- Search
|
|
||
Abstract
Objective
To investigate the utility of full-endoscopic lumbar discectomy (FELD) in surgical treatment of recurrent lumbar disc herniation (RLDH).
Methods
Forty-five patients were prospectively studied. All patients were subjected to FELD for RLDH. They were assessed preoperatively and in regular intervals at 6 weeks and 3 months, 6 months, and 12 months postoperatively. Evaluation was conducted with visual analogue scale for leg (VAS-LP) and low back (VAS-BP) pain. Short-Form 36 Health Survey Questionnaire was utilized for health-related quality of life assessment.
Results
All studied parameters featured statistically significant amelioration at all follow-up intervals. Maximal improvement was in general at 6 weeks observed, with subsequent lesser improvement until 6 months and stabilization until the end of follow-up. Comparative assessment indicated that VAS-BP displayed quantitatively lower improvement, whereas physical function, bodily pain, and role-emotional parameters demonstrated greater amelioration.
Lumbar disc herniation (LDH) represents a frequent situation in routine clinical practice [1]. Primary clinical manifestations include motor and/or sensory deficit in distribution of the affected nerve root, encountered on the ground of referred low back and/or radicular pain. Conservative treatment should institute the first-line selection. Medication regimen, physical therapy sessions, epidural spinal injections as well as other alternative treatment methods may be hence initially implemented. However, clinical failure of conservative management dictates surgical intervention. Microdiscectomy procedures continue to represent the gold standard surgical treatment method in these cases [2].
Nevertheless, microdiscectomy surgery conduction may be accompanied by considerable complications. Direct nerve root injury, hematoma, instability as well as wound complications may occur [3,4]. Recurrent LDH (RLDH) represents another special and potentially serious complication. Prevalence of RLDH is reported to be 5%ŌĆō18%, depending from the follow-up period accomplished. The emergence of clinically significant and undertreated with conservative methods pain in conjunction with motor deficiency imposes surgical treatment. Revision discectomy may be then conducted. However, surgical outcomes are poorer than these of primary intervention [5].
Recently, full-endoscopic lumbar discectomy (FELD) has been proposed as a potentially beneficial alternative for RLDH surgical management [6]. FELD is performed selecting transforaminal (TFED) or interlaminar (IFED) route [7]. FELD represents a novel, emerging and minimally invasive technique in the field of spine surgery. Remarkable surgical advantages as preservation of dorsal musculature and spine elements as well as minimization of perioperative morbidity are responsible for its exponential expansion in current years [8-10].
To our best knowledge, recruitment of FELD for RLDH after conventional open discectomy/ microdiscectomy has been described few times in the literature [11-16]. However, in none of these studies was patientsŌĆÖ health-related quality of life (HRQoL) assessed, so that a more multifaceted evaluation of FELD for RLDH could be accomplished.
Aim of this article is to analyze the outcomes of FELD for RLDH, paying particular focus in HRQoL evaluation.
All patients recruited in this study were diagnosed with RLDH after conventional microdiscectomy, according to clinical and radiologic criteria. Moreover, current indications for iterative conventional microdiscectomy were fulfilled. StudyŌĆÖs principles and aims were thoroughly explicated in all patients. All patients agreed to participate, signing a fully informed written acquiescence. This study was further approved by Institutional Review Board and local ethics committee. Additionally, all perspectives in this study were in complete compliance with Ethical Principles for Medical Research Involving Human Subjects, as defined in Helsinki Declaration of 1975 and as revised in 2000.
