 |
 |
- Search
|
|
||
Abstract
Objective
To evaluate the biomechanical stability of anterior transarticular crossing screw (ATCS) and compare it with anterior transarticular screw (ATS) which may provide basic evidence for clinical application.
Methods
Eight human fresh cadaveric specimens (occiput-C4) were tested with 5 conditions including the intact status, the injury status (type II odontoid fracture), the injury+ATS fixation status (traditional bilateral ATS fixation); the injury+unilateral ATCS fixation status; and the injury+bilateral ATCS fixation status. Specimens were applied to a pure moment of 1.5 Nm in flexion-extension, lateral bending, and axial rotation, respectively. The range of motions (ROMs) and the neutral zones (NZs) of C1 to C2 segment were calculated and compared between 5 status.
Results
ATS and ATCS fixations significantly reduced the motions in all directions when compared with the intact and injury statues (p < 0.05). In flexion-extension, the ROMs of ATS, unilateral ATCS, and bilateral ATCS were 4.7° ±2.5°, 4.1° ±1.9°, and 3.2° ±1.2°, respectively. Bilateral ATCS resulted in a significant decrease in ROM in flexion-extension when compared with ATS and unilateral ATCS (p = 0.035 and p = 0.023). In lateral bending and axial rotation, there was no significant difference in ROM between the 3 fixations (p > 0.05). Three fixations resulted in similar NZs in all directions (p > 0.05).
Atlantoaxial instability can arise from numerous conditions, such as trauma, malignancy, rheumatoid arthritis, congenital anomalies, inflammation, degenerative joint disease, or infectious disease. Due to the intricate and vital structures in the vicinity, surgical fixation is necessary to provide robust stability and security in this region. The anterior transarticular screw (ATS) fixation for atlantoaxial instability is a classic technique that Barbour [1] first described in 1971 and was anatomically studied by Lu et al. [2] in 1998. Afterward, no further relevant studies were published until 2003 when Reindl et al. [3] reported a case of traumatic instability using the classic retropharyngeal Smith-Robinson approach. Two years later, they conducted a biomechanical study to demonstrate the effectiveness and feasibility of this technique in atlantoaxial stabilization [4]. Subsequently, this technique was used to treat various atlantoaxial disorders with satisfactory postoperative outcomes, and now ATS fixation is widely used [5-10].
However, in some unique clinical cases, such as atlantoaxial facet splitting, atlantoaxial lateral mass loss, screw cut-out at the atlantoaxial facet, fracture of the anterior rim of the C2 articular, or high-riding vertebral artery, traditional fixation techniques may not be feasible [11,12]. This may be due to fewer landmarks for safe and effective repositioning of ATS [4,13]. We have previously proposed anterior transarticular crossing screw (ATCS) fixation through anatomical and morphometric studies in adults and children, demonstrating the safety and feasibility of this technique [11,14]. The results showed that ATCS has a longer screw purchase and can achieve significantly stronger screw holding capability. ATCS may provide a useful supplement or salvage procedure for ATS. However, it has not been evaluated from a biomechanical perspective. Therefore, the present study aims to evaluate the biomechanical stability of ATCS and compare it with conventional ATS.
Eight specimens (Occiput-C4) were collected from fresh-frozen human cadavers. The sex and age of the donors were unknown, and specimens with osteoporosis (T value < 2.5) were excluded by bone mineral density examination. Routine anteroposterior and lateral x-ray examinations were performed to exclude obvious deformities, fractures, tuberculosis, tumors, and other pathological conditions in the specimens.
All specimens were stored at -20°C and thawed at room temperature overnight before the experiment. Muscle tissue was removed, and the joint capsule and ligaments were carefully preserved. The partial occipital bone and C4 vertebrae were embedded in dental stone to maintain C1–2 levels during testing. The specimens were regularly sprayed with normal saline to keep them moist.
This study was approved by the Ethic Committee of Nanfang Hospital (NFEC-2022-197).
Odontoid process was cutoff with an electric drill, a 2.5-mm diameter drill splinter, a rongeur forceps and a osteotome after testing in the intact status, resulting in a type II odontoid fracture. For ATS, the entry point was located at the midpoint of the C2 body, which is in the medial third of the C1–2 facet joint, below the sulcus on the anterior body of the C2 [4,14]. For ATCS, the entry point was set 5 mm lateral to the C2 body from the midline to the contralateral side in the coronal plane, to ensure a sufficient gap between the screw head and the C2–3 intervertebral disc, thereby mitigating the risk of adjacent level ossification [14]. In the sagittal plane, the entry point was set at the anteroinferior level of the C2 body.
The ideal direction for ATS and ATCS was toward the superolateral corner of the superior articular process of C1 on anteroposterior radiograph, leaving 2–3 mm clearance from lateral margin of the lateral mass, as shown in Figs. 1 and 2. On lateral radiographs, all screws are aimed at the superoposterior corner of C1 superior articular process [15].
During the procedure, a 1.0-mm K-wire was used to drill in a specific direction under x-ray fluoroscopy. Once the needle was inserted into the subcortical area in the atlas mass, a 2.5-mm electric drill bit was used to drill along the K-wire, and a 4-mm diameter hollow tension screw was inserted. The same procedure was then performed on the contralateral side to complete bilateral ATCS fixation for the specimen. The type of screw used in this procedure was peak summit from DePuy Spine, Johnson. The radiography of the embedded specimen after implantation verified that the fixation was satisfactory, as illustrated in Fig. 3. To minimize damage to the specimens, ATCS and ATS were randomly performed on the left or right side of each specimen.
