- Search
|
|
||
Abstract
Background/Aims
The purpose of this study was to provide anatomical data on the dimensions and location of the subaxial transverse foramen (TF) in relation to surgical landmarks routinely used during anterior cervical procedures.
Methods
A total of 116 patients who underwent preoperative computed tomography (CT) evaluations for degenerative cervical disease were enrolled. Axial and coronal CT images of the cervical vertebrae from C3 to C6 were analyzed to measure interforaminal distance, the TF distance from the anterior and posterior vertebral body margin, TF dimensions, and the TF medial margin from the tip and medial margin of the uncus. Comparative and correlative analyses were also performed according to age, body mass index (BMI), and sex.
Results
All measurement values in male patients were larger than those in their female counterparts. The interforaminal distance gradually increased from C3 to C6. The distance of the TF medial margin from the tip of the uncus was found be above approximately 3 mm in all vertebrae except C6. Correlation analysis revealed that age had a significant negative relationship with the transverse diameter of TF. In contrast, BMI had a significant positive correlation with interforaminal distance. Moreover, the distances of the TF medial margin from the tip and medial margin of the uncus showed strong negative correlations with age.
Conclusion
Useful morphometric data were obtained that may help the operating surgeon to avoid vertebral artery injury. The safe distance from the tip of the uncus to the TF medial margin was found to be approximately 3 mm, and this distance should not be violated during lateral decompression. In addition, this value may decrease with age.
Vertebral artery (VA) injury during anterior cervical procedures is a rare catastrophic but yet an avoidable event often leading to intraoperative or postoperative complications. A thorough understanding of the VA and its relation to the bony structures of cervical vertebra is essential. Although morphometric analyses of the relationship of VA with the surrounding bony structures have been published in literatures [1-10], the scope of these publications is limited. Most of these reports were based on cadaveric studies in a small number of subjects [1-5,7]. However, Malik et al. [6] studied in live subjects but they were all young and without any symptoms or were nonsurgical subjects. Another important point to be noted in these representative studies was that they were all performed in non-Asian population and with regards to the possibility of differences in anatomy depending upon the ethnicity and geographic location, scope of such studies in Korean population might be questionable. However, Park et al. [8] studied anatomy in Korean population but the main drawback of their study is that all the subjects were nonsurgical with normal uncinates. Hence clinical implication of such normal findings in patients with degeneration or ailments that need to be addressed surgically becomes once again irrelevant. Thus the main objective of this study was to study the location and morphology of transverse foramen (TF) in relation to the vertebral bodies C3 through C6, using computed tomography (CT) analysis in elderly Korean patients planned for elective anterior cervical procedures and present an anatomical basis of reference for dealing such patients in future to avoid iatrogenic VA injury.
From January 2010 to December 2016, a total of 116 patients who underwent preoperative CT evaluation for the degenerative cervical disease were enrolled. We retrospectively reviewed these patients, patients meeting any of the following criteria were excluded: younger than 50 years; prior cervical spine surgery; history of an acute trauma or cervical fracture; evidence of congenital cervical malformations; infections; cervical bone tumor.
This study was approved by the Institutional Review Board of Kyung Hee Medical Center (approval number: KMC 1511-11). Written informed consent by the patients was waived by the IRB due to a retrospective nature of our study.