Inclusion criteria were: (1) radiculopathy, (2) positive nerve root tension sign, (3) negative prone instability test, (4) motor neurologic deficit on clinical examination, (5) hernia confirmed by magnetic resonance imaging of the lumbar spine, in compliance with clinical findings, (6) emergence of resistant to 12-week conservative treatment (medication regimen, physical therapy sessions and epidural spinal injections) pain.
(1), (4), (5), and (6) were in all patients after a minimum of 6 months (mean, 10 months) after previous surgery, at the same intervertebral level and on the ipsi- or contralateral side of the pathology encountered.
Exclusion criteria were: (1) ascending LDH (migrated disc fragments with ascending course), (2) LDH located at the shoulder of nerve root, (3) central or lateral recess spinal stenosis, (4) positive prone instability test, (5) spondylolisthesis, (6) spinal tumor or infection, and (7) vertebral fracture.
Forty-five patients were enrolled in this prospectively designed original study. All patients were subjected in successful TFED with transforaminal endoscopic surgical system (TESSYS) for RLDH in 2016ŌĆō2017. Clinical evaluation was performed preoperatively and at predetermined specific chronic intervals in 6 weeks and in 3 months, 6 months, and 12 months postoperatively. Practical assessment was conducted with the standardized visual analogue scale (VAS). VAS was implemented 2 times for each patient in each follow-up interval; lower limb pain (VAS for leg pain, VAS-LP) and low back pain (VAS for back pain, VAS-BP) were thus separately considered. Furthermore, general evaluation of HRQoL was by the Short-Form 36 (SF-36) Health Survey Questionnaire evaluated.
All patients were subjected to TFED with TESSYS by a single experienced spine surgeon and in a single institute. Technique was performed under local anesthesia and mild sedation. All patients received antibiotic prophylaxis (1.5-g Cefuroxim Sodium) preoperatively. Intraoperative monitoring (blood pressure, pulse rate, electrocardiographic record, and oxygen saturation) was incessantly conducted. Patients were initially in lateral decubitus position placed, lying down on the opposite side. Optimal enlargement of the foraminal space could be hence accomplished. Entry point was determined at 11 cm laterally of midline, so that transit corridor led in Kambin triangle [17]. Disinfection of surgical field and local anesthesia administration at the point of needle entrance was subsequently applied. Needle was promoted under constant fluoroscopic guidance. Administration of mild sedation and analgesia (fentanyl ampule) was afterwards applied. Sequentially forwarded reamers were characterized by gradually increasing diameters (5.5, 6.5, and 7.5 mm; Joimax Inc., Irvine, CA, USA), so that compensatory foraminoplasty could be accomplished. Cannula and endoscope were finally imported, followed by removal of herniated disc material with graspers (Fig. 1).
VAS is theorized to constitute a facile and precise method for evaluation of pain intensity [18]. A unipolar horizontal line (100 mm) was implemented in present study. Patients were asked to demonstrate the perceived pain level with a point in every predetermined follow-up interval. VAS was 2 times in each clinical assessment applied; lower limb and low back pain (recorded as VAS-LP and VAS-BP respectively) were thus separately esteemed. All scores were registered as millimeters (mm), being previously processed with a one-decimal place approach. Minimal clinically remarkable alteration was defined at 9 mm. No other relevant parameters as age, pain etiology and gender were separately investigated [19].
SF-36 Medical Health Survey Questionnaire represents an established method for HRQoL assessment in the field of spine surgery.20 This versatile questionnaire is composed of 36 individual items, being represented in 8 distinct aspects of patientsŌĆÖ overall health status; physical function (PF), role-physical (RP), bodily pain (BP), general health (GH), energy, fatigue and vitality (V), social function (SF), role-emotional (RE) and mental health (MH). This questionnaire was completed by all patients in each follow-up interval. Results of each patient were thereafter compiled and processed, being represented by a percentage. The accomplishment of higher scores in these 8 parameters is linked to ameliorated HRQoL. Questionnaires were theorized invalid if less than 50% of form entries were filled out.