Fig. 4 shows a custom-designed spinal testing machine [16] that applied a pure couple moment to the specimens under 5 conditions, in flexion-extension, lateral bending, and axial rotation. Each specimen was subjected to a continuous pure moment of 1.5 Nm for 3 cycle loading, with a displacement rate of 2°/sec. Data from the third cycle was used in the testing. Two optoelectronic camera systems (Certus; Northern Digital, Waterloo, ON, Canada) were used to measure the motion of the cervical spine. With an accuracy of 0.1°, this is currently the most accurate motion measurement system. The 2 cameras were angled +/- 45° toward the posterior view of the specimen to ensure that no markers were missed during motion, particularly in axial rotation. The marker carriers with 4 infrared light-emitting diodes were attached to the C1, C2, and C3. The Optotrak 3-dimensional motion measurement system was used to continuously calculate the motion of the markers, with a sampling frequency of 20 Hz. Range of motions (ROMs) and neutral zones (NZs) between C1 and C2 in flexion-extension, lateral bending, and axial rotation were calculated, respectively. To reduce the influence of the test order, the sequence of the 2 fixation procedures and the order of the 3 directions were randomized.
Each specimen was tested with following 5 configurations: (1) the intact status; (2) the injury status (type II odontoid fracture); (3) the injury+ATS fixation status (traditional bilateral ATS fixation); (4) the injury+unilateral ATCS fixation status; and (5) the injury+bilateral ATCS fixation status.
The left lateral bending and axial rotation movements were observed to be statistically similar to those on the right side (p > 0.05); therefore, an average value was calculated for both directions. To determine the differences in ROMs and NZs between the intact, injury, ATS fixation, and ATCS fixation groups in all directions, we employed 1-way analysis of variance with a Tukey post hoc test. The data were presented as mean±standard deviation, and statistical significance was set at p<0.05. All statistical analyses were performed using IBM SPSS Statistics ver. 24.0 (IBM Co., Armonk, NY, USA).
ROM refers to the degree of displacement between the maximum range of motion and the neutral position when a pure couple moment is applied. The neutral position is the state in which the spinal column experiences the least amount of stress and requires minimal force to maintain proper posture.
NZ is the section of the ROM where the load on the spine is nearly zero, and the ligaments are most relaxed, enabling a broad range of spinal motion with minimal force.
Table 1 shows the ROMs and NZs of the C1–2 segments in 5 different conditions, with a comparison between ATS, unilateral ATCS, and bilateral ATCS represented in Figs. 5 and 6. In intact status, the ROMs in flexion-extension, lateral bending, and axial rotation were 12.4°±6.7°, 3.3°±1.6°, and 63.7°±28.8°, respectively. Compared with the intact state, the ROMs of the C1–2 segments in the injury state were significantly increased in the flexion-extension, lateral bending, and axial rotation directions (26.2°±8.9°, 11.0°±3.3°, and 78.3°±10.3°, respectively) (p<0.05). After ATCS and ATS fixation, the ROMs and NZs of the fixed segments were significantly reduced compared to the intact and injured states (p<0.05). The ROMs for ATS, unilateral ATCS, and bilateral ATCS in flexion-extension were 4.7° ±2.5°, 4.1°±1.9°, and 3.2°±1.2°, respectively. Significant differences were found between bilateral ATCS and the other 2 methods (p<0.05). No significant differences were found between the 3 fixations in lateral bending or in axial rotation (p>0.05).
The NZs for the intact state were 3.2°±3.6°, 0.8°±0.8°, and 25.8°±12.5° in flexion-extension, lateral bending, and axial rotation, respectively. In all directions, the injury state increased the NZs, whereas the 3 fixation states decreased the NZs significantly when compared with the intact state (p < 0.05). After ATS fixation and bilateral ATCS fixation, the NZs reduced to 0.6°±0.5°, 0.5°±0.3° in flexion-extension, 0.3°±0.3°, 0.3°±0.5° in lateral bending, and 2.1°±4.1°, 0.8°±0.6° in axial rotation, respectively. Similarly, after unilateral ATCS fixation, the NZs were 0.4°±0.3°, 0.3°±0.5°, and 0.6°±0.5° in the respective directions. Except in direction of axial rotation (p<0.05), no significant differences were observed in NZs between the 3 conditions (p>0.05).
Atlantoaxial instability can be caused by several factors, such as trauma, tumors, rheumatoid arthritis, and infectious diseases, which often lead to severe spinal cord injury and nerve root-related abnormal manifestations [17]. The key to relieving these symptoms is to surgically stabilize the atlantoaxial complex. However, surgical treatment of the C1–2 segment has always been a challenge in spine surgery due to the complexity of the atlantoaxial joint. The atlantoaxial posterior approach, first proposed by Gallie et al. [18] in 1939, has become the mainstream posterior fixation technique after continuous development and innovation. Nonetheless, in cases with contraindications such as abnormal vertebral artery, posterior atlantoaxial structural fractures, lateral mass fractures, or patients who need a cervical operation in supine position with cardiovascular and respiratory disease, the posterior approach may not be feasible [9,15].
The use of ATS for patients with atlantoaxial instability was first reported in 1971 by Barbour [1], and its anatomic parameters were studied by Lu et al. [2] using 30 dried human cervical spines to confirm its feasibility. However, traditional ATS fixation techniques may not be possible or may fail in some unique clinical cases, such as atlantoaxial facet splitting, atlantoaxial lateral mass loss, screw cut-out the atlantoaxial facet, fracture of the anterior rim of the C2 articular, or high-riding vertebral artery. Kim et al. [19] found that traditional ATS lacks biomechanical stability in flexion and extension in specific cases. Therefore, we proposed a novel ATCS fixation technique and studied its anatomical characteristics [14]. Our study demonstrated that ATCS has a significantly longer screw purchase, which is favorable for resisting screw pullout. ATCS appears to be feasible and may become an alternative option for atlantoaxial fixation techniques. Three years later, Lvov et al. [9] performed ATCS in 2 patients and achieved good atlantoaxial joint stability in the postoperative evaluation, showing better long-term clinical outcomes. In 2020 and 2022, we designed a retrospective multiplanar computed tomography-based morphometric study to determine the morphometric characteristics and the potential trajectory of ATCS in adults and children. We comprehensively measured the range of screw lengths of ATCS, as well as screw lateral angles (LAs) and incline angles (IAs), which provide security guarantees for ATCS [11,15]. Our study showed that the longer screw length of ATCS has larger pullout strength. However, there are no biomechanical stability tests of ATCS. Therefore, this current study aims to analyze the biomechanical characteristics, including ROMs and NZs of ATS, unilateral ATCS, and bilateral ATCS fixation, to provide basic evidence for clinical application.
