- Search
| Neurospine > Volume 18(3); 2021 > Article |
|
|
See commentary "Commentary on “Characteristics and Risk Factors of Rod Fracture Following Adult Spinal Deformity Surgery: A Systematic Review and Meta-Analysis”" in Volume 18 on page 455.
Abstract
Objective
The aim of study is to investigate the features and risk factors of rod fracture (RF) following adult spinal deformity (ASD) surgery.
Methods
We searched the PubMed, Embase, Web of Science, and Cochrane Library databases to identify relevant studies. Patient’s data including age, sex, body mass index (BMI), previous spine surgery, pedicle subtraction osteotomy (PSO), interbody fusion, fusion to the pelvis, smoking history, preoperative sagittal vertical axis (SVA), preoperative pelvic tilt (PT), preoperative pelvic incidence minus lumbar lordosis, preoperative thoracic kyphosis (TK), and change in the SVA were documented. Comparable factors were evaluated using odds ratio (OR) and weighted mean difference (WMD) with 95% confidence interval (CI).
Results
Seven studies were included. The overall incidence of RF following ASD surgery was 12%. Advanced age (WMD, 2.8; 95% CI, 1.01–4.59; p<0.002), higher BMI (WMD, 1.98; 95% CI, 0.65–3.31; p=0.004), previous spine surgery (OR, 1.47; 95% CI, 1.05–2.04; p=0.02), PSO (OR, 2.28; 95% CI, 1.62–3.19; p<0.0001), a larger preoperative PT (WMD, 6.17; 95% CI, 3.55–8.97; p<0.00001), and a larger preoperative TK (WMD, 5.19; 95% CI, 1.41–8.98; p=0.007) were identified as risk factors for incidence of RF.
Conclusion
The incidence of RF in patients following ASD surgery was 12%. Advanced age, higher BMI, previous spine surgery, and PSO were significantly associated with an increased occurrence of RF. A larger preoperative PT and TK were also identified as risk factors for occurrence of RF following ASD surgery.
Compared with other spinal diseases, adult spinal deformity (ASD) has a significant impact on a patient’s quality of life. Treatment of ASD has evolved significantly over the past decade and involves improved spinal instrumentation, surgical techniques, and perioperative management. Thus far, the data shows that selected adults with spinal deformities have great potential for improvement following surgical treatment; however, the overall rate of complications is still high, indicating scope for improvement [1]. Mechanical complications that may occur following ASD surgery include proximal junctional kyphosis (PJK), proximal junctional failure (PJF), distal junctional kyphosis, distal junctional failure, rod fracture (RF), and other implant-related complications. RF is a frequent implant-related complication of ASD surgery [2]. It causes significant pain and deterioration of spinal alignment, which can then adversely affect clinical outcomes and the patient’s mental health [3]. The incidence of RF following ASD surgery in symptomatic RF patients has been reported by Smith et al. as 6.8% [4]. Another study by Smith et al. [5] reported that 9% of the patients who underwent ASD surgery developed RF at a mean of 14.7 months postsurgery, and 22% of the patients who underwent pedicle subtraction osteotomy (PSO) developed RF by the their 1-year follow-up. To date, extensive research has been conducted on PJK and PJF, but research on RF is lacking. To the best of our knowledge, no study has summarized the characteristics of RF, which is essential for understanding this complication. Through this systematic review and meta-analysis, we analyzed the characteristics and risk factors of RF following ASD surgery, in order to expand the literature available on this complication
We searched the PubMed, Embase, Web of Science, and Cochrane Library databases to identify differences between the groups with and without RFs and to investigate risk factors for RF in patients who underwent ASD surgery. The Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines were followed. The search terms included: “adult spinal deformity” OR “ASD” AND “rod fracture” OR “RF”. The language was restricted to English, and only published articles were considered. The studies were then screened by 2 authors independently based on the inclusion and exclusion criteria, and data on the risk factors were collected from the eligible studies. We also searched the reference lists of the selected studies, reviews, or comments to identify any other relevant studies.
