedure with a mean of 806 mL less blood loss than PSO [10]. The rate of neurologic and system complications was found to be similar between the procedures [10,11].
Given the cited ranges of correction, a 3-level PCO may provide a similar therapeutic effect as a single-level PSO of at least 30° of correction. However, the complication profile between these procedures has not been extensively investigated. Cho et al. [9] compared 3-level PCO (n = 30) and single-level PSO (n = 41) in the correction of sagittal imbalance in kyphosis, finding identical degrees of correction and operating time. There was, however, a greater chance of overcorrecting the patient into concavity with PCO, and substantially greater amount of blood loss in PSO. Additionally, Lau et al. [12] retrospectively compared PCO and 3-column osteotomy via PSO in the correction of cervicothoracic deformity in 95 patients. There was no significant difference in complication rates in this study, although the procedures were performed for different indications in the separate study groups. Considering the 2 procedures achieve similar sagittal correction, the purpose of the current study is to thoroughly assess the difference in complication profiles between 3-level PCO and single-level PSO and to assess utilization trends between the 2 procedures via retrospective analysis of a national database.
Patients were identified using the PearlDiver Mariner Database (PearlDiver Technologies, Fort Wayne, IN, USA), which includes records from more than 90 million patients from 2010 to 2020. The database includes inpatient and outpatient records of demographics, diagnoses, and procedures from both private and public insurance. Informed consent was waived due to the retrospective nature of the study and Institutional Review Board approval was not required as the database is deidentified.
Using International Classification of Disease (ICD), 9th (ICD-9) and 10th (ICD-10) edition and Current Procedural Terminology codes, patients with degenerative spinal disease were identified (Supplementary Table 1). Patients were then separated into 2 cohorts based on the index procedure that they received for their degenerative spine disease: (1) 3-level PCO or (2) single-level PSO. The 2 treatment cohorts were then further categorized based on the number of fused posterior segments: (1) 2 segments, (2) 3 to 6 segments, (3) 7 to 12 segments, and (4) 13 or more segments. Patients were excluded if they were under 18 years of age, if they had a history of spinal malignancy, spinal infection or spinal trauma, or if they underwent a posterior fusion of less than 3 segments.
The primary outcomes of this study were systemic and procedure-related complications within 30 days of the index procedure. The following complications were assessed: wound complications, venous thromboembolism (VTE), stroke, respiratory complications (pneumonia, acute respiratory failure), cardiac complications (myocardial infarction, acute heart failure, cardiogenic shock), renal complications (acute renal failure, urinary tract infection, renal infarction), sepsis, pressure ulcer, dural tear, delirium, neurologic injuries (injury to spinal cord or nerve roots, plegias, cauda equina syndrome, radiculopathies), postoperative hematoma, and postoperative anemia. Secondary outcomes included patient age, sex, and year of procedure to assess trends in 3-level PCO compared to single-level PSO.
Data normality was assessed and continuous variables were analyzed using Student t-test or Mann-Whitney U-test for parametric and nonparametric distributions respectively. To compare rates of complications between PCO and PSO cohorts, the 2 cohorts were matched at a 1:1 ratio based on age, sex, Elixhauser comorbidity index (ECI) and number of fused posterior segments. The rates of complications in the 2 matched cohorts were then compared using chi-square tests. Odds ratios are reported with 95% confidence intervals with an alpha of 0.05.