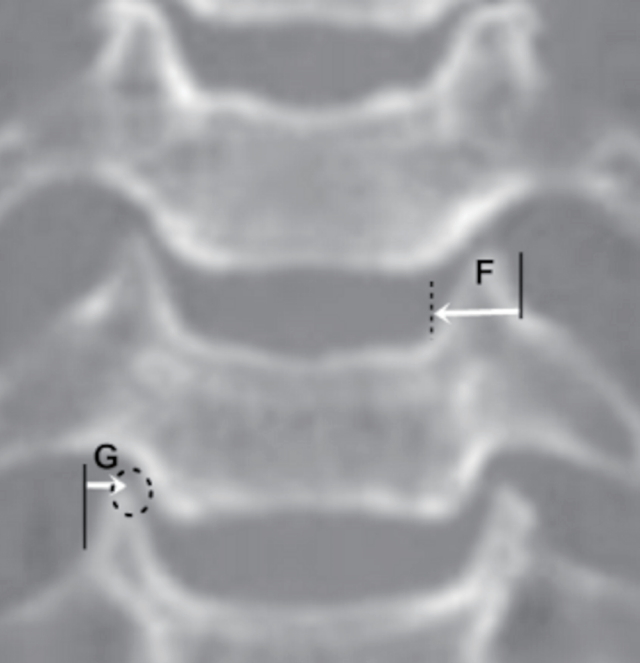
CT scans of the cervical spine were obtained in 3-mm increments (Siemens Somatom, Siemens Inc., Munich, Germany) with the subject supine, in a neutral position. Images reconstructed at 1.5-mm intervals were arranged into axial (parallel to vertebral body endplates) and coronal (perpendicular to the spinal axis) plane. In axial CT images of cervical vertebrae, the following dimensions were recorded: TF diameters, interforaminal distance, and an anterior and posterior border of TF to anterior and posterior vertebral body margin (Fig. 1). In coronal planes, distances from the medial margin of TF to the tip of the uncovertebral joint and medial margin of the uncus were measured (Fig. 2). During measurement of distances, a best-fit image of the vertebral body including the right or left TF was obtained. To increase intra-, interobserver reliability, all measurements were performed by 2 independent observers. Two observers were neurosurgeons, all correlation coefficients were above 0.6.
Descriptive statistics, such as mean, standard deviations were computed for all data. Correlations between patientsŌĆÖ demographic factors and transverse foraminal dimension (or landmark) were analyzed by calculating Pearson correlation coefficients. IBM SPSS Statistics ver. 21.0 (IBM Co., Armonk, NY, USA) was used, a p-value less than 0.05 was considered significant.
One hundred sixteen patients (57 men, 59 women) were enrolled in this study. Mean age and body mass index (BMI) was 67.4┬▒3.9 years and 25.1 kg/m2.
Mean anterior-posterior foraminal diameter was larger in males than in females at all spinal levels. For males and females, anterior-posterior diameters gradually increased from C3 through C6. It was larger in males than in females at each level from C3 through C6. Mean transverse diameter was dependent on the only gender. It was larger in males than in females at each spinal level from C3 through C6. The mean value was above 6.1 mm in males, was approximately 5.8 mm in females. Mean interforaminal distance was dependent on gender and spinal level. It was larger in males than in females at all spinal levels, generally increased from C3 through C6. All measured values are shown in Table 1.
In correlation analysis between transverse foraminal dimension and demographic factors, the effect of changes in age and BMI on diameter was assessed (Table 2). Interforaminal diameters exhibited a positive, significant correlation in each spinal level. In contrast, anterior-posterior foraminal diameters did not correlate with any variables. With the exception C6 segment, transverse foraminal diameters exhibited a negative, significant correlation from C3 through C5.
Anterior and posterior margin magnitude was dependent on sex. Mean anterior and posterior margin was larger in males than in females at each spinal level from C3 from through C6. Mean anterior margin was smallest at C4, mean posterior margin was smallest at C3 for both genders. Foramen-uncus tip distance was dependent on sex and spinal level. Mean distance was greater in males than in females at each spinal level from C3 through C6. Mean distance was smallest at C6 for both sexes, the value was less than 3 mm. Foramen-uncus medial margin distance was dependent on sex. Except for the female C5 level, all values were greater than 6 mm regardless of sex or spinal level. All measured values are shown in Table 3.
In correlation analysis between transverse foraminal landmark and demographic factors, the effect of changes in age and BMI on diameter was assessed (Table 4). The age was significant negative correlated with foramen-uncus tip and foramenuncus medial margin distance in each spinal level. In contrast, the BMI did not correlate with any variables (except for C4, foramen-tip distance).