The results of the biomechanical stability test revealed that the ROMs after each of the 3 procedures was less than the intact and injured states with statistically significant differences. This indicates that each procedure achieved great immediate stability and satisfactory clinical efficacy. However, the distant fusion effect in body has not been observed yet. Sen et al. [4] found that the ROMs and NZs of ATS were 5.41° and 1.07° in flexionextension, 0.97° and 0.36° in lateral bending, and 1.67° and 0.47° in axial rotation, respectively. Furthermore, the ROMs of ATS collected by Lapsiwala et al. [20] were 4.89°, 0.98°, and 1.98° in the 3 directions, respectively. These data were comparable to the actual ROMs and NZs of ATS measured in this study, demonstrating the reliability of our findings. On the other hand, the ROMs of unilateral ATCS performed in this study were 4.11°, 0.82°, and 1.87° in flexion-extension, lateral bending, and axial rotation, respectively. The ROMs of bilateral ATCS were 3.20°, 0.81°, and 1.43° in flexion-extension, lateral bending, and axial rotation, respectively, indicating better stability than ATS. According to our previous anatomical findings on fresh cadaveric specimens, we found that the ATCS screw length (40.4 mm) was significantly longer than ATS (26.4 mm) (p<0.001). The ATCS screw length of C1 purchase was 14.8 mm, similar to ATS (14.9 mm), while the ATCS length of C2 purchase was 25.6 mm, longer than ATS (11.4 mm) (p<0.001) [14]. Besides, similar to our previous study, the large LAs and IAs of ATCS, up to 38.4° and 41.0°, respectively, providing more space for further bone graft on the facet surface, allowing for stronger fixation and an increased probability of bone fusion [7]. Bianco et al. [21] demonstrated that initial stiffnesses and peak pullout forces were larger in longer screws that those in shorter screws, thus it is expected that ATCS fixation is more stable than ATS fixation, consistent with our measurements.
The analysis of the ROMs for the 3 procedures demonstrated similar stability in lateral bending and axial rotation. However, we believe that unilateral ATCS is clinically advantageous for several reasons: (1) The ROM exhibits a significant decreasing trend, suggesting better stability; (2) Tian et al. [22] found that high-riding vertebral artery may results in a significantly increased risk of injury during surgical procedures, the surgical strategy is using alternative fixation methods instead of C2 pedicle screw. Uniateral ATCS allows for anterior soft tissue exposure from a unilateral incision to expose the axis. It is less invasive and utilizes the virtual space, reducing the the infection rate and the risk of contralateral soft tissue stripping and vertebral artery injury, which may accelerate postoperative rehabilitation [5]; (3) Bilateral ATCS requires higher accuracy in screw placement, making the procedure more challenging.
ATCS is more stable than ATS in flexion and extension, possibly because the atlantoaxial joint provides only 12% of the motion of the upper cervical spine in flexion and extension, whereas it provides 50% in lateral bending and axial rotation, thus strong fixation has a greater impact on stability in this direction [23]. Moreover, the 4 mm diameter hollow tension screw used in ATCS can be tightly attached to the atlantoaxial facet, which is far from the center of rotation of the vertebral body and has a longer screw length and force arm, whereas the ATS screw is near the atlantoaxial facet and lateral mass, reducing its ability to resist flexion and extension movements. However, the main structure of the axis is cancellous bone, and previous finite element analysis studies suggest that the longer screws used in ATCS may not withstand the greater stresses in the direction of lateral bending and axial rotation [24]. Therefore, although ATCS fixation can significantly reduce the ROM of lateral bending and axial rotation of the atlantoaxial spine, excessive head and neck rotation should be avoided to prevent fixation failure. A comprehensive finite element analysis of the ATCS is also needed to determine the stress and optimize the ATCS technique.
However, the present study has several limitations, which are common among studies on fresh cadaver specimens. Firstly, human cervical spine specimens are difficult to obtain in large numbers, resulting in weak statistical power. The small sample size affects the representativeness of the measurement results, and more samples are needed to verify the reliability. Secondly, the age, gender, and other specific information of the cadaver specimens in this study are unknown, and there is bias in the selection of specimens. To minimize the influence of non-treatment factors, the biomechanical test design was based on a self-control study. Thirdly, the influence of individual muscles and ligaments on spinal motion after the atlantoaxial instability operation was not considered in this experiment. Fourthly, long-term biomechanical data are also unknown as this study only tested acute stability. Fifthly, ATCS fixation technique is demanding and not every clinical surgeon can perform it accurately, which affects its practicability.
In current cadaveric biomechanical study, ATCS fixation can provide similar biomechanical stability in 3 directions compared with ATS fixation. suggesting that ATCS fixation may potentially serve as an alternative or supplemental method for treating atlantoaxial instability. Furthermore, though there is equivalent biomechanical stability between unilateral ATCS fixation and bilateral ATCS fixation, the former is more favorable due to its reliability and efficiency. Further clinical studies are needed to evaluate long-term biomechanical stability of ATCS fixation.
NOTES
ACKNOWLEDGEMENTS
We thank Zhiping Huang, BSc (from the Department of Orthopedics, Nanfang Hospital, Southern Medical University) for help with the experiments.
Fig. 1.
Artist’s illustrations showing the anterior transarticular screw (ATS) fixation and the anterior transarticular crossing screw (ATCS) fixation.