To assess the suitability of a study, the Population Intervention, Comparative Results and Study Design methodology and PRISMA guidelines were applied [6]. The inclusion criteria for our meta-analysis were: (1) the patient was diagnosed with ASD and underwent ASD surgery, (2) had more than 1-year follow-up, (3) ASD patients with RF, (4) retrospective or prospective studies comparing risk factors between patients with and without RFs, and (5) sufficient data was available (the mean±standard deviations of continuous variables and the number of count variables). The exclusion criteria were as follows: (1) ASD patients resulting from secondary disease such as autoimmune diseases, infectious disease, tumors, or other pathological conditions, and adolescent idiopathic scoliosis; (2) available data was not reported; and (3) duplicate reports and review articles.
Data were extracted from eligible studies by 2 authors (SHN, DKC) according to the inclusion and exclusion criteria. In case of discrepancies, consensus was reached through discussion. The extracted data included information on study design, patient characteristics, sample size, detailed follow-up information, intervention time, and results. All relevant data reported in each eligible study, including the demographic factors, surgical variables, and the preoperative and postoperative radiological parameters, were collected and analyzed, and the risk factors for RF were investigated. Radiological parameters at the time of follow-up were analyzed to detect the characteristics of RF in ASD patients.
The Newcastle-Ottawa Quality Assessment Scale (NOQAS) was used to assess the quality of each included study, as most were nonrandom comparative studies [7]. The NOQAS consists of 3 major assessment categories (selection, comparability, and exposure). A maximum of 9 stars could be assigned to a study, and more than 6 stars in the final score indicated high quality.
This meta-analysis employed Review Manager Software 5.3 (Cochrane Collaboration, Oxford, UK). Funnel plots were marked using Meta Essentials. Effect size of the continuous data was measured using weighted mean differences (WMDs) and the corresponding 95% confidence interval (CI). Effect size of the variable data was calculated using a 95% CI corresponding to an odds ratio (OR). Heterogeneity among studies was evaluated according to the I2 index. If there was serious heterogeneity between studies, pooled effect size was calculated using a random-effect model (p<0.05 or I2>50%); otherwise, a fixed-effect model was applied. A p-value of < 0.05 was considered significant.
A total of 191 studies were originally found in the PubMed (91), Embase (60), Web of Science (38), and Cochrane Library (2) databases. Ninety-nine studies remained after duplicate trials were excluded. After reviewing the titles and summaries, 20 studies were removed, and 55 studies were excluded in accordance with the exclusion criteria. Ten studies were eliminated due to inadequate data. Finally, 7 studies were selected for this meta-analysis. Fig. 1 shows the document selection process. The follow-up period of all studies was more than 12 months. The study characteristics are summarized in Table 1.
Based on the NOQAS, 6 studies scored 8 points, and 1 study scored 7 points (Table 2). Thus, the quality of each study was relatively high.
A total of 209 patients developed RF following ASD surgery. Based on the 7 studies, the overall incidence of RF following ASD surgery was 12%. As presented in 6 papers, RF developed after a mean time of 23.2 months after ASD surgery.
Among the demographic risk factors, advanced age (WMD, 2.8; 95% CI, 1.01–4.59; p<0.002), higher body mass index (BMI) (WMD, 1.98; 95% CI, 0.65–3.31; p=0.004), and prior spinal surgery (OR, 1.47; 95% CI, 1.05–2.04; p=0.02) were significantly associated with RF (Figs. 2–4). Among the surgical risk factors, PSO (OR, 2.28; 95% CI, 1.62–3.19; p<0.0001) was significantly associated with RF (Fig. 5). Among the radiologic risk factors, larger preoperative pelvic tilt (PT) (WMD, 6.17; 95% CI, 3.55–8.97; p<0.00001) and larger preoperative thoracic kyphosis (TK) (WMD, 5.19; 95% CI, 1.41–8.98; p=0.007) were identified as risk factors for RF (Figs. 6, 7). Sex, the number of fused segments, osteoporosis/osteopenia, interbody fusion, fusion to pelvis, rod diameter, rod materials, smoking history, preoperative sagittal vertical axis (SVA), change of SVA, and preoperative pelvic incidence minus lumbar lordosis (PI–LL) did not differ significantly between the groups with and without RF. Table 3 shows the number of studies that reported each risk factor and the results of our forest plot.