Among patients with a diagnosis of degenerative spine disease, a total of 4,582 patients underwent PCO while 675 underwent PSO. The majority of patients in both PCO and PSO cohorts were female (60.6% vs. 63.3%, p = 0.92) and under age 65 (58.9% vs. 60.2%). Age distribution was, however, significantly different between groups, with PCO being utilized more commonly within younger age groups (p < 0.001) (Table 1). Utilization rates for PSO overall increased from 38 in 2010 to 101 in 2017 (+166%), followed by a decline (-59.4%) in procedure volume to 41 cases in 2021. In contrast, PCO utilization maintained a steady increase from 246 cases in 2010 to 665 by end of 2019 (+170% overall); PCO utilization, however, similarly declined in 2020 to 475 procedures (-28.7%), albeit to a lesser degree compared to PSO. Annual utilization trends for PCO and PSO are depicted in Fig. 1 with case numbers further stratified by number of involved segments in Table 1.
In the PCO cohort, 2,534 (55.3%) had 3 to 6 fused segments, 1,470 (32.1%) had 7 to 12 fused segments, and 578 (12.6%) had 13 or more fused segments. In the PSO cohort, 229 (32.6%) had 3 to 6 fused segments, 359 (51.1%) had 7 to 12 fused segments, and 114 (16.2%) had 13 or more fused segments.
In the PCO cohort, a total of 2,216 patients (48.4%) experienced a 30-day complication (Table 2). The most prevalent complications were postoperative anemia (1,178; 25.7%) and neurological injury (819, 16.6%). In the PSO cohort, a total of 390 patients (57.8%) experienced a 30-day complication, wherein the most prevalent complications were postoperative anemia (220, 32.6%) and respiratory complications (127, 18.8%).
The PCO and PSO cohorts underwent 1:1 nearest neighbor propensity-score matching to account for age, sex, ECI, and number of segments fused as covariates. There were 631 patients in both cohorts (Table 3). In the chi-square analysis, PCO patients had decreased odds of having a respiratory complication (OR, 0.58; 95% CI, 0.43–0.82; p = 0.001) or renal complication (OR, 0.59; 95% CI, 0.40–0.88; p = 0.009) when compared to PSO patients. Notably, there were no significant differences between PCO and PSO with respect to postoperative anemia (28.1% vs. 30.4%, p = 0.353) and neurological injury (16% vs. 14.4%, p = 0.433), which were the most prevalent complications seen with PCO prior to propensity-matching. No other differences were seen for rates of 30-day wound complications, VTE, cardiac complications, sepsis, delirium (all p > 0.05). We were unable to determine differences in stroke, hematoma, pressure ulceration, and dural tear due to insufficient power.
In the present study, patients who underwent single-level PSO were found to have increased rates of 30-day respiratory and renal complications when compared to those who underwent 3-level PCO when matched based on age, sex, ECI, and segments fused. There was no difference in rate of 30-day wound complications, VTE, anemia, cardiac, sepsis, delirium, and neurologic complications. Overall, there was a 49.9% complication rate in patients undergoing 3-level PCO and a 55.2% complication rate in patients undergoing single-level PSO, which was not significantly different.