Statistical analysis of compiled data was by IBM SPSS Statistics ver. 23.0 (IBM Co., Armonk, NY, USA) conducted. Continuous variables (age, VAS scores, and SF-36 scores) were featured as mean┬▒standard deviation. Categorical variables were presented as percentages. Statistical comparison of continuous parameters was conducted either with Student t-test for independent samples or with Wilcoxon test (in the presence and absence of normal distribution, respectively). Level of statistical significance was established at p=0.05.
All patients were discharged at the first postoperative day. No severe complications (as dural tear, infection, major intraoperative hemorrhage, or nerve tissue damage) were observed. One patient (2.22%) expressed postoperative dysesthesia in distribution of exiting nerve root (L5 root). This complication was, however, provisional, being retreated with conservative treatment in the first follow-up section (6 weeks postoperatively).
Patients were subsequently evaluated until the end of followup in 12 months postoperatively. Demographic and other characteristics of enrolled patients are featured in Table 1.
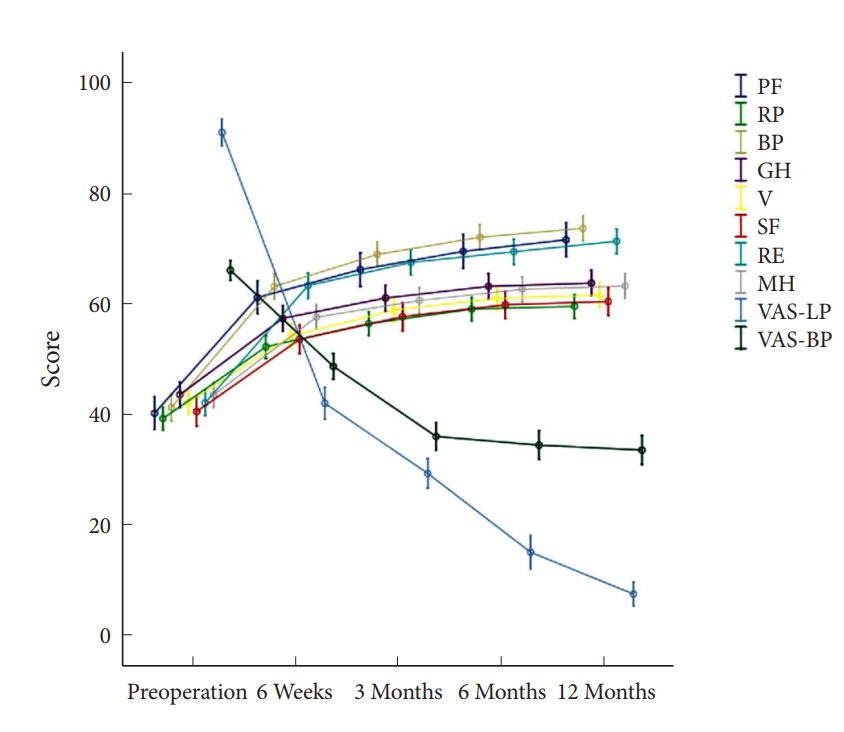
Studied indexes were recorded to feature maximal amelioration in 6 weeks postoperatively. Lesser improvement was in 3 and 6 months presented, with subsequent stabilization and minimal only amelioration until 12 months. This improvement pattern was similar for all studied parameters except for VAS-BP, which displayed equal alteration in 6 weeks and 3 months intervals, with subsequent stabilization (Fig. 2).
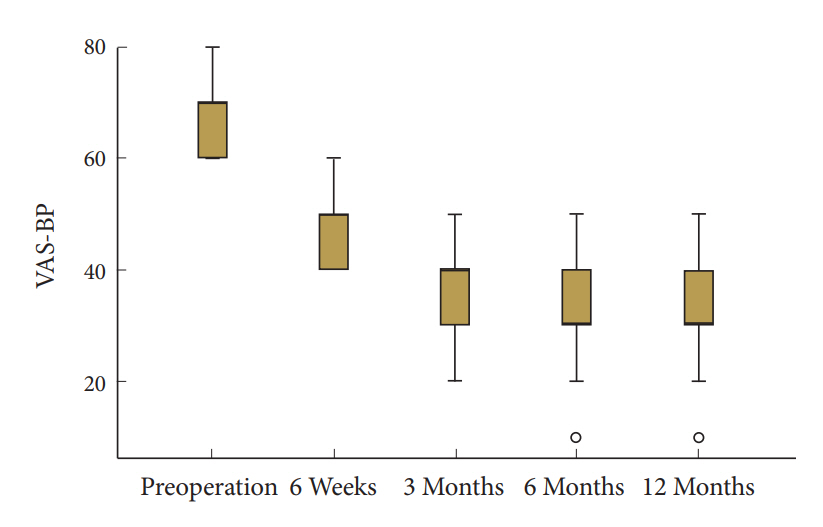
Evaluation of VAS scores indicated thus a considerable differentiation. Preoperative values of VAS-LP and VAS-BP were remarkably differentiated. VAS-LP scores presented a major and statistically significant improvement in 6 weeks postoperatively, accomplishing lesser improvement in 3 months, with ulterior stabilization and minimal alteration until the end of follow-up (Fig. 3). Despite the relatively lesser quantitative amelioration after the interval of 6 weeks, statistical analysis demonstrated a statistically significant improvement in every followup assessment, when compared with previous interval (Table 2). VAS-BP values also featured a statistically significant amelioration in all follow-up intervals. Nevertheless, quantitative improvement was remarkably slighter in this parameter (Fig. 4, Table 2).
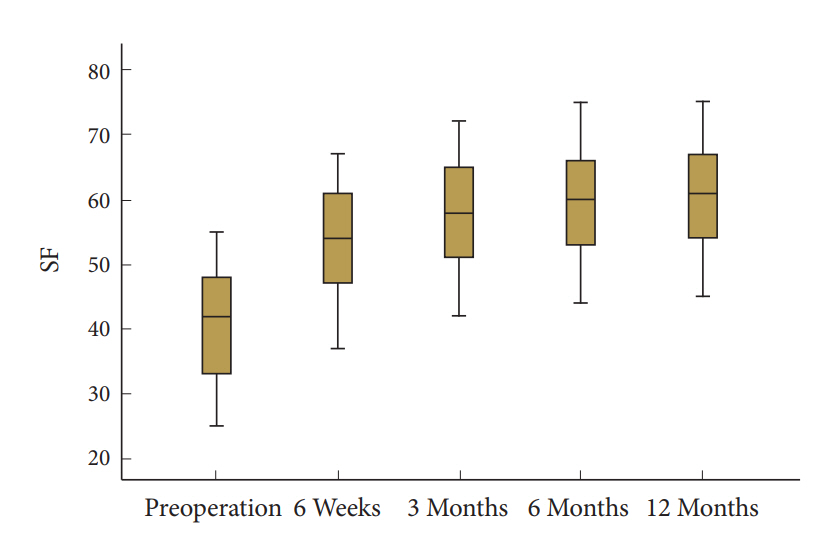
All studied indexes of SF-36 featured also a strong statistically significant improvement at 6 weeks postoperatively, whereas presence of minor amelioration in 3 and 6 months with subsequent consolidation in 12 months was observed. Statistical significance was maintained in all follow-up intervals for all studied indexes, being clearly strong (Table 3). PF, BP, and RE were recorded to demonstrate major amelioration (Fig. 5, Table 3). The other assessed parameters featured lesser and equal improvement rates (Fig. 6, Table 3).
The precise definition of RLDH remains controversial in the literature. Nonetheless, RLDH is primarily determined as the emergence of disc reherniation in the ipsilateral or contralateral side and at the same intervertebral level of previously operated lesion. The clinical appearance of radiculopathy after at least 6 months free of symptomatology is substantial for RLDH diagnosis [5].
Anticipation of RLDH appearance seems to be particularly complex. Li et al. [21] retrospectively evaluated 321 patients, in order to designate the risk factors for RLDH in China. It was concluded that male sex, young age, greater body mass index, harmful habits as smoking and occupational lifting, surgical procedures as well as especial anatomic-biomechanical characteristics of recurrent lesion are remarkably associated with RLDH. It was stated, thus, that presence of these risk factors imposes a closer postoperative monitoring.