VA injury during foraminal decompression via anterior approach in the absence of instrumentation is rare but very fatal. When surgeries involve complex procedures like corpectomy, instrumentation, and treatment for neoplasms and traumas, the incidence of intraoperative VA injury ranges from 0.14% to 9.8% depending on the experience of the surgeon and approach [11,12]. On the other hand, this incidence decreases dramatically to approximately 0.3% during low-risk cervical procedures [13]. Despite low incidence, the surgeon should be aware of the possibilities of such injuries and should understand and have a thorough knowledge of the VA anatomy and its relationship with the surrounding bony structures.
Several studies have been performed to define the relationship of VA and bony structures around it. But most of them were cadaveric studies and dealt with the morphometric analyses of the TF in relation to vertebral landmarks. The implication of those findings in a surgical scenario is debatable. Few years back, a retrospective study involving 98 asymptomatic young volunteers was published [6]. The authors analyzed interforaminal distance, TF distance from anterior and posterior vertebral body margins, TF dimensions and medial margin distance from the uncus tip and medial margin from C3 to C7 vertebra. Our current study is also based on or influenced by this study but we attempted to define these parameters in patients who were planned for surgeries as dimensions could be easily affected by the presence and degree of degeneration along with the pathology. Above studies were performed in non-Asian subjects and these findings could be different in Korean counterparts. We performed our study in a racially homogenous Korean society and in those patients who were planned for surgeries. And different from the aforementioned study, we also analyzed the effect of the patientŌĆÖs age and BMI on these findings.
Similar to the study performed by Vaccaro et al. [9] and Malik et al. [6], the interforaminal distance gradually increased C3 through C6. Similarly, although anteroposterior dimension of the foramen gradually increased; decrease in the transverse dimension of the foramen was noted from C3 to C6 level. This might imply that there are few millimeters of space available for lateral decompression when moving from cephalad to caudal direction. But this needs to be compared and verified with other prominent bony structures like uncinate process which is a more reliable structure to determine the laterality of decompression. When the medial margin of the TF was measured from the tip of the uncus and from the medial margin of the uncinate process, the foramen gradually shifted to the medial side from C3 to C6 except for C6 in terms of foramen to the medial margin of the uncinate process. And the foramen was also found to move anteriorly from cephalad to caudal. These trends in our study are in agreement with the findings suggested by Malik et al. [6] However, although dimensions in males were different from their female counterparts no statistical significance could be appreciated in our study.
Correlation analyses revealed that age had a significant negative effect on the transverse diameter of the TF which could be due to the increased incidence of bony degeneration including hypertrophy with the increase in age, mechanism very similar to decrease in width of the neural foramen with age [14]. Also with age, the distances from the TF medial margin to the medial margin and tip of the uncinate process were found to decrease in the entire vertebra. Hence in the patient with advanced age, the transverse diameter of the arterial foramen would be expected to be smaller and during lateral decompression safe distance from the VA is comparatively shorter than the younger counterparts. This implies that the treating surgeon should be more cautious of avoiding VA injury while operating in an elderly patient. We found that the safe distance from the tip of the uncinate process to the TF margin was approximately 3 mm and at least this safe distance should be maintained. Also, the medial margin of the uncinate process was approximately 6 mm distant from the medial margin of the TF in the entire vertebra. Previous studies also support that the width of the uncinate process varied from 3.5 to 6 mm [7,15-18]. BMI, on the other hand, was found to have a positive effect on interforaminal distance i.e., with