- Search
|
|
||
Abstract
Odontoidectomy is indicated for some cases of ventral compression in the upper cervical spine. In this paper, we discuss the indications, surgical steps, and nuances of transoral odondoidectomy (TO) and endoscopic endonasal (EE) odontoidectomy. We compare both approaches and discuss the advantages and disadvantages of each. A broad narrative literature review was performed. We also added tips and surgical pearls of the senior author (KDR) in performing odontoidectomies. Surgical techniques were presented. EE is performed in patients where the dens is located above the nasopalatine line. Although technically more demanding, EE has less soft tissue injury and potentially less risk of dysphonia and dysphagia. The TO approach provides a wider exposure and is not limited by the nasopalatine line. Additionally, the TO approach allows the ability for a more extensive resection of C2; these could include the C2 body and the C2–3 disc space. Ventral reconstructions with cages and plates are also feasible via the TO approach. However, there are additional risks of prolonged intubation and tracheostomy with the TO approach. Surgeons who manage upper cervical spine disease should be comfortable performing both approaches, and selecting the best approach should be determined using patient-specific characteristics.
Anterior approaches to the upper cervical spine are used to treat a variety of pathologies, such as inflammatory diseases, traumatic injuries, congenital disorders, neoplastic and infectious conditions [1-5]. The most common indication for an anterior approach to the upper cervical spine is spinal cord compression caused by an inflammatory pannus (generally in atlantoaxial joint in context of rheumatoid arthritis [RA]) and congenital craniovertebral junction (CVJ) anomalies, such as basilar invagination or fixed atlantoaxial dislocation [6,7]. Overall, the incidence of pannus formation in RA patients is decreasing due to better disease control with biologic medication [8,9]. Moreover, advancements in posterior CVJ fixation techniques allows indirect ventral decompression and avoids the morbidity associated with a ventral surgical approach in the majority of the cases. Considering this, the anterior approach to the upper cervical spine is generally indicated for: (1) patients with persistent neurologic symptoms after they have failed posterior surgery or (2) severe anterior compression that cannot be safely managed with a posterior only procedure [7].
The odontoid process of C2 is generally the most common bone structure that causes compression of the neural tissue in the upper cervical spine. Odontoidectomy can be performed by 2 main routes: the transoral approach or the endonasal approach using an endoscope. In this paper, we discuss the anatomic and biomechanics of the CVJ, the surgical steps, and pearls associated with the TO and EE approaches, and we provide a comparison between the 2 techniques.
The CVJ is responsible for about 50% of cervical rotation (mainly at C1–2), and about 30° of flexion and extension of the cervical spine [10]. This vast range of motion is strongly influenced by the unique anatomy of the joints that exist at C1 and C2; the occipital condyles are rounded structures that allow movements in the sagittal plane (flexion-extension – the largest contribution from any single joint in the cervical spine). There are limited axial rotation and lateral bending, and the articular joint surfaces of C1 and C2 allow a large degree of axial rotation around the dens (almost half of all of the cervical spine) [11,12]. This wide range of movement requires strong ligamentous support to preserve spine integrity. Both the skull and C1 rotate about the dens of C2, and this rotation is stabilized by the anterior arch of C1 and the transverse ligament [12,13]. The alar ligaments act as restraints by attaching the dens to the occipital condyle and therefore preventing the dens from excessive motion. When a pannus is encountered, it is generally developed either between the dens and the anterior arch of the atlas or between the dens and the transverse ligament [14,15].