FELD represents a novel surgical technique, principally recruited for the treatment of LDH. Endoscopic approach offers direct visualization and restoration of underlying lesion, alongside with minimization of intraoperative hemorrhage and epidural space scarring. Furthermore, FELD has been considerably correlated to diminished hospitalization times and more rapid rehabilitation. The utilization of local anesthesia with mild sedation eliminates the potentiality of hazardous general anesthesia-related complications emergence [8-10,22-24].
Revision surgery for RLDH constitutes a challenge for the spine surgeon. The initial conventional open discectomy/microdiscectomy results in epidural scarring, primarily encountered around dura mater and nerve roots [25-29]. Hence, conduction of a revision open discectomy/microdiscectomy may be unfavorably associated with dural tear and nerve root damage [29,30]. Selection of FELD as revision surgery overcomes this difficulty since cannula and endoscope are not promoted through the scar tissue in epidural space [29]. Furthermore, the emergence of CSF fistulas and dural tears is unlikely after revision FELD. However, FELD conduction may be linked to postoperative chronic low back pain [15].
Utilization of minimally invasive FELD for RLDH post conventional open discectomy/microdiscectomy has been reported few times in recent literature, individually or in the frame of general analysis [11-16]. A synopsis of these studies is quoted in Table 4. FELD outcomes were generally depicted to be favorable in all studies.
Shin et al. [11] retrospectively studied 41 patients with RLDH after previous open discectomy. FELD was applied in all patients. VAS scores for lower limb and low back pain featured a statistically significant amelioration postoperatively. Furthermore, implementation of modified MacNab criteria demonstrated that 90.2% of patients displayed favorable (excellent or good) outcomes. Rerecurrence was observed in 2 of patients (4.9%). Based on this data, authors concluded that FELD may constitute a beneficial alternative over repeated conventional discectomy, concerning its minimally invasive philosophy. This conclusion was also extracted in the study of Kim et al. [12], who aimed to investigate the technical adjustment of IFED in RLDH in 10 patients. The record of 1 rerecurrence (10%) and excellent or good outcomes by MacNab criteria in 6 patients (60%) advocated for the genuine benefit of IFED.
In another study, Kim et al. [13] retrospectively assessed 26 patients subjected either in TFED or in IFED. Underlying lesion was successfully removed in all cases, without the necessity of conversion to open surgery. An auspicious outcome according to MacNab criteria evaluation was accomplished in 21 patients (81%), whereas rerecurrence was exhibited to occur in 2 cases (7.7%). It was concluded that FELD should be considered as a beneficial alternative when revision surgery is required.
In the widest study, Liu and Zhou [15] attempted to compare FELD (conducting TFED) with minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF) for RLDH surgical management. Recovery rate was estimated to be 92.3% in FELD and 97.4% in MIS-TLIF group. Second recurrence was observed in 12 patients (5.7%) in FELD group. FELD was advocated to be equal to MIS-TLIF in terms of clinical outcomes favorability.
More recently, Wu et al. [16] retrospectively investigated the utility of full-endoscopic decompression (FED) in 94 consecutive patients with recurrent sciatica symptomatology. Seventy-four patients (78.8%) demonstrated favorable outcomes at MacNab criteria implementation. Rerecurrence rate was 9.6% on average, being not remarkably differentiated between the groups. FED was thus inferred to be safe and efficacious for surgical treatment of recurrent sciatica symptomatology.
Results of our study are in absolute conformity with existing literature data. Forty-five patients were prospectively assessed with VAS as well as with SF-36 questionnaire. SF-36 implementation, although bizarre, underlines the originality of our study. Hence, we selected not to be confined in VAS scores or MacNab criteria utilization. We theorize that RLDH is associated with reappearance of clinically noteworthy pain which has a considerable impact in many aspects of patientsŌĆÖ daily life by undermining physical, but also psychological status. Therefore, we decided to conduct a more multifaceted evaluation, in order to estimate the immiscible effect of FELD in patientsŌĆÖ postoperative daily routine.