the increase in BMI, there was the concurrent increase in the interforaminal distance. In other words, in patients with higher BMI values, one can expect more lateral location of TF. But these findings are obtained from Korean subjects and generalization to other races is debatable. Park et al. [8] performed a different anatomical study in Korean patients based on morphometric analyses of a height of uncinate process and distance of pedicle from midline to establish safe dimensions of an uncinate process that can be resected during anterior procedures. They derived that it is safe to decompress the intervertebral foramen by removing the uncinate process out to 1.3 cm laterally from the midline and approximately 4 mm above the pedicle. Therefore, after analyzing the findings from our and the study by Park et al. [8] we can derive to a conclusion that in Korean patients there is a safety margin of 3 to 4 mm laterally from the medial margin of the uncinate process to avoid TF.
In summary, our results suggest that there is approximately 6 mm of safe distance from the medial margin of the uncinate process to the medial margin of the TF whereas the safe distance from the tip of the uncus to the medial margin of the TF is only about 3 mm. However, with age, the transverse diameter of the TF is expected to get smaller leading to increased probability of injuring VA whereas, with the increase in BMI, the interforaminal distance also increases concurrently resulting the increase in lateral safety margin during decompression. Maintaining decompression more posterior and medial to the wall of the TF will definitely increase the safety margin, however, it is recommended that the surgeon examine the preoperative radiological images thoroughly before performing decompressions in each case.
Fig.┬Ā1.
Axial cervical vertebrae measurements. A, anterior to posterior diameter of the transverse foramen. B, transverse diameter of the transverse foramen. C, inter-foraminal distance. D, anterior margin. E, posterior margin.
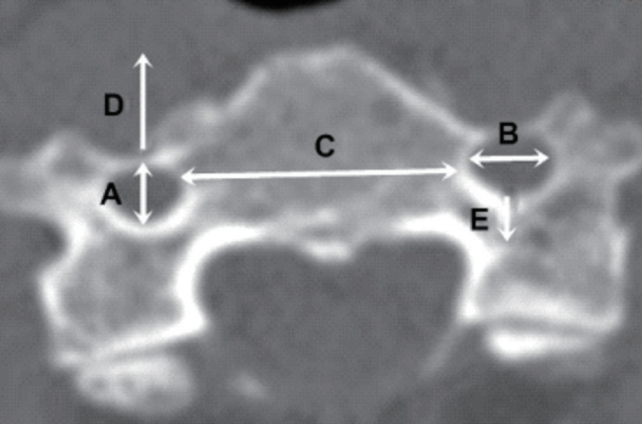
Fig.┬Ā2.
Coronal cervical vertebrae measurement. Distances from the medial margin of the transverse foramen to the medial ridge of the uncovertebral joint (F) and to tip of the uncus (G). During measurement of distances, a best fit image of the vertebral body including right or left transverse foramen was obtained. The medial margin of the transverse foramen (black straight line). The medial ridge of the uncovertebral joint (black dotted line). Tip of the uncus (black dotted circle).
Table┬Ā1.
Mean cervical spine transverse foraminal dimensions in axial cervical images (mm)
Table┬Ā2.
Correlations between patientŌĆÖs demographic factors and transverse foraminal dimension
| Variable |
C3 |
C4 |
C5 |
C6 |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AP | TR | IF | AP | TR | IF | AP | TR | IF | AP | TR | IF | |
| Age (r) | -0.24 | -0.37 | -0.12 | -0.25 | -0.38 | -0.12 | -0.27 | -0.43 | -0.17 | -0.28 | -0.20 | -0.27 |
| ŌĆāp-value | 0.14 | * | 0.44 | 0.11 | * | 0.45 | 0.09 | * | 0.29 | 0.08 | 0.21 | 0.08 |
| BMI (r) | 0.05 | 0.07 | 0.14 | 0.11 | 0.10 | 0.16 | 0.06 | 0.11 | 0.22 | 0.08 | 0.07 | 0.25 |
| ŌĆāp-value | 0.07 | * | * | 0.11 | 0.17 | * | 0.11 | 0.30 | * | 0.09 | * | * |
Table┬Ā3.
Subaxial course of the vertebral artery foramen (mm)
Table┬Ā4.
Correlations between patientŌĆÖs demographic factors and transverse foraminal landmark
| Variable |
C3 |
C4 |
C5 |
C6 |
||||
|---|---|---|---|---|---|---|---|---|
| Foramen-Tip | Foramen-Medial margin | Foramen-Tip | Foramen-Medial margin | Foramen-Tip | Foramen-Medial margin | Foramen-Tip | Foramen-Medial margin | |
| Age (r) | -0.57 | -0.63 | -0.59 | -0.62 | -0.32 | -0.57 | -0.27 | -0.45 |
| ŌĆāp-value | * | * | * | * | * | * | 0.85 | * |
| BMI (r) | 0.11 | 0.26 | 0.09 | 0.18 | 0.06 | 0.20 | 0.09 | 0.19 |
| ŌĆāp-value | 0.08 | 0.41 | * | 0.12 | 0.33 | 0.41 | 0.07 | 0.09 |
REFERENCES
1. Curylo LJ, Mason HC, Bohlman HH, et al. Tortuous course of the vertebral artery and anterior cervical decompression: a cadaveric and clinical case study. Spine (Phila Pa 1976) 2000 25:2860-4.