While there has been an abundance of published studies discussing the differences in sagittal correction between PCO and PSO, data on complication rates between PCO and PSO is limited [6,9,13-15]. Liu et al. [16] published a meta-analysis of patients with ankylosing spondylitis undergoing either PCO or PSO and compared outcomes, including medical complications. In total, 441 patients were included in the PCO cohort and 512 in the PSO cohort. The majority of patients underwent single-level procedures. They found no significant difference in terms of dural tear, neurologic complication, implant related complications, infection, aortic rupture, death, and total complications. Average blood loss was found to be 2,012 mL in the PSO cohort and 1,307 mL in the PCO cohort. Operative time was also found to be longer for PSO (4.0 hours vs. 3.1 hours).
Hu et al. [10] published a similar meta-analysis comparing 120 patients who underwent PCO to 300 patients who underwent PSO for the treatment of ankylosing spondylitis. The majority of patients underwent single or 2-level PCO and single-level PSO. Similar to Liu et al. [16], they found that PSO had increased blood loss compared to PCO. There was no difference in rates of neurologic, dural, or systemic complications.
The present matched cohorts comparing 3-level PCO to single-level PSO is the largest study to date to assess systemic complications and the safety profile between these 2 procedures. We found the only significant differences in 30-day complications to be decreased respiratory and renal complications in the PCO cohort. There was no difference in postoperative anemia, which differs from previous reports stating that PSO leads to increased blood loss compared to PCO [10,16]. However, these studies largely compared single-level PCO to single-level PSO, whereas the present study directly compared 3-level PCO to single-level PSO. Furthermore, postoperative anemia does not necessarily correlate with intraoperative blood loss. While our study observed a higher incidence of neurological complications amongst with 3-level PCO (16.6%) than that reported within the literature, this was likely attributed to several contributive factors including our sole inclusion of 3-level procedures compared to single-level procedures in other studies [5], reporting of transient neuropraxias within the immediate postoperative period, and inherent discrepancies associated with use of ICD coding across institutions. Nonetheless, incidence of neurological injury remained comparable between matched PCO and PSO cohorts, which is concordant with other studies comparing multilevel PCO and PSO for deformity correction [17]. Additionally, we provide data on 30-day cardiac complications, wound complications, VTE rates, sepsis, and delirium, which have not been reported on previously in the literature. We did not find any significant differences between the 2 cohorts in terms of these complications.
Trends of 3-level PCO compared to single-level PSO were also assessed. We found that the rate of 3-level PCO increased from 2010 to 2019, whereas PSO increased from 2010 to 2017 and then saw a steady decline. Both procedures decreased in 2020, likely due to the COVID-19 pandemic [18]. The decline in utilization of PSO starting 2017 and the steady increase in PCOs likely indicates that more surgeons are utilizing PCOs when possible, perhaps due to the decreased blood loss reported in the literature and because PCO is purported to be less labor intensive [6,9]. While PCOs seemingly offer a technique which place less physiological demands on patients undergoing ASD surgery, it is also important to highlight the advent of minimally invasive techniques such as mini-open PSO, which could further improve clinical outcomes in ASD patients who are appropriately indicated [19].