All studied indexes featured a statistically significant amelioration in all follow-up intervals. FELD was thus evidenced to constitute a generally beneficial technique for RLDH. Regarding VAS scores, comparative evaluation of VAS-LP with VASBP indicated that VAS-LP featured a quantitatively major improvement. Efficacious foraminal decompression alongside with anatomical restoration of affected nerve root is potentially responsible for this outcome. The existence, however, of a previous open lumbar disc surgery particularly limits the possibility of significant VAS-BP reduction. Nevertheless, VAS-BP also was observed to be statistically significantly enhanced, reflecting thus the favorable impact of FELD.
Regarding SF-36, clinical assessment revealed a rapid and notable amelioration of HRQoL postoperatively. The emergence of RLDH is associated with a considerably negative impact in patientsŌĆÖ psychosocial status and daily routine. Hence, direct postoperative clinical amelioration upgraded these parameters. Furthermore, quick rehabilitation and return to work in conjunction with amelioration of intellectual abilities also contributed to quality of life improvement in enrolled patients.
Statistical comparison of individual SF-36 parameters denoted quantitatively greater improvement rates for PF, BP, and RE indexes. Consideration of these outcomes indicates that VASLP represents the primary portion of perceived pain. Improvement of VAS-LP, therefore, leads to diminish of BP parameter. This has 2 fundamental consequences. First, the semantic decline of pain upgrades patientsŌĆÖ psychological status, resulting in RE parameter improvement. Second, pain reduction results to physical functioning improvement. Hence, postoperative physical status improvement allows the conduction of a more intense physiotherapy protocol, leading thus in significant amelioration of PF at the end of follow-up in 1 year.
Regarding exclusion criteria of our study, FELD is not indicated in cases of spinal tumors or vertebral fractures. In addition, FELD cannot provide access to ascending or nerve root shoulder-located LDH. Hence, these patients have been excluded from our study. Furthermore, the presence of central or lateral recess spinal stenosis requires IFED and not TFED, which was conducted in present study. Patients with positive prone instability test or spondylolisthesis primarily require spinal fusion. Finally, FELD may be implemented in patients with spinal infections; however, description of this condition is not a part of present study.
Limitations of our study principally include the limited followup examination as well as the relatively small number of enrolled patients. However, regarding previous conducted prospective studies, only Liu and Zhou [15] utilized greater than our population size. Furthermore, agreement of our outcomes to existing literature data may confirm their validity. We, nonetheless, theorize that wider multicenter studies with more extensive follow-up (in order to assure the success of FELD more safely by excluding any potential rerecurrences occurring after 12 months postoperatively), greater number of patients as well as concurrent analysis with comparator groups are required in order to elucidate the precise utility of FELD in RLDH surgical treatment.
In this prospectively designed study, FELD was illustrated to be correlated with early return to daily activity as well as maintenance of favorable clinical outcomes for patients with RLDH. All studied indexes were statistically significantly ameliorated at the end of follow-up in 1 year. FELD may be therefore considered as a beneficial alternative instead of the majorly difficult revision open disc surgery for RLDH restoration.
CONFLICT OF INTEREST
Dr. Kapetanakis is a reference doctor for Joimax GmbH and receives payments for teaching. The other authors have no conflicts of interest to declare.
Fig.┬Ā1.
(A) Insertion of cannula and endoscope inside the annulus fibrosus for the removal of herniated disc material (lateral view). (B) Insertion of cannula and endoscope along the medial pedicular line for the removal of herniated disc material (anteroposterior view).