All funnel plots were symmetric, indicating an absence of significant publication bias among the studies. The Egger test results for each risk factors were age (p=0.8803), BMI (p=0.9248), prior spine surgery (p=0.0526), PSO (p=0.2636), preoperative PT (p=0.7836), and preoperative TK (p=0.7382). These results show that there is no real evidence of publication bias in the data set.
ASD surgery techniques have advanced in the past decade. The results of ASD surgery are constantly improving, but a high proportion of major complications following this surgery still persist. This meta-analysis was performed to evaluate the characteristics and risk factors of RF following ASD surgery.
Among the demographic factors, age, BMI, and previous spinal surgery were the risk factors associated with RF. Smith et al. [5], Lertudomphonwanit et al. [7], and Daniels et al. [8] reported that age and BMI had a statistically significant effect on the incidence of RF. Smith et al. [5] also reported that previous spinal surgery was significantly associated with RF. In our meta-analysis, advanced age and high BMI were significantly associated with a high incidence of RF. Patients who had undergone previous spine surgeries were also more likely to develop RF (OR, 1.47; 95% CI, 1.05–2.04; p=0.02). Among the demographic factors, sex, bone mineral density (BMD), and smoking history were not significantly associated with the incidence of RF. And Charlson Comorbidity Index (CCI) was also not statistically significant. The CCI was first developed by Mary Charlson and colleagues in 1987 as a weighted index to predict the risk of death within one year of hospitalization for patients with certain comorbid diseases [9]. However, osteoporosis and smoking history are known to be risk factors for mechanical complications after ASD [10]. Yagi et al. [11] said that low BMD (T score< -1.5) is a meaningful risk factor for PJF in ASD surgery. These factors are not statistically related to RF in each article, but are related to other mechanical complications such as pseudoarthrosis and other implant-related problems [10]. Therefore, it is necessary to quit smoking or increase BMD in ASD surgery. And Yilgor et al. [12] created a Global Alignment and Proportion score (GAP) system that predicts mechanical complication after ASD surgery, where sacral slope and lower lumbar lordosis distribution were reported as risk factors for mechanical complication. And Noh et al. [13] made GAPB system in which BMI and BMD were added to the GAP system, and reported that the higher the BMI and the lower the BMD, as well as the GAP score, the greater the risk of mechanical complications. Therefore, it is difficult to say that the ASD surgery was successful when there was no RF. Therefore, the efforts are needed to reduce mechanical complications after ASD surgery.
Among the surgical factors, PSO and a larger number of fused segments had statistically significant influences on RF. These results are in accordance with several studies that reported a statistically significant influence of PSO on RF [2,5,8,14]. Smith et al. [5] reported that RF occurred in 22.0% of the patients who underwent PSO and in 4.7% of those who did not; they also stated that PSO is a powerful way to drastically correct discrepancy in the sagittal spinopelvic alignment and that this added force is likely to contribute to an increase in the incidence of RF in these cases. Moreover, Bridwell et al. [15] and Upadhyaya et al. [16] have documented cases of RF associated with PSO. During PSO, an interbody fusion is performed to provide anterior support or multiple rods are inserted at the PSO site to reduce the chances of RF occurrence [17]. In the study by Lertudomphonwanit et al. [7], the proportion of RF patients who underwent PSO was high, but the difference in the RF incidence was not statistically significant. This was because multirod structures were used at the osteotomy site, interbody fusion was performed at the segment adjacent to the osteotomy site, and high doses of recombinant human bone morphogenetic protein-2 (rhBMP-2) and sufficient autologous bone grafts were used [7]. Lertudomphonwanit et al. [7] reported that a longer fused segment was associated with RF occurrence. Specifically, for patients receiving a high dose of rhBMP-2 per level fused, the total number of levels fused was not a significant risk factor for RF, but for patients receiving a low dose of rhBMP-2 per level fused, it was a significant risk factor. In our meta-analysis, PSO (OR, 2.28; 95% CI, 1.62–3.19; p<0.0001) was shown to be a risk factor of RF. However, a longer fused segment (WMD, 1.01; 95% CI, -2.70 to 4.72; p=0.59) was not significantly associated with RF.
