- Search
| Neurospine > Volume 19(3); 2022 > Article |
|
|
See commentary "Building a Successful Practice of Endoscopic Spine Surgery: Learning, Setting the Goal, and Expanding the Border" in Volume 19 on page 571.
Abstract
Objective
Percutaneous transforaminal endoscopic discectomy (PTED) is gaining popularity by both surgeons and patients as a less invasive treatment option for sciatica. Concerns, however, exist for its learning curve. No previous study has assessed the learning process of PTED. Hereby we present the learning process of 3 surgeons learning PTED.
Methods
This analysis was conducted alongside a multicenter randomized controlled trial. After attending a cadaveric workshop, 3 spine-dedicated surgeons started performing PTED, initially under the supervision of a senior surgeon. After each 5 cases, and up to case 20, the learning process was evaluated using the validated questionnaires (objective structured assessment of technical skills [OSATS], global operative assessment of laparoscopic skills [GOALS]) and a 10-step checklist specifically developed for PTED.
Results
In total, 3 learning curve surgeons performed a total of 161 cases. Based on self-assessment, surgeons improved mostly in the domains ŌĆ£time and motion,ŌĆØ ŌĆ£respect for tissue,ŌĆØ and ŌĆ£knowledge and handling of instruments.ŌĆØ Learning curve surgeons were more able to detect differences in performances on the OSATS than the senior surgeon. Based on the GOALS, the biggest improvements could be seen in ŌĆ£depth-perceptionŌĆØ and ŌĆ£autonomy.ŌĆØ Based on the 10-item specific checklist, all surgeons performed all 10 steps by case 10, while only 1 surgeon performed all steps adequately by case 15.
Conclusion
Based on these study results, PTED appears to be successfully adopted stepwise by 3 spine-dedicated surgeons. From 15 cases on, most steps are performed adequately. However, more cases might be necessary to achieve good clinical results. Validated tools are needed to determine the cutoff when a surgeon should be able to perform PTED independently.
Full-endoscopic spine surgery is gaining interest as a less invasive alternative to treat sciatica caused by a lumbar disc herniation [1-7]. Compared to microdiscectomy, which is regarded as the golden standard to treat sciatica, full-endoscopic procedures have a smaller incision, require less destruction of bony structures, and facilitate outpatient surgery [8-10]. On the other hand, full-endoscopic procedures rely more on fluoroscopy and expose both patients and surgeons to more radiation [11]. Another disadvantage of full-endoscopic procedures is the learning curve. The learning curve is often seen as a barrier by surgeons for offering full-endoscopic spine surgery [12-14]. Especially more so for percutaneous transforaminal endoscopic discectomy (PTED) which may be more difficult to perform compared to its interlaminar variant, because of the transforaminal route that most surgeons are unfamiliar with [15].
Recently, the results of a randomized controlled trial (RCT) were published in which noninferiority of PTED in leg pain reduction was shown compared to microdiscectomy [1,2]. In addition, PTED resulted in more favorable outcomes regarding functionality, quality of life, recovery, and opioid utilization. Furthermore, mainly due to less societal costs, PTED showed dominance in cost-effectiveness over microdiscectomy [1]. These study results are an important foundation for the implementation of PTED for sciatica.
As PTED warrants implementation, studies assessing the surgical learning curve are needed. Most studies assessing the learning curve are focused on duration of surgery or patient-reported outcomes such as leg pain [8-10,12-14,16]. Up to now, no studies have been conducted that evaluated the learning curve process from start systematically. In the set-up of the current study, 3 surgeons naive to PTED, were trained in PTED by a senior surgeon. Their learning process has been extensively measured using questionnaires. In the current manuscript, the results of this learning process are presented.
A multicenter, noninferiority, RCT was conducted at 4 general hospitals in The Netherlands among patients with sciatica caused by lumbar disc herniation. Details of the protocol and study design have been published previously [17]. The study was funded by ZonMw, The Netherlands Organization for Health Research and Development. The trial was initiated and performed without involvements of the industry. The research protocol was approved by the research ethics board of all participating hospitals. All patients provided written informed consent prior to enrollment. The trial was registered at ClinicalTrials.gov (NCT02602093).
From February 2016 to April 2019 patients were screened and enrolled by spine surgeons. Patients were eligible for the PTED-study if they were between 18 to 70 years of age; had more than 6 weeks of excessive radiating pain and no tendency for any clinical improvement; had an indication for surgery; had magnetic resonance imaging demonstrating a disc herniation with nerve compression with or without concomitant spinal or lateral recess stenosis or sequestration, and; had sufficient knowledge of the Dutch language in order to complete forms and follow instructions independently. Exclusion criteria were previous surgery on the same or adjacent disc level; cauda equina syndrome; spondylolytic or degenerative spondylolisthesis; pregnancy; severe comorbid medical or psychiatric disorder (American Society of Anesthesiologists physical status classification > II); severe caudal or cranial sequestration of disc fragments; contraindication for surgery and moving abroad on short notice [17].