Dickman et al. [11] performed odontoidectomies in cadaveric adult humans and baboon cervical spines, preserving the surrounding ligaments and bone structures. They reported that translational movements in the specimens increased in all directions after odontoidectomy (flexion, extension, and lateral bending), and the greatest subluxations were in the anteroposterior plane, averaging up to 12.7 mm of motion. The total range of motion significantly increases in all directions (flexion, extension, and lateral bending) after an odontoidectomy. Of note, axial rotation did not increase significantly; this is likely given that the normal axial rotation at C1–2 is generally high to begin with. Given the results of this study, we could infer that instability may occur either directly following an odontoidectomy, or in a delayed fashion.
It is well-accepted that a ventral dens resection will result in spinal instability (acute or delayed), therefore requiring posterior fixation. For most published studies, posterior cervical fixation and fusion are performed within the same surgical procedure, immediately following the dens resection. Interestingly, there are anecdotal reports suggesting that posterior fixation was not necessary in less extensive odontoidectomies (also called by some surgeons as “odontoid sparing decompression” - preserving the transverse ligament and the base of the dens) [16]. Even though these anecdotal reports exist, fatal instability after this procedure has been reported by Edwards et al. [17] In our practice, we generally recommended immediate stabilization following the ventral dens resection. If immediate stabilization is not medically possible, then we recommend halo-vest immobilization until it can be completed.
The degree of posterior fixation and the impact upon ventral brainstem pathology was reported upon by Chang et al. [18] in a retrospective series of patients who underwent an anterior odontoidectomy. These patients were evaluated based on whether they had a posterior fixation that did not include C1–2, versus those that did include C1–2 (e.g., an occipital–C1–2 fusion). They reported that ventral brainstem decompression was greater in patients who had a craniocervical fixation that included the C1–2 joints when compared to those patients with an occipital-subaxial cervical spine fusion.
Prior to surgery, a clinical assessment should include an evaluation of the patient’s ability to open their mouth at least 5–6 cm; this is necessary in order to evaluate the access corridor to the posterior oral pharynx (a practical tip is the mouth should open enough in order to allow 3 fingerbreadths between the upper and lower rows of teeth). Patients are recommended to have an evaluation by a dentist to make sure that there is no infection.
Antibiotics covering the oral and skin flora and posterior oral pharynx are given. In the United States, oral anaerobes are often resistant to high-dose penicillin. Alternatives are ampicillin-sulbactam or clindamycin. We place plastic drapes around the mouth, to drape out the nose and neck and prep the skin around the mouth with normal cleansing material. To cleanse the oral cavity, we fill it with betadine, with the patient placed in reverse Trendelenburg position (to prevent leakage into the lung). The betadine is left in place until after the draping is completed.
A preoperative lumbar drain may be considered in patients with intradural pathology, or in cases where there is evidence of a cerebrospinal fluid (CSF) leak. Given that the etiology often involves brainstem and upper cervical compression, neurophysiological monitoring is advisable to increase the safety of positioning for this procedure.
The patient is then intubated orally by a flexible endotracheal tube (the tube is placed away from the midline to provide access for a nasal tube, or some authors prefer nasal intubation instead); extubation is only performed after a minimum of 24 hours, or after perioral swelling has resolved. A nasogastric tube is useful for secretion management from the patient’s gastric contents, and it can also be used postoperatively for feeding. A tracheostomy is considered by many authors, but we generally do not require this. Head fixation is not mandatory, but some head extension is recommended.
We do not cut the soft palate unless the clivus needs to be exposed, but we do take measures for retracting the uvula out of the surgical corridor. To achieve this, we insert the tip of a small nasogastric tube threaded through the nare into the posterior oropharynx and suture the midsubstance of the uvula to the nasogastric tube, which can then be pulled back and retracted out of the operative window into the nasopharynx. This allows the uvula to be retracted cranially and increases surgical exposure. In exceptional cases, where exposure of the superior clivus is necessary, one side of the soft palate can be excised for further retraction.