Fig.┬Ā2.
Schematic representation all studied indexes alteration during follow-up. PF, physical function; RP, role-physical; BP,
bodily pain; GH, general health; V, energy, fatigue and vitality; SF, social function; RE, role-emotional; MH, mental health; VAS-LP, visual analogue scale for leg pain, VAS-BP, visual analogue scale for back pain.
Table┬Ā1.
Demographic characteristics of recruited patients
Table┬Ā2.
VAS values differentiation during follow-up examination
| Parameter |
Clinical follow-up interval (p-value)a) |
||||
|---|---|---|---|---|---|
| Preoperative | 6 Weeks | 3 Months | 6 Months | 12 Months | |
| VAS-LP (mm) | 90.9 ┬▒ 7.9 | 42.0 ┬▒ 9.7 (< 0.001*) | 29.3 ┬▒ 8.9 (< 0.001*) | 15.1 ┬▒ 9.9 (< 0.001*) | 7.6 ┬▒ 7.1 (< 0.001*) |
| VAS-BP (mm) | 66.0 ┬▒ 5.8 | 48.7 ┬▒ 7.6 (< 0.001*) | 36.0 ┬▒ 8.4 (< 0.001*) | 34.4 ┬▒ 8.7 (< 0.001*) | 33.6 ┬▒ 8.6 (< 0.001*) |
Table┬Ā3.
Representation of improvement course of all SF-36 studied parameters
| Index |
Clinical follow-up interval (p-value)a) |
||||
|---|---|---|---|---|---|
| Preoperative | 6 Weeks | 3 Months | 6 Months | 12 Months | |
| PF | 40.2 ┬▒ 9.8 | 61.1 ┬▒ 9.9 (< 0.001*) | 66.1 ┬▒ 10.2 (< 0.001*) | 69.4 ┬▒ 10.3 (< 0.001*) | 71.5 ┬▒ 10.2 (< 0.001*) |
| RP | 39.2 ┬▒ 6.9 | 52.2 ┬▒ 6.9 (< 0.001*) | 56.4 ┬▒ 7.0 (< 0.001*) | 59.0 ┬▒ 7.0 (< 0.001*) | 59.5 ┬▒ 7.1 (< 0.001*) |
| BP | 41.2 ┬▒ 7.9 | 63.1 ┬▒ 7.6 (< 0.001*) | 68.9 ┬▒ 7.4 (< 0.001*) | 72.0 ┬▒ 7.5 (< 0.001*) | 73.6 ┬▒ 7.4 (< 0.001*) |
| GH | 43.6 ┬▒ 7.4 | 57.3 ┬▒ 7.6 (< 0.001*) | 61.0 ┬▒ 7.7 (< 0.001*) | 63.1 ┬▒ 7.6 (< 0.001*) | 63.7 ┬▒ 7.6 (< 0.001*) |
| V | 42.1 ┬▒ 7.2 | 54.1 ┬▒ 7.3 (< 0.001*) | 58.8 ┬▒ 7.2 (< 0.001*) | 60.9 ┬▒ 7.3 (< 0.001*) | 61.5 ┬▒ 7.4 (< 0.001*) |
| SF | 40.5 ┬▒ 8.7 | 53.6 ┬▒ 8.5 (< 0.001*) | 57.6 ┬▒ 8.3 (< 0.001*) | 59.8 ┬▒ 8.3 (< 0.001*) | 60.4 ┬▒ 8.2 (< 0.001*) |
| RE | 42.1 ┬▒ 7.7 | 63.2 ┬▒ 7.6 (< 0.001*) | 67.4 ┬▒ 7.5 (< 0.001*) | 69.4 ┬▒ 7.6 (< 0.001*) | 71.2 ┬▒ 7.4 (< 0.001*) |
| MH | 43.5 ┬▒ 7.5 | 57.6 ┬▒ 7.4 (< 0.001*) | 60.6 ┬▒ 7.7 (< 0.001*) | 62.6 ┬▒ 7.5 (< 0.001*) | 63.2 ┬▒ 7.6 (< 0.001*) |
Values are presented as mean┬▒standard deviation.
SF-36, Short-Form 36 Health Survey Questionnaire; PF, physical function; RP, role-physical; BP, bodily pain; GH, general health; V, energy, fatigue and vitality; SF, social function; RE, role-emotional; MH, mental health.
Table┬Ā4.
Description of FELD for RLDH surgical treatment in recent literature
| Study | Year | Study design | Patients (n) | Follow-up duration (mo) | Previous surgical operation (n) | Present surgical operation (n) |
|---|---|---|---|---|---|---|
| Shin et al. [11] | 2011 | Retrospective | 41 | 13ŌĆō42 (mean, 16) | Open discectomy | TFED (9), IFED (32) |
| Kim et al. [12] | 2012 | Technical report | 10 | 14.4 ┬▒ 9.9 | Open discectomy | IFED |
| Kim et al. [13] | 2014 | Retrospective | 26 | 19.3 ┬▒ 11.3 | Open discectomy (22), TFED (2), IFED (2) | TFED (11), IFED (15) |
| Yeung and Gore [14] | 2014 | Prospective | 30 | (mean, 40; minimum, 12) | Open or microsurgery | TFED |
| Liu and Zhou [15] | 2017 | Prospective | 401 | 12ŌĆō69 (mean, 46.5) | Open discectomy | 209 (TFED), 192 (MIS-TLIF) |
| Wu et al. [16] | 2018 | Retrospective | 94 | 36 (mean) | Open discectomy (30), FELD (17), TLIF (16), MED (31) | Posterolateral endoscopic decompression |
| Present study | Prospective | 45 | 12 | Microdiscectomy | TFED |
REFERENCES
1. Zhong M, Liu JT, Jiang H, et al. Incidence of spontaneous resorption of lumbar disc herniation: a meta-analysis. Pain Physician 2017 20:E45-52.