Fig. 3.
X-ray images of unilateral (A, B) and bilateral (C, D) ATCS, respectively, are shown on anteroposterior (A, C) and lateral (B, D) radiographs. All screws are aimed at the superolateral corner of C1 superior articular process; all screws are aimed at the superoposterior corner of C1 superior articular process. ATCS, anterior transarticular crossing screw; ATS, anterior transarticular screw.

Fig. 5.
Bar graph demonstrating the range of motion of C1–2 segment in all directions. *Indicates statistical difference from bilateral anterior transarticular crossing screw (ATCS) (p<0.05). Error bars represent standard deviation. ATS, anterior transarticular screw.
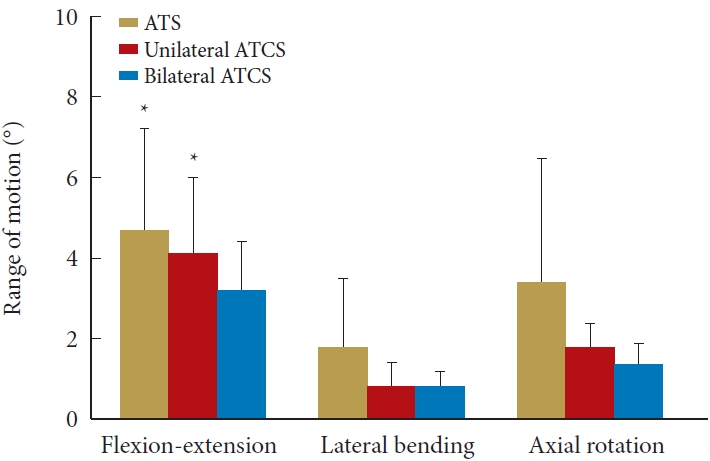
Fig. 6.
Bar graph demonstrating the neutral zone of C1–2 segment in all directions. *Indicates statistical difference from bilateral anterior transarticular crossing screw (ATCS) (p<0.05). Error bars represent standard deviation. ATS, anterior transarticular screw.