Following draping, which includes the entire patient except for the mouth, we suck out the betadine that had been placed into the oral cavity. The patient can then be taken out of the Trendelenburg position.
Our preference for retraction is the Aesculap’s transoral retractor, which provides retraction of the endotracheal tube, the tongue, and the posterior oral pharynx mucosa (Aesculap, 1000 Gateway Blvd., South San Francisco, CA, USA).
The anterior ring of C1 is easily palpated by the surgeon within the posterior oral pharynx. A direct longitudinal incision (2 to 3 cm) is made centered upon the anterior tubercle, but a semicircular mucosal flap may be recommended for more extensive procedures requiring a wider corridor. It is important to stay in the midline to avoid and minimize excessive bleeding.
We start the decompression by removing the anterior arch of C1. In many cases, the cranial 25% of the C1 anterior arch can be preserved. One only needs to resect the minimum amount necessary to transect and remove the dens. If the entire anterior arch requires removal, approximately 1.5-cm width of bone is generally sufficient. Visualizing the shoulder of the base of the odontoid is advisable at this point. The dens can then be resected in 2 ways: (1) amputating its base and removal en bloc in cases of basilar invagination, or (2) using a high-speed burr and removing it piecemeal in cases of a retro-dental mass such as pannus (generally with a side-cutting matchstick burr). In cases of basilar invagination, it is preferable to drill and place a few threads of tap into the dens before transecting the base of the dens. This prevents its retraction cranially after the base of the dens is cut and allows one to control and extract the dens easily. Alternatively, some surgeons advocate for the removal of the dens to be performed in a cranial to caudal direction, to avoid upward migration of the tip of the dens. The apical and alar ligaments, which are attached to the tip of the dens, are transected to allow for removal of the dens. A complete dens resection is considered the removal of both the apical and alar ligaments, the tectorial membrane, the transverse ligament and exposure of the dural surface. Some authors recommend against dural visualization after bone removal to avoid the risk of a dural leak; this recommendation is often coupled with the fact that pannus regression is expected after posterior upper cervical spine stabilization. To assess the completeness of the decompression, if the dura is not visualized, some surgeons have recommended filling the space with radiopaque dye.
We strongly advocate for the use of the microscope to increase safety and efficacy and to provide better visualization of structures. Since we generally continue the decompression until the transverse ligament is resected and the dura is visualized, the use of an operating microscope minimizes the risk of dural injury. The anatomical limits of the decompression are the hypoglossal nerves, the vertebral arteries, and the Eustachian tubes.
Although some believe that closure of the mucosa of the posterior pharynx is not mandatory, we close this space using a buried knot with 3-0 chromic sutures. This allows for rapid resumption of oral feeding.
Intraoperative dural tears are managed with a combination of a lumbar drain, local fibrin glue, and fat or fascial grafts. Meningitis can also occur, and it is an important complication. The vertebral artery is the anatomical limit of the corridor. Therefore injury to these vessels may result in intraoperative hemorrhage, the possibility of an ischemic stroke, and often endovascular intervention following the injury. A dedicated arterial study in cases of congenital anomalies is advisable. One should avoid excessive lateral exposure and bone removal.
Soft palate incisions may cause dysphonia, and it is because of this reason that we avoid opening the soft palate. Local complications due to retractors are also important considerations, such as tongue necrosis, broken teeth, soft tissue edema, and airway compromise; any isolated or combination of these could result in hypoxia and potentially could require a tracheostomy. To avoid these complications, the placement of the retractors should be done carefully, and all measures should be taken to avoid extubation while the soft tissues are edematous.