There are several limitations to this study. Like all database studies, it is inherently limited by reliance on accurate medical coding. Second, we were unable to assess sagittal correction between the 2 procedures, as radiographic data is not available in the database. Third, we did not report on reoperation or hardware failure as it was outside the scope of this study. While the use of ICD-9 and ICD-10 diagnosis codes precluded our study from accurately evaluating mechanical complication rates, further research incorporating machine-learning based algorithms could substantially improve risk prediction amongst various osteotomy techniques [20]. Doing so would additionally refine indications for patients undergoing ASD surgery and would better individualize operative treatment strategies for this complex patient population. Nonetheless, despite these limitations, our study is the first to assess nationwide PCO and PSO trends in which we are aware of, and presents an important area of further research.
In conclusion, 3-level PCO utilization increased steadily throughout the study period, whereas single-level PSO utilization peaked in 2017 and has since seen a steady decline. Patients who undergo 3-level PCO are at decreased risk of renal and respiratory complications compared to patients undergoing single-level PSO. There was no difference in rate of 30-day wound, VTE, anemia, cardiac, sepsis, delirium, and neurologic, and overall complications. Considering the 2 procedures achieve similar sagittal correction, it is important for surgeons to be aware that 3-level PCO has an improved safety profile compared to single-level PSO.
Supplementary Material
Supplementary Table 1 can be found via https://doi.org/10.14245/ns.2346222.111.
Supplementary Table 1.
All International Classification of Disease, 9th and 10th edition and Current Procedural Terminology (CPT) codes used
NOTES
Conflict of Interest
Emily S. Mills MD, Kevin Mertz BS, Ethan Faye BS, Jennifer A. Bell MD, Andy T. Ton BS have nothing to disclose. Jeffrey C. Wang has received intellectual property royalties from Zimmer Biomet, NovApproach, SeaSpine, and DePuy Synthes. Ram K. Alluri, MD discloses has received grant funding from NIH, consulting fees from HIA Technologies, and payment from Eccentrial Robotics for lectures and presentations. Raymond J. Hah MD has received grant funding from SI bone, consulting fees from NuVasive, and support from the North American Spine Society to attend meetings.
Fig. 1.
Yearly trends in 3-level posterior column osteotomy (PCO) versus single-level pedicle subtraction osteotomy (PSO) from 2010–2020.
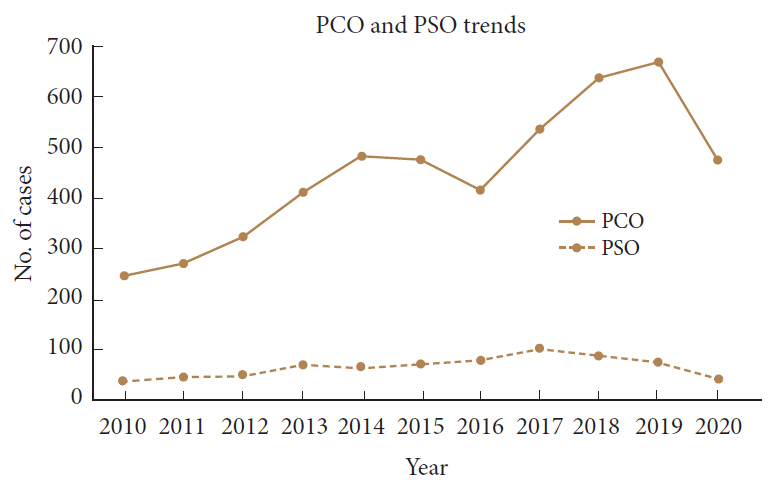
Table 1.
Demographic data for patients who underwent 3-level posterior column osteotomy (PCO) and single-level pedicle subtraction osteotomy (PSO)
| Variable |
3-Level PCO (n) |
Single-level PSO (n) |
p-value | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| All (n = 4,582) | 3 to 6* (n=2,534) | 7 to 12* (n=1,470) | 13 or more* (n = 578) | All (n=675) | 3 to 6* (n=202) | 7 to 12* (n=359) | 13 or more* (n=114) | |||
| Age (yr) | < 0.001 | |||||||||
| 15–19 | 27 (0.6) | < 10 | < 10 | 17 (2.9) | 15 (2.2) | < 10 | < 10 | < 10 | ||
| 20–24 | 81 (1.7) | < 10 | 36 (2.4) | 40 (6.9) | 15 (2.2) | < 10 | < 10 | < 10 | ||
| 25–29 | 65 (1.4) | 12 (0.5) | 26 (1.8) | 20 (3.5) | 15 (2.2) | < 10 | < 10 | < 10 | ||
| 30–34 | 80 (1.7) | 28 (1.1) | 28 (1.9) | 19 (3.3) | 15 (2.2) | < 10 | < 10 | < 10 | ||
| 35–39 | 99 (2.2) | 42 (1.7) | 23 (1.6) | 16 (2.8) | 10 (1.4) | < 10 | < 10 | 0 (0) | ||
| 40–44 | 205 (4.5) | 124 (4.9) | 36 (2.4) | 26 (4.5) | 15 (2.2) | < 10 | < 10 | < 10 | ||
| 45–49 | 297 (6.5) | 154 (6.1) | 54 (3.7) | 40 (6.9) | 21 (3.1) | < 10 | 11 (3.1) | < 10 | ||
| 50–54 | 414 (9.0) | 237 (9.4) | 104 (7.1) | 48 (8.3) | 45 (6.6) | 17 (8.4) | 23 (6.4) | < 10 | ||
| 55–59 | 644 (14.1) | 345 (13.6) | 177 (12.0) | 87 (15.1) | 89 (13.2) | 21 (10.4) | 47 (13.1) | 21 (18.4) | ||
| 60– 64 | 789 (17.2) | 418 (16.5) | 254 (17.3) | 82 (14.2) | 167 (24.7) | 54 (26.7) | 86 (24.0) | 27 (23.7) | ||