2. Benzakour T, Igoumenou V, Mavrogenis AF, et al. Current concepts for lumbar disc herniation. Int Orthop 2018 Nov 30 [Epub]. https://doi.org/10.1007/s00264-018-4247-6.


3. Shriver MF, Xie JJ, Tye EY, et al. Lumbar microdiscectomy complication rates: a systematic review and meta-analysis. Neurosurg Focus 2015 39:E6.

4. Zhang B, Liu S, Liu J, et al. Transforaminal endoscopic discectomy versus conventional microdiscectomy for lumbar discherniation: a systematic review and meta-analysis. J Orthop Surg Res 2018 13:169.




5. Mashhadinezhad H, Sarabi E, Mashhadinezhad S, et al. Clinical outcomes after microdiscectomy for recurrent lumbar disk herniation: a single-center study. Arch Bone Jt Surg 2018 6:397-401.


6. Mizuno J, Hirano Y, Nishimura Y. Establishment of endoscopic spinal neurosurgery and its current status. No Shinkei Geka 2016 44:203-9.

7. Wang D, Xie W, Cao W, et al. A cost-utility analysis of percutaneous endoscopic lumbar discectomy for L5-S1 lumbar disc herniation: transforaminal vs interlaminar. Spine (Phila Pa 1976) 2018 Oct 11 [Epub]. https://doi.org/10.1097/BRS.0000000000002901.

8. Kapetanakis S, Charitoudis G, Thomaidis T, et al. Health-related quality of life after transforaminal percutaneous endoscopic discectomy: an analysis according to the level of operation. J Craniovertebr Junction Spine 2017 8:44-9.