Acute infection of the teeth, nose, mouth, or pharynx is an absolute contraindication for using the TO approach for decompression. Also, the poor dental condition is a relative contraindication, and it is recommended to have any oral treatment that may be required before undergoing surgery for an odontoidectomy. Vascular anomalies, such as a ventral midline vertebral artery, is also a relative contraindication. Intradural pathology is a relative contraindication due to the high risk of postoperative infection.
Very high odontoids, such as in the context of clival hypoplasia, cannot be easily assessed using the TO approach; in these instances, the EE approach may be more suitable for an odontoid resection.
(1) Patients should have concomitant posterior instrumented craniocervical fusion (ideally in the same surgical procedure, flipped with a rigid cervical collar).
(2) Rigid cervical collar or halo may be used according to the degree of instability, bone quality, and risk factors for pseudoarthrosis.
(3) Oral feeding can be resume immediately for the majority of patients whose incisions are closed; complex procedures or those with significant local edema may require to tube feeding until the edema resolves.
(4) Extubation is advised when the oral and pharynx swelling are controlled. If any concerns exist, extubation should be postponed.
The endoscopic endonasal approach was first described in 2005 by Kassam et al. [19], and it provides a good alternative to the transoral approach for an odontoidectomy. The nasopalatine line is identified using a sagittal image and connecting from the most inferior point of the nasal bone to the posterior edge of the hard palate; the projected line identifies the inferior limit of the exposure. It also is a useful anatomical parameter to evaluate the degree of resection that can be achieved of the odontoid using a transnasal approach. Figs. 1 and 2 illustrate the nasopalatine line.
The patient is positioned with the head in rigid fixation, in flexion, and rotated ipsilaterally to the side of approach (generally right-sided approach). Neuronavigation can be utilized for improved anatomical orientation.
Orotracheal intubation is performed, and then the nostril cavity is prepared with betadine solution. Antibiotics prophylaxis is administered around 30 minutes before making an incision. We prefer 15- to 18-cm endoscopes, which are 0° with a 4-mm diameter irrigation sheath. A binostril approach is utilized as the working corridor, generally with the endoscope in the right nostril and the working instruments in the left. The posterior and caudal portion of the nasal septum is then resected. Additionally, if the working corridor is too narrow, the right middle turbinate can also be resected. Once at the choana, the endoscope is direct to the base of the odontoid. The incision then made in the posterior oral pharynx; a linear midline incision or an inverted U-shaped incision can be made. Neuronavigation is used when selected the location where to incise, and the overlying longus colli and longus capitis are reflected laterally. We generally reflect this musculature using the monopolar electrocautery. A subperiosteal exposure of the anterior arch of C1 and the base of the odontoid is then performed. Similar to a transoral odontoidectomy, the arch of C1 is drilled first, followed by the dens. The ligamentous attachments are released at the apex of the dens. Kerrison’s are useful for removing residual posterior cortical bone, as well as the use of the high-speed drill. If a mucosal flap was harvested and planned to cover the defect, a biologic sealant is used to secure the mucosal flap. Also, a balloon-inflated Foley catheter is placed that will rest against the flap.
Similar adverse events can occur with the endoscopic endonasal odontoidectomy as were previously described for the TO approach. These include infection, dural tears, and vertebral artery injury. Local complications due to retractors are less common, such as tongue and tooth injuries. Finally, managing local mucosal bleeding can be quite severe, requiring nasal packing.
(1) Patients should have concomitant posterior instrumented craniocervical fusion (ideally in the same surgical procedure, flipped with a rigid cervical collar).
(2) A rigid cervical collar or a halo may be used according to the degree of instability, bone quality, risk factors for pseudoarthrosis.