| 65–69 | 836 (18.2) | 430 (17.0) | 268 (18.2) | 76 (13.1) | 109 (16.1) | 35 (17.3) | 57 (15.9) | 17 (14.9) | ||
| 70–74 | 878 (19.2) | 460 (18.2) | 290 (19.7) | 69 (11.9) | 140 (20.7) | 49 (24.3) | 76 (21.2) | 15 (13.2) | ||
| 75–79 | 447 (9.8) | 236 (9.3) | 151 (10.3) | 34 (5.9) | 65 (9.6) | 21 (10.4) | 39 (10.9) | < 10 | ||
| 80– 84 | 57 (1.2) | 37 (1.5) | 15 (1.0) | < 10 | < 10 | < 10 | < 10 | < 10 | ||
| Sex | 0.921 | |||||||||
| Female | 2,778 (60.6) | 1,405 (55.4) | 939 (63.9) | 434 (75.1) | 427 (63.3) | 137 (67.8) | 214 (59.6) | 76 (66.7) | ||
| Male | 1,804 (39.4) | 1,129 (44.6) | 531 (36.1) | 144 (24.9) | 275 (40.7) | 92 (45.5) | 145 (40.4) | 38 (33.3) | ||
| Year | 0.002 | |||||||||
| 2010 | 246 | 91 | 67 | 34 | 38 | 12 | 14 | < 10 | ||
| 2011 | 270 | 117 | 69 | 39 | 45 | 12 | 20 | 11 | ||
| 2012 | 323 | 159 | 84 | 37 | 49 | 14 | 24 | < 10 | ||
| 2013 | 411 | 206 | 112 | 42 | 70 | 21 | 36 | < 10 | ||
| 2014 | 482 | 260 | 135 | 44 | 66 | 18 | 33 | 13 | ||
| 2015 | 474 | 254 | 140 | 53 | 70 | 21 | 39 | 12 | ||
| 2016 | 415 | 219 | 144 | 49 | 78 | 27 | 38 | 11 | ||
| 2017 | 534 | 272 | 162 | 71 | 101 | 37 | 47 | 16 | ||
| 2018 | 635 | 342 | 201 | 74 | 88 | 22 | 41 | 13 | ||
| 2019 | 665 | 359 | 206 | 83 | 76 | 31 | 42 | < 10 | ||
| 2020 | 475 | 256 | 152 | 52 | 41 | 14 | 25 | < 10 | ||
Table 2.
Postoperative complication rates of patients who underwent 3-level posterior column osteotomy (PCO) and single-level pedicle subtraction osteotomy (PSO) across varying number of posterior segments fused
| Variable |
3-Level PCO (n) |
Single-level (PSO) (n) |
||||||
|---|---|---|---|---|---|---|---|---|
| All | 3 to 6* | 7 to 12* | 13 or more* | All | 3 to 6* | 7 to 12* | 13 or more* | |
| Wound complications | 153 | 75 | 55 | 23 | 26 | < 10 | 15 | < 10 |
| VTE | 146 | 55 | 63 | 25 | 26 | < 10 | < 10 | < 10 |
| Stroke | 30 | < 10 | 12 | < 10 | < 10 | < 10 | < 10 | < 10 |
| Hematoma | 36 | 15 | 15 | < 10 | < 10 | 0 | < 10 | < 10 |
| Anemia | 1,178 | 489 | 478 | 213 | 220 | 59 | 125 | 47 |
| Transfusion | 98 | 50 | 35 | 16 | 16 | < 10 | < 10 | < 10 |
| Respiratory complications | 429 | 123 | 194 | 116 | 127 | 34 | 63 | 34 |
| Cardiac complications | 98 | 39 | 35 | 18 | 24 | < 10 | 13 | < 10 |
| Renal complications | 351 | 154 | 138 | 55 | 75 | 25 | 36 | 14 |
| Sepsis | 85 | 35 | 40 | < 10 | 13 | < 10 | < 10 | < 10 |
| All | 2,216 | 1,034 | 789 | 325 | 390 | 119 | 200 | 72 |
Table 3.
Postoperative complication rates of matched cohorts of patients who underwent 3-level posterior column osteotomy (PCO) and single-level pedicle subtraction osteotomy (PSO)
| Variable | 3-Level PCO (n) | Single-level PSO (n) | OR | 95% CI | p-value |
|---|---|---|---|---|---|
| Wound complications | 29 (4.6) | 25 (4.0) | 1.168 | 0.534–1.714 | 0.578 |
| VTE | 14 (2.2) | 25 (4.0) | 0.550 | 0.384–1.318 | 0.078 |
| Stroke | < 10 | < 10 | - | - | - |
| Hematoma | < 10 | < 10 | - | - | - |
| Anemia | 177 (28.1) | 192 (30.4) | 0.891 | 0.734–1.201 | 0.353 |
| Transfusion | 12 (1.9) | 15 (2.4) | 0.891 | 0.369–1.715 | 0.353 |
| Respiratory complications | 74 (11.7) | 116 (18.4) | 0.590 | 0.431–0.818 | 0.001* |
| Cardiac complications | 19 (3.0) | 20 (3.2) | 0.948 | 0.596–2.045 | 0.871 |
| Renal complications | 44 (7.0) | 71 (11.3) | 0.591 | 0.399–0.876 | 0.009* |
| Sepsis | 15 (2.4) | 12 (1.9) | 1.256 | 0.583–2.708 | 0.560 |
| Pressure ulcer | < 10 | < 10 | - | - | - |
| Dural tear | < 10 | < 10 | - | - | - |
| Delirium | 37 (5.9) | 52 (8.2) | 0.694 | 0.495–1.181 | 0.101 |
| Neurologic injury | 101 (16.0) | 91 (14.4) | 1.131 | 0.792–1.405 | 0.433 |
| All | 315/631 (49.9) | 348/631 (55.2) | 0.811 | 0.649–1.011 | 0.063 |
REFERENCES
1. Enercan M, Ozturk C, Kahraman S, et al. Osteotomies/spinal column resections in adult deformity. Eur Spine J 2013;22 Suppl 2(Suppl 2):S254-64.