Table 1.
ROMs and NZs of C1–2 specimens in different statues (°)
| ROM & NZ | Intact | Injury | ATS | Unilateral ATCS | Bilateral ATCS | |
|---|---|---|---|---|---|---|
| ROM | ||||||
| Flexion-extension | 12.4 ± 6.7 | 26.2 ± 8.9 | 4.7 ± 2.5* | 4.1 ± 1.9* | 3.2 ± 1.2 | |
| Lateral bending | 3.3 ± 1.6 | 11.0 ± 3.3 | 1.8 ± 1.7 | 0.8 ± 0.6 | 0.8 ± 0.4 | |
| Axial rotation | 63.7 ± 28.8 | 78.3 ± 10.3 | 3.4 ± .3.1 | 1.8 ± 0.6 | 1.4 ± 0.5 | |
| NZ | ||||||
| Flexion-extension | 3.2 ± 3.6 | 6.2 ± 5.3 | 0.6 ± 0.5 | 0.4 ± 0.3 | 0.5 ± 0.3 | |
| Lateral bending | 0.8 ± 0.8 | 2.6 ± 1.1 | 0.3 ± 0.3 | 0.3 ± 0.5 | 0.3 ± 0.5 | |
| Axial rotation | 25.8 ± 12.5 | 30.8 ± 7.4 | 2.1 ± 4.1 | 0.6 ± 0.5* | 0.8 ± 0.6 | |
REFERENCES
1. Barbour JR. Screw fixation and fractures of the odontoid process. S Aust Clin 1971;5:20-4.
2. Lu J, Ebraheim NA, Yang H, et al. Anatomic considerations of anterior transarticular screw fixation for atlantoaxial instability. Spine (Phila Pa 1976) 1998;23:1229-35. discussion 1236.