(3) Oral feeding can be resumed immediately following surgery for most patients.
(4) The Foley catheter and nasal pack are removed on postoperative day 2.
There are several limitations when utilizing the EE approach. These include having a lower limit of resection that is determined by the nasopalatine line; generally, access to the C2–3 disc is unachievable. Also, a C2 corpectomy is often beyond the bounds of limits of the operative corridor and cannot be achieved. Ventral reconstruction of the axis with a plate or cage are also not possible. Direct dural repairs in the setting of a dural tear are challenging. Lastly, the Eustachian tube limits the extent of the lateral resection. Figs. 3 and 4 illustrate the limitation of each approach.
Shriver et al. [20] performed a systematic review and meta-analysis comparing complications of TO versus EE odontoidectomy. Complications included arterial injury, CSF leak, infection, sepses, reoperation, among many others. A total of 26 articles were included and analyzed. The only significant statistical difference in complications was the risk of postoperative tracheostomy, which was higher in the TO approach.
Ponce-Gómez et al. [21] reported the results of 12 patients who had an odontoidectomy performed. The EE approach for odontoidectomy was used in 5 patients, which the odontoid was above the nasopalatine line. The remaining 7 patients that underwent an odontoidectomy using the TO approach had the odontoid located below the nasopalatine line. Both groups had a similar neurological outcome. Complications in the TO group included 2 patients with postoperative dysphonia, 1 with dysphagia, and 1 with a CSF leak. Both dysphonia and dysphagia improved in the first 2 weeks after surgery. Although the EE group had longer operative times (238 minutes on average vs. 141 minutes in TO, p<0.02), the EE group were extubated sooner than the TO group (all patients were extubated immediately following surgery who had EE, whereas 6 were extubated at 24 hours and one at 48 hours in the TO group). Time to resuming oral feeding after surgery was also shorter in the EE group (p<0.009), the EE group had an overall shorter hospital stay, and there were no complications reported.
The comparison of transoral versus endoscopic endonasal odontoidectomy is presented in Table 1.
Although not addressed in this review, some authors described endoscopic odontoidectomy using a transoral approach [5]. In a small cases series, this approach was used successfully, and it is an alternative to the traditional TO and EE odontoidectomies. This approach was likely derived from its prior use for the resection of clivus chordomas, and its usefulness for odontoidectomies would require further investigation.
Both TO and EE approaches are acceptable surgical options for ventral odontoidectomies. Both approaches have unique characteristics that can be tailored individually to patients based on their anatomical and pathological constraints. Surgeons who treat CVJ diseases should be familiar with these nuances, as well as the specific advantages for selecting the best management strategies when treating these complex diseases.
Fig. 1.
(A) The red line represents the nasopalatine line. Only the portion above the red line (yellow area) can be accessed using an endoscopic endonasal approach. (B) In this patient, there is a clivus hypoplasia, and the tip of the dens is quite high. Considering as the dens is completely above the nasopalatine line (red), an endoscopic endonasal approach is preferential to a transoral route for dens resection.
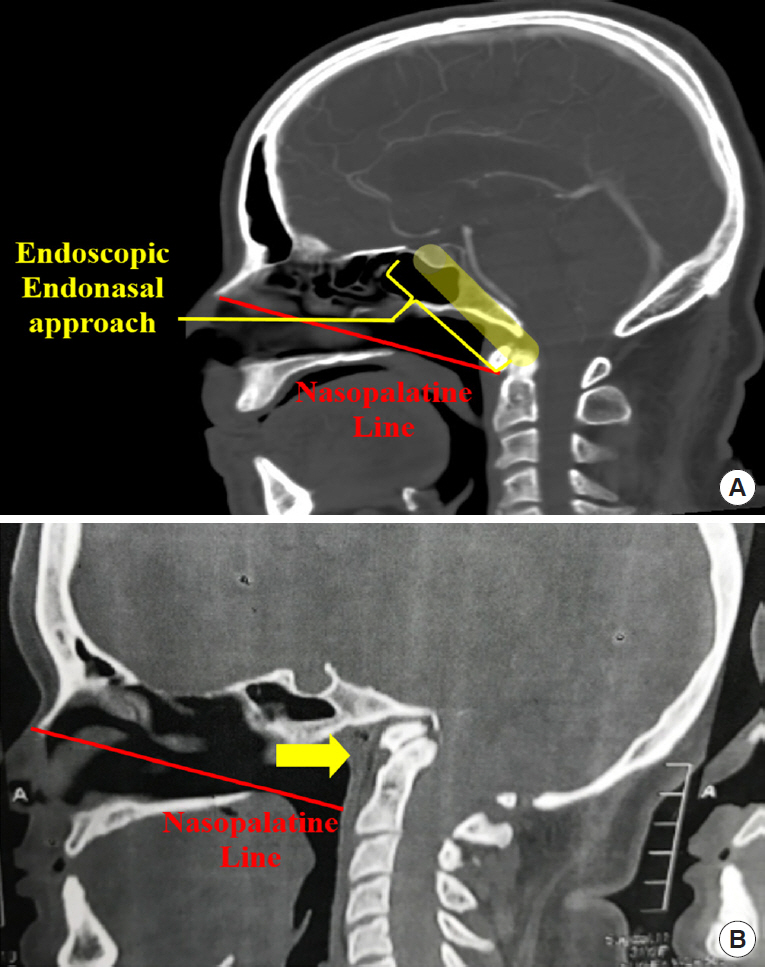
Fig. 2.
Comparative picture of the anterior approaches to the
craniocervical junction and their anatomical limits. Yellow area: can be preferentially accessed using an endoscopic endonasal route; Red area: can be preferentially accessed with a transoral approach – and some upper extension is possible (into the yellow area) if the soft palate is incised. Blue area: a transcervical route is feasible and a good surgical option.
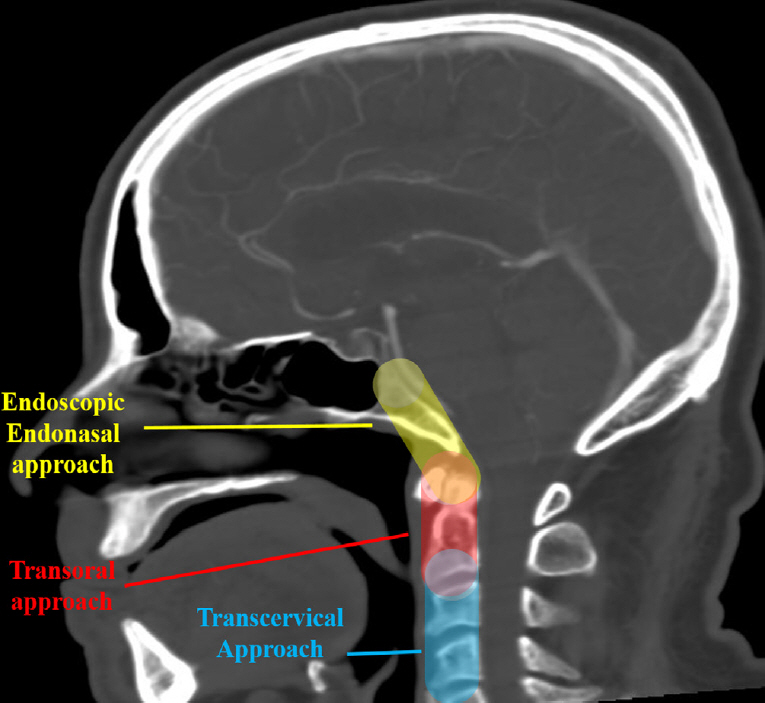
Fig. 3.
Transoral odontoid resection in a patient with a basilar invagination with atlanto axial dislocation with ventral compression. (A) Preoperative sagittal T2 sequence magnetic resonance imaging. (B) Preoperative sagittal computed tomography (CT). (C) Postoperative CT. (D) Intraoperative X-ray showing drill depth. (E) Intraoperative retractor.