Among the intraoperative factors, interbody fusion, cross link, fusion to the pelvis, and approach to interbody fusion were not significantly associated with the incidence of RF. Regarding rod diameter, Smith et al. [4], Daniels et al. [8], and Lertudomphonwanit et al. [7] individually compared rods with diameters of 5.5 mm, 6.0 mm, and 6.35 mm. The 5.5-mm rod diameter induced more RF, but this result was not statistically significant in our metaanalysis. With respect to rod material, Smith et al. [5], Daniels et al. [8], and Lertudomphonwanit et al. [7] individually compared cobalt-chromium, stainless steel, and titanium alloy. Rods made of cobalt-chromium caused more RF, but this result was also not statistically significant in our meta-analysis.
Among the radiological factors, larger preoperative PT and TK had a statistically significant influence on occurrence of RF. A great amount of force is applied to the rod to correct a large preoperative PT and TK. Thus, inferior radiological parameters before the surgery may cause an increased incidence of RF. In our meta-analysis, larger preoperative PT (WMD, 6.17; 95% CI, 3.55–8.97; p<0.00001) and larger preoperative TK (WMD, 5.19; 95% CI, 1.41–8.98; p=0.007) were the risk factors associated with RF. We found preoperative SVA, change of SVA, and PI–LL were not significantly associated with RF.
Several papers have proposed methods to reduce RF [18-21]. Gupta et al. [19] recommended the 4-rod technique for the PSO site. The point of maximum stress on the body is at its apex, where the spine becomes unstable by osteotomy. As such, RF usually occurs at the osteotomy site. The advantage of the 4-rod technique is that it does not require a surgeon to bend the rod sharply at the PSO site over the length of the fusion. This technique also helps to significantly reduce the potential for premature RF due to biomechanical damage of the rod [20]. Banno et al. [18] reported that multirod structure use improved stability compared to use of the standard 2-rod structure, which was effective in preventing implant failure and symptomatic pseudarthrosis.
There were some limitations to this meta-analysis. First, only 7 matching studies were selected, and most of them were retrospective, which may have affected the reliability of our results. Second, patients, surgical adaptations, and techniques may have varied in each center. Finally, other factors commonly considered, such as rod diameter, rod material, access to intervertebral fusion, CCI were not considered in the analysis due to insufficient data. Despite these limitations, the results from this study will broaden the understanding of RF and provide potential guidance for the prevention of RF after ASD surgery. However, further studies are required to form a comprehensive understanding of RF incidence and risk factors among patients with ASD.
The incidence of RF following ASD surgery was 12%. Advanced age, higher BMI, previous spine surgery, and PSO were significantly associated with an increased occurrence of RF. Larger preoperative PT and TK were also identified as risk factors for RF following ASD surgery. Surgeons should ensure they understand these risk factors before performing ASD surgery.
Fig. 2.
Forest plot showing the relationship between age and rod fracture occurrence. SD, standard deviation; df, degrees of freedom; CI, confidence interval.
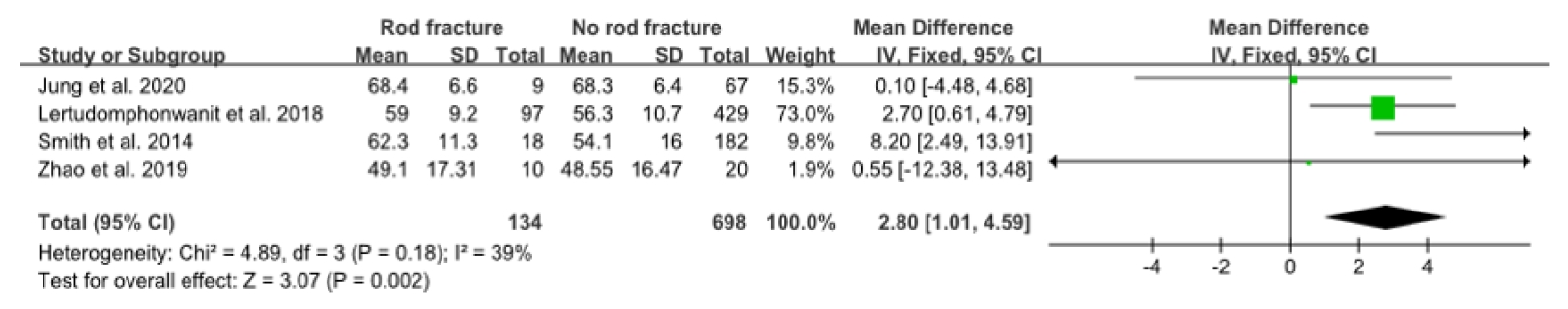
Fig. 3.
Forest plot showing the relationship between body mass index and rod fracture occurrence. SD, standard deviation; CI, confidence interval; df, degrees of freedom.
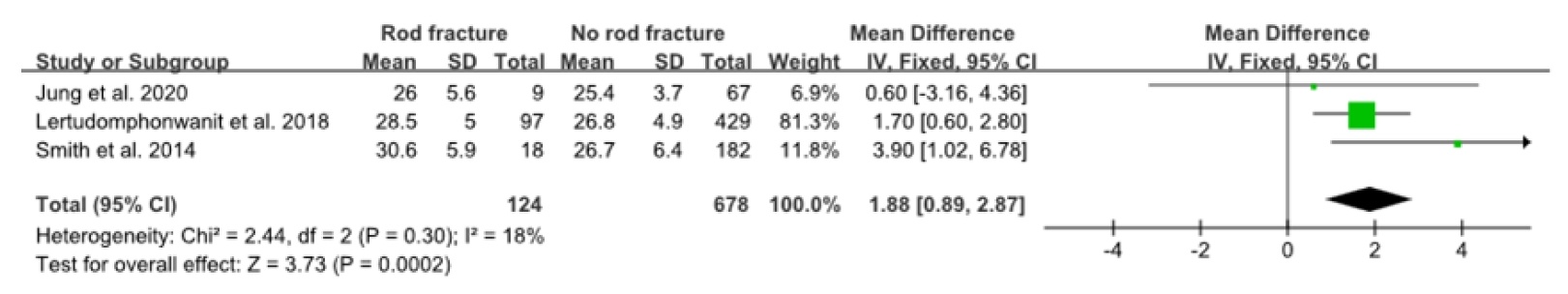
Fig. 4.
Forest plot showing the relationship between prior spine surgery and rod fracture occurrence. df, degrees of freedom; CI, confidence interval.