3. Reindl R, Sen M, Aebi M. Anterior instrumentation for traumatic C1-C2 instability. Spine (Phila Pa 1976) 2003;28:E329-33.


4. Sen MK, Steffen T, Beckman L, et al. Atlantoaxial fusion using anterior transarticular screw fixation of C1-C2: technical innovation and biomechanical study. Eur Spine J 2005;14:512-8.




5. Sonone S, Dahapute AA, Waghchoure C, et al. Anatomic considerations of anterior transarticular screw fixation for atlantoaxial instability. Asian Spine J 2019;13:890-4.




6. Gembruch O, Ahmadipour Y, Lemonas E, et al. The anterior transarticular fixation of C1/C2 in the elderly with dens fractures. Int J Spine Surg 2020;14:162-9.



7. Josten C, Jarvers JS, Glasmacher S, et al. Anterior transarticular atlantoaxial screw fixation in combination with dens screw fixation for type II odontoid fractures with associated atlanto-odontoid osteoarthritis. Eur Spine J 2016;25:2210-7.



8. Polli FM, Miscusi M, Forcato S, et al. Atlantoaxial anterior transarticular screw fixation: a case series and reappraisal of the technique. Spine J 2015;15:185-93.


9. Lvov I, Grin A, Kaykov A, et al. Anterior transarticular C1-C2 fixation with contralateral screw insertion: a report of two cases and technical note. Eur Spine J 2018;27:347-52.



10. Wu AM, Wang XY, Zhou F, et al. Percutaneous atlantoaxial anterior transarticular screw fixation combined with miniopen posterior C1/2 wire fusion for patients with a high-riding vertebral artery. J Spinal Cord Med 2016;39:234-9.



11. Liu Q, Lin J, Yin Y, et al. Anterior transarticular crossing screw placement for atlantoaxial instability in children: computed tomography-based study. World Neurosurg 2022;161:e192-8.


12. Xu H, Chi YL, Wang XY, et al. Comparison of the anatomic risk for vertebral artery injury associated with percutaneous atlantoaxial anterior and posterior transarticular screws. Spine J 2012;12:656-62.


13. Koller H, Kammermeier V, Ulbricht D, et al. Anterior retropharyngeal fixation C1-2 for stabilization of atlantoaxial instabilities: study of feasibility, technical description and preliminary results. Eur Spine J 2006;15:1326-38.




14. Ji W, Zheng M, Tong J, et al. Feasibility and trajectory study of anterior transarticular crossing screw placement for atlantoaxial joint instability: a cadaveric study and description of a novel technique. Eur Spine J 2015;24:2954-60.



15. Liu Q, Ji W, Yang Z, et al. Radiologic characteristics of anterior transarticular crossing screw placement for atlantoaxial joint instability. World Neurosurg 2020;137:e152-8.


16. Goertzen DJ, Kawchuk GN. A novel application of velocitybased force control for use in robotic biomechanical testing. J Biomech 2009;42:366-9.


17. Finn MA, Apfelbaum RI. Atlantoaxial transarticular screw fixation. Neurosurgery 2010;66:A184-92.


18. Gallie WE. Skeletal traction in the treatment of fractures and dislocations of the cervical spine. Ann Surg 1937;106:770-6.



19. Kim SM, Lim TJ, Paterno J, et al. Biomechanical comparison of anterior and posterior stabilization methods in atlantoaxial instability. J Neurosurg 2004;100:277-83.


20. Lapsiwala SB, Anderson PA, Oza A, et al. Biomechanical comparison of four C1 to C2 rigid fixative techniques: anterior transarticular, posterior transarticular, C1 to C2 pedicle, and C1 to C2 intralaminar screws. Neurosurgery 2006;58:516-21. discussion 516-21.



21. Bianco RJ, Arnoux PJ, Wagnac E, et al. Minimizing pedicle screw pullout risks: a detailed biomechanical analysis of screw design and placement. Clin Spine Surg 2017;30:E226-32.