Fig. 4.
Endoscopic endonasal odontoid resection in a patient with ventral brainstem compression. (A) Preoperative sagittal T2 sequence magnetic resonance imaging. (B) Preoperative sagittal computed tomography (CT). (C) Postoperative sagittal CT. (D) Intraoperative navigation showing endoscope position. (E) Intraoperative endoscopic view.
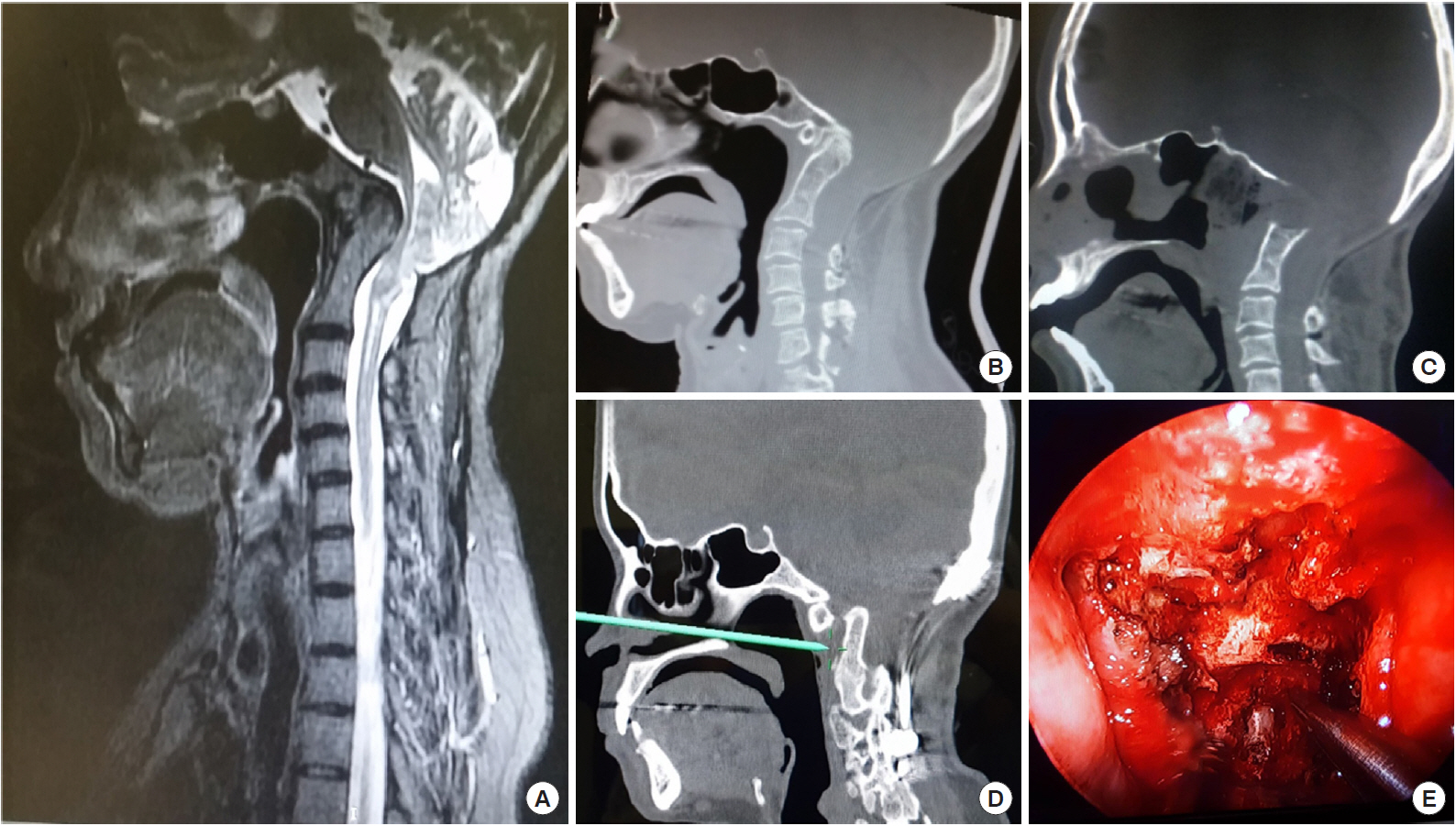
Table 1.
Comparison of the transoral odontoidectomy (TO) versus endoscopic endonasal (EE) odontoidectomy – authors perspectives
REFERENCES
1. Alonso WA, Black P, Connor GH, et al. Transoral transpalatal approach for resection of clival chordoma. Laryngoscope 1971 81:1626-31.