Fig. 5.
Forest plot showing the relationship between pedicle subtraction osteotomy and rod fracture occurrence. df, degrees of freedom; CI, confidence interval.

Fig. 6.
Forest plot showing the relationship between preoperative pelvic tilt and rod fracture occurrence. df, degrees of freedom; CI, confidence interval.

Fig. 7.
Forest plot showing the relationship between preoperative thoracic kyphosis and rod fracture occurrence. SD, standard deviation; CI, confidence interval; df, degrees of freedom.

Table 1.
Characteristics of studies included in the meta-analysis
| Study | Year | Country | Type of scoliosis | Study period | Rod Fx. | No rod Fx. | Mean age (yr) | Mean fusion level | Mean period from surgery to rod fracture (mo) | F/U period (mo) | Study type |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Smith et al. [4] | 2012 | USA | ASD | 2004–2010 | 30 | 412 | Rod Fx. 61 (29–79) | ND | 15.7 (2–73) | ≥ 12 | Retrospective |
| Smith et al. [5] | 2014 | USA | ASD | ND | 18 | 182 | 54.8 ± 15.8 | 12 ± 4 | 14.7 (3–27) | ≥ 12 | Prospective |
| Barton et al. [2] | 2015 | USA | ASD | 2007–2014 | 7 | 68 | 59 ± 12.9 | ND | 20 (11–58) | ≥ 35 | Retrospective |
| Daniels et al. [8] | 2018 | USA | ASD | ND | 38 | 364 | 57.4 ± 14.8 | 11.1 ± 4.1 | ND | ≥ 24 | Retrospective |
| Lertudomphonwanit et al. [7] | 2018 | USA | ASD | 2004–2014 | 97 | 429 | 58.9 ± 9.2 | 14 (6–17) | 39.6 (6–121) | ≥ 24 | Retrospective |
| Zhao et al. [14] | 2019 | China | ASD | 2009–2017 | 10 | 20 | ND | ND | 22.1 (6–73) | ≥ 12 | Retrospective |
| Jung et al. [21] | 2020 | Korea | ASD | 2012–2018 | 9 | 67 | 68.7 | ND | 27.3 (20–42) | ≥ 12 | Retrospective |
Table 2.
Quality assessment of included studies in the metaanalysis according to Newcastle-Ottawa Quality Assessment Scale
| Study | Selection | Comparability | Exposure | Total score |
|---|---|---|---|---|
| Smith et al. [4] | 3 | 2 | 3 | 8 |
| Smith et al. [5] | 3 | 2 | 3 | 8 |
| Barton et al. [2] | 3 | 2 | 3 | 8 |
| Daniels et al. [8] | 3 | 2 | 3 | 8 |
| Lertudomphonwanit et al. [7] | 3 | 2 | 3 | 8 |
| Zhao et al. [14] | 2 | 2 | 3 | 7 |
| Jung et al. [21] | 3 | 2 | 3 | 8 |
Table 3.
Summary of related risk factors for rod fracture in adult spinal deformity surgery
REFERENCES
1. Smith JS, Shaffrey CI, Glassman SD, et al. Clinical and radiographic parameters that distinguish between the best and worst outcomes of scoliosis surgery for adults. Eur Spine J 2013 22:402-10.