9. Kapetanakis S, Gkantsinikoudis N, Chaniotakis C, et al. Percutaneous transforaminal endoscopic discectomy for the treatment of lumbar disc herniation in obese patients: healthrelated quality of life assessment in a 2-year follow-up. World Neurosurg 2018 113:e638-49.


10. Kapetanakis S, Gkantsinikoudis N, Papathanasiou JV, et al. Percutaneous endoscopic ventral facetectomy: an innovative substitute of open decompression surgery for lateral recess stenosis surgical treatment? J Craniovertebr Junction Spine 2018 9:188-95.



11. Shin KH, Chang HG, Rhee NK, et al. Revisional percutaneous full endoscopic disc surgery for recurrent herniation of previous open lumbar discectomy. Asian Spine J 2011 5:1-9.



12. Kim CH, Chung CK, Jahng TA, et al. Surgical outcome of percutaneous endoscopic interlaminar lumbar diskectomy for recurrent disk herniation after open diskectomy. J Spinal Disord Tech 2012 25:E125-33.


13. Kim CH, Chung CK, Sohn S, et al. The surgical outcome and the surgical strategy of percutaneous endoscopic discectomy for recurrent disk herniation. J Spinal Disord Tech 2014 27:415-22.


14. Yeung A, Gore S. Endoscopic foraminal decompression for failed back surgery syndrome under local anesthesia. Int J Spine Surg 2014 Dec 1;8. https://doi.org/10.14444/1022. eCollection 2014.

15. Liu C, Zhou Y. Percutaneous endoscopic lumbar diskectomy and minimally invasive transforaminal lumbar interbody fusion for recurrent lumbar disk herniation. World Neurosurg 2017 98:14-20.


16. Wu J, Zhang C, Lu K, et al. Percutaneous endoscopic lumbar reoperation for recurrent sciatica symptoms: a retrospective analysis of outcomes and prognostic factors in 94 patients. World Neurosurg 2018 109:e761-9.


17. Kambin P, Brager MD. Percutaneous posterolateral discectomy. Anatomy and mechanism. Clin Orthop Relat Res 2087 (223):145-54.
18. Lee JJ, Lee MK, Kim JE, et al. Pain relief scale is more highly correlated with numerical rating scale than with visual analogue scale in chronic pain patients. Pain Physician 2015 18:E195-200.

19. Kelly AM. Does the clinically significant difference in visual analog scale pain scores vary with gender, age, or cause of pain? Acad Emerg Med 1998 5:1086-90.


20. Guilfoyle MR, Seeley H, Laing RJ. The Short Form 36 health survey in spine disease--validation against condition-specific measures. Br J Neurosurg 2009 23:401-5.


21. Li Z, Yang H, Liu M, et al. Clinical characteristics and risk factors of recurrent lumbar disk herniation: a retrospective analysis of three hundred twenty-one cases. Spine (Phila Pa 1976) 2018 43:1463-9.


22. Kapetanakis S, Giovannopoulou E, Thomaidis T, et al. Transforaminal percutaneous endoscopic discectomy in parkinson disease: preliminary results and short review of the literature. Korean J Spine 2016 13:144-50.



23. Kapetanakis S, Gkasdaris G, Angoules AG, et al. Transforaminal percutaneous endoscopic discectomy using transforaminal endoscopic spine system technique: Pitfalls that a beginner should avoid. World J Orthop 2017 8:874-80.



24. Kapetanakis S, Giovannopoulou E, Charitoudis G, et al. Health-related quality of life (HRQoL) following transforaminal percutaneous endoscopic discectomy (TPED) for lumbar disc herniation: a prospective cohort study - early results. J Back Musculoskelet Rehabil 2017 30:1311-7.



25. Ebeling U, Kalbarcyk H, Reulen HJ. Microsurgical reoperation following lumbar disc surgery. Timing, surgical findings, and outcome in 92 patients. J Neurosurg 1989 70:397-404.


26. J├Čnsson B, Str├Čmqvist B. Clinical characteristics of recurrent sciatica after lumbar discectomy. Spine (Phila Pa 1976) 1996 21:500-5.


27. Dai LY, Zhou Q, Yao WF, et al. Recurrent lumbar disc herniation after discectomy: outcome of repeat discectomy. Surg Neurol 2005 64:226-31.



28. Fu TS, Lai PL, Tsai TT, et al. Long-term results of disc excision for recurrent lumbar disc herniation with or without posterolateral fusion. Spine (Phila Pa 1976) 2005 30:2830-4.