2. Crockard HA. The transoral approach to the base of the brain and upper cervical cord. Ann R Coll Surg Engl 1985 67:321-5.


3. Kerschbaumer F, Kandziora F, Klein C, et al. Transoral decompression, anterior plate fixation, and posterior wire fusion for irreducible atlantoaxial kyphosis in rheumatoid arthritis. Spine (Phila Pa 1976) 2000 25:2708-15.


4. Apuzzo ML, Weiss MH, Heiden JS. Transoral exposure of the atlantoaxial region. Neurosurgery 1978 3:201-7.



5. Qiuhang Z, Feng K, Bo Y, et al. Transoral endoscopic odontoidectomy to decompress the cervicomedullary junction. Spine (Phila Pa 1976) 2013 38:E901-6.


6. Sukoff MH, Kadin MM, Moran T. Transoral decompression for myelopathy caused by rheumatoid arithritis of the cervical spine. Case report. J Neurosurg 1972 37:493-7.


7. Joaquim AF, Tedeschi H, Chandra PS. Controversies in the surgical management of congenital craniocervical junction disorders - a critical review. Neurol India 2018 66:1003-15.


8. Kaito T, Hosono N, Ohshima S, et al. Effect of biological agents on cervical spine lesions in rheumatoid arthritis. Spine (Phila Pa 1976) 2012 37:1742-6.


9. Kaito T, Ohshima S, Fujiwara H, et al. Predictors for the progression of cervical lesion in rheumatoid arthritis under the treatment of biological agents. Spine (Phila Pa 1976) 2013 38:2258-63.


10. Tubbs RS, Hallock JD, Radcliff V, et al. Ligaments of the craniocervical junction. J Neurosurg Spine 2011 14:697-709.


11. Dickman CA, Crawford NR, Brantley AG, et al. Biomechanical effects of transoral odontoidectomy. Neurosurgery 1995 36:1146-52.



12. Dickman CA, Locantro J, Fessler RG. The influence of transoral odontoid resection on stability of the craniovertebral junction. J Neurosurg 1992 77:525-30.


13. Dvorak J, Schneider E, Saldinger P, et al. Biomechanics of the craniocervical region: the alar and transverse ligaments. J Orthop Res 1988 6:452-61.


14. Young WF, Boyko O. Magnetic resonance imaging confirmation of resolution of periodontoid pannus formation following C1/C2 posterior transarticular screw fixation. J Clin Neurosci 2002 9:434-6.


15. Grob D, Würsch R, Grauer W, et al. Atlantoaxial fusion and retrodental pannus in rheumatoid arthritis. Spine (Phila Pa 1976) 1997 22:1580-3.


16. Vitali M, Canevari FR, Cattalani A, et al. Stability-sparing endoscopic endonasal odontoidectomy in a malformative craniovertebral junction: case report and biomechanical considerations. Acta Neurochir Suppl 2019 125:229-33.


17. Edwards RJ, Britz GW, Johnston FG. Fatal instability following “odontoid sparing” transoral decompression of a periodontoid pseudotumour. J Neurol Neurosurg Psychiatry 2002 73:756-8.



18. Chang PY, Yen YS, Wu JC, et al. The importance of atlantoaxial fixation after odontoidectomy. J Neurosurg Spine 2016 24:300-8.


19. Kassam AB, Snyderman C, Gardner P, et al. The expanded endonasal approach: a fully endoscopic transnasal approach and resection of the odontoid process: technical case report. Neurosurgery 2005 57(1 Suppl):E213.



