2. Barton C, Noshchenko A, Patel V, et al. Risk factors for rod fracture after posterior correction of adult spinal deformity with osteotomy: a retrospective case-series. Scoliosis 2015 10:30.



3. Yamato Y, Hasegawa T, Kobayashi S, et al. Treatment strategy for rod fractures following corrective fusion surgery in adult spinal deformity depends on symptoms and local alignment change. J Neurosurg Spine 2018 29:59-67.


4. Smith JS, Shaffrey CI, Ames CP, et al. Assessment of symptomatic rod fracture after posterior instrumented fusion for adult spinal deformity. Neurosurgery 2012 71:862-8.


5. Smith JS, Shaffrey E, Klineberg E, et al. Prospective multicenter assessment of risk factors for rod fracture following surgery for adult spinal deformity. J Neurosurg Spine 2014 21:994-1003.


6. Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015 4:1.



7. Lertudomphonwanit T, Kelly MP, Bridwell KH, et al. Rod fracture in adult spinal deformity surgery fused to the sacrum: Prevalence, risk factors, and impact on health-related quality of life in 526 patients. Spine J 2018 18:1612-24.


8. Daniels AH, Durand W, Hamilton DK, et al. Wednesday, September 26, 2018 3:35 PM – 5:05 PM How to avoid complications: 101. Rod fracture following apparently solid radiographic fusion in adult spinal deformity patients. Spine J 2018 18:S48-9.
9. Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987 40:373-83.


10. Park S, Lee C, Chung S, et al. Different risk factors of proximal junctional kyphosis and proximal junctional failure following long instrumented fusion to the sacrum for adult spinal deformity: survivorship analysis of 160 patients. Neurosurgery 2017 80:279-86.


11. Yagi M, Fujita N, Tsuji O, et al. Low bone-mineral density is a significant risk for proximal junctional failure after surgical correction of adult spinal deformity: a propensity scorematched analysis. Spine 2018 43:485-91.

12. Yilgor C, Sogunmez N, Boissiere L, et al. Global Alignment and Proportion (GAP) score: development and validation of a new method of analyzing spinopelvic alignment to predict mechanical complications after adult spinal deformity surgery. J Bone and Joint Surg Am 2017 99:1661-72.

13. Noh SH, Ha Y, Obeid I, et al. Modified global alignment and proportion scoring with body mass index and bone mineral density (GAPB) for improving predictions of mechanical complications after adult spinal deformity surgery. Spine 2020 20:776-84.

14. Zhao J, Li B, Chen Z, et al. Rod fracture after long construct fusion in adult spinal deformity surgery: a retrospective case-control study. J Orthop Sci 2019 24:607-11.


15. Bridwell KH, Lewis SJ, Edwards C, et al. Complications and outcomes of pedicle subtraction osteotomies for fixed sagittal imbalance. Spine 2003 28:2093-101.


16. Upadhyaya CD, Berven S, Mumaneni PV. Spondylolisthesis following a pedicle subtraction osteotomy. Case report. Neurosurg Focus 2010 28:E16.
17. Charosky S, Moreno P, Maxy P. Instability and instrumentation failures after a PSO: a finite element analysis. Eur Spine J 2014 23:2340-9.


18. Banno T, Hasegawa T, Yamato Y, et al. Multi-rod constructs can increase the incidence of iliac screw loosening after surgery for adult spinal deformity. Asian Spine J 2019 13:500.



19. Gupta S, Eksi MS, Ames CP, et al. A novel 4-rod technique offers potential to reduce rod breakage and pseudarthrosis in pedicle subtraction osteotomies for adult spinal deformity correction. Oper Neurosurg (Hagerstown) 2018 14:449-56.



