2. Kose KC, Bozduman O, Yenigul AE, et al. Spinal osteotomies: indications, limits and pitfalls. EFORT Open Rev 2017;2:73-82.




3. Smith-Petersen MN, Larson CB, Aufranc OE. Osteotomy of the spine for correction of flexion deformity in rheumatoid arthritis. Clin Orthop Relat Res 1969;66:6-9.


4. Ponte A, Vero B, Siccardi GL. Surgical treatment of Scheuermann’s kyphosis. In: Winter RBet al., editors. Progress in spinal pathology: kyphosis. Bologna (Italy): Aulo Gaggi; 1984. p. 75-80.
5. Dorward IG, Lenke LG. Osteotomies in the posterior-only treatment of complex adult spinal deformity: a comparative review. Neurosurg Focus 2010;28:E4.

6. Bridwell KH. Decision making regarding Smith-Petersen vs. pedicle subtraction osteotomy vs. vertebral column resection for spinal deformity. Spine (Phila Pa 1976) 2006;31(19 Suppl):S171-8.


7. Thomasen E. Vertebral osteotomy for correction of kyphosis in ankylosing spondylitis. Clin Orthop Relat Res 1985;194:142-52.

8. Luque ER. Segmental spinal instrumentation for correction of scoliosis. Clin Orthop Relat Res 1982;163:192-8.

9. Cho KJ, Bridwell KH, Lenke LG, et al. Comparison of Smith-Petersen versus pedicle subtraction osteotomy for the correction of fixed sagittal imbalance. Spine (Phila Pa 1976) 2005;30:2030-7. discussion 2038.


10. Hu X, Thapa AJ, Cai Z, et al. Comparison of Smith-Petersen osteotomy, pedicular subtraction osteotomy, and poly-segmental wedge osteotomy in treating rigid thoracolumbar kyphotic deformity in ankylosing spondylitis a systematic review and meta-analysis. BMC Surg 2016;16:4.



11. Bao H, He S, Liu Z, et al. Will immediate postoperative imbalance improve in patients with thoracolumbar/lumbar degenerative kyphoscoliosis? A comparison between Smith-Petersen osteotomy and pedicle subtraction osteotomy with an average 4 years of follow-up. Spine (Phila Pa 1976) 2015;40:E293-300.


12. Lau D, Deviren V, Joshi RS, et al. Comparison of perioperative complications following posterior column osteotomy versus posterior-based 3-column osteotomy for correction of rigid cervicothoracic deformity: a single-surgeon series of 95 consecutive cases. J Neurosurg Spine 2020 May 7:1-10. doi: 10.3171/2020.3.SPINE191330. [Epub].


13. Lee KY, Lee JH, Kang KC, et al. Minimally invasive multilevel lateral lumbar interbody fusion with posterior column osteotomy compared with pedicle subtraction osteotomy for adult spinal deformity. Spine J 2020;20:925-33.


14. McClendon J Jr, Koski TR, Ondra SL, et al. Sagittal imbalance: multiple Smith-Petersen osteotomies versus pedicle subtraction osteotomies. In: Jandial R, Garfin SRet al., editors. Best evidence for spine surgery: 20 cardinal cases. Philadelphia (PA): Elsevier Saunders; 2012. p. 210-23.
15. Zhu Z, Wang X, Qian B, et al. Loss of correction in the treatment of thoracolumbar kyphosis secondary to ankylosing spondylitis: a comparison between smith-petersen osteotomies and pedicle subtraction osteotomy. J Spinal Disord Tech 2012;25:383-90.

16. Liu H, Yang C, Zheng Z, et al. Comparison of Smith-Petersen osteotomy and pedicle subtraction osteotomy for the correction of thoracolumbar kyphotic deformity in ankylosing spondylitis: a systematic review and meta-analysis. Spine (Phila Pa 1976) 2015;40:570-9.

17. Han S, Hyun SJ, Kim KJ, et al. Multilevel posterior column osteotomies are not inferior for the correction of rigid adult spinal deformity compared with pedicle subtraction osteotomy. World Neurosurg 2017;107:839-45.


18. Farid Y, Schettino M, Kapila AK, et al. Decrease in surgical activity in the COVID-19 pandemic: an economic crisis. Br J Surg 2020;107:e300.





- TOOLS
- Related articles in NS
-
Journal Impact Factor 3.2



