2. Ebraheim NA, Lu J, Brown JA, et al. Vulnerability of vertebral artery in anterolateral decompression for cervical spondylosis. Clin Orthop Relat Res 1996 322:146-51.

3. Ebraheim NA, Reader D, Xu R, et al. Location of the vertebral artery foramen on the anterior aspect of the lower cervical spine by computed tomography. J Spinal Disord 1997 10:304-7.


4. G├╝ven├¦er M, Men S, Naderi S, et al. The V2 segment of the vertebral artery in anterior and anterolateral cervical spinal surgery: a cadaver angiographic study. Clin Neurol Neurosurg 2006 108:440-5.


5. Heary RF, Albert TJ, Ludwig SC, et al. Surgical anatomy of the vertebral arteries. Spine (Phila Pa 1976) 1996 21:2074-80.


6. Malik SW, Stemper BD, Metkar U, et al. Location of the transverse foramen in the subaxial cervical spine in a young asymptomatic population. Spine (Phila Pa 1976) 2010 35:E514-9.


7. Oh SH, Perin NI, Cooper PR. Quantitative three-dimensional anatomy of the subaxial cervical spine: implication for anterior spinal surgery. Neurosurgery 1996 38:1139-44.


8. Park MS, Moon SH, Kim TH, et al. Surgical anatomy of the uncinate process and transverse foramen determined by computed tomography. Global Spine J 2015 5:383-90.



9. Vaccaro AR, Ring D, Scuderi G, et al. Vertebral artery location in relation to the vertebral body as determined by twodimensional computed tomography evaluation. Spine (Phila Pa 1976) 1994 19:2637-41.


10. Jin SW, Kim SH, Choi JI, et al. Late infection from anterior cervical discectomy and fusion after twenty years. Korean J Spine 2014 11:22-4.



11. Neo M, Fujibayashi S, Miyata M, et al. Vertebral artery injury during cervical spine surgery: a survey of more than 5600 operations. Spine (Phila Pa 1976) 2008 33:779-85.


12. Yeom JS, Buchowski JM, Kim HJ, et al. Risk of vertebral artery injury: comparison between C1-C2 transarticular and C2 pedicle screws. Spine J 2013 13:775-85.


13. Oberm├╝ller T, Wostrack M, Shiban E, et al. Vertebral artery injury during foraminal decompression in "low-risk" cervical spine surgery: incidence and management. Acta Neurochir (Wien) 2015 157:1941-5.


14. Humphreys SC, Hodges SD, Patwardhan A, et al. The natural history of the cervical foramen in symptomatic and asymptomatic individuals aged 20-60 years as measured by magnetic resonance imaging. A descriptive approach. Spine (Phila Pa 1976) 1998 23:2180-4.


15. Brigham CD, Tsahakis PJ. Anterior cervical foraminotomy and fusion. Surgical technique and results. Spine (Phila Pa 1976) 1995 20:766-70.


16. Lu J, Ebraheim NA, Yang H, et al. Cervical uncinate process: an anatomic study for anterior decompression of the cervical spine. Surg Radiol Anat 1998 20:249-52.

