Patients were randomized in a 1:1 ratio to PTED or microdiscectomy using computer-generated variable block sizes (4, 6, or 8), stratified by enrolling center. Blinding of patients was not feasible because of the substantial differences between both procedures (e.g., PTED having an 8-mm incision lateral of the spine and microdiscectomy having an incision of 2ŌĆō5 cm dorsal of the spine in the midline).
All trial surgeons were spine-dedicated surgeons who had 8 to 11 years of experience in performing degenerative lumbar surgery. Before the trial, only one of the participating neurosurgeons was proficient in performing PTED in The Netherlands [18]. During this study, 3 surgeons (one per center) were trained in performing PTED, alongside the senior surgeon in the fourth hospital. Each surgeon attended a hands-on cadaveric workshop on PTED. This workshop existed of presentations on indications, outcomes, and pearls and pitfalls of PTED. After these presentations, the surgeons could practice PTED multiple times on a cadaver. After this workshop they performed 10 to 20 procedures under the supervision of the senior surgeon. Afterwards, they would perform PTED independently. Based on an educated guess, we assumed that the learning curve would take 50 cases per surgeon.
The full procedure has been published previously [15]. Local anesthesia was administered [19]. After insertion of a guidewire in the neuroforamen, conical rods are introduced followed by a drill to enlarge the neuroforamen. Hereafter, an endoscope was introduced within the working channel using an 8-mm cannula. A forceps was used to remove the disc fragments. Patients were treated on an outpatient basis. All surgeons used the same instruments (MaxMoreSpine, Unterf├Čhring, Germany).
A complete overview of the patient-reported outcome measures (PROMs) measured during the PTED-study, along with the statistical analysis plan, has been published elsewhere [2,17]. In brief, the PTED-study was a RCT which established the noninferiority of PTED in leg pain reduction compared to microdiscectomy. The sample size was set at 682 patients and included 150 learning curve cases which were matched with 150 microdiscectomy cases. The PTED learning curve cases were excluded for the primary analysis.
The following instruments were used during the study:
ŌĆó The objective structured assessment of technical skills (OSATS) [20]
The OSATS is often used by attending physicians to score technical skills of residents. The OSATS scores 8 different domains and an overall score on technical scales on a scale ranging from 4 to 10 (highest skills). These domains are; indication for surgery; respect for tissue; time and motion; knowledge & handling of instruments; use of assistants; flow of operation; knowledge of specific procedure; and perioperative management. The OSATS was assessed by both the learning curve surgeons themselves, and the senior surgeon.
ŌĆó A 10-item checklist with 10 essential steps of PTED was created (Supplementary material 1)
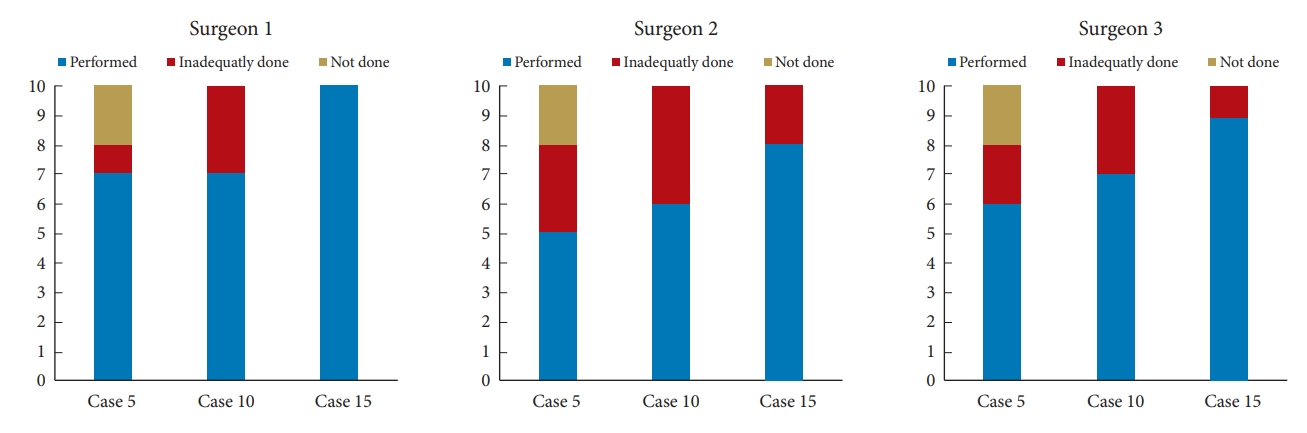
After each 5 cases, the senior surgeon would score if the learning curve surgeons would have performed all of these 10 steps, and whether it was performed adequately.
ŌĆó The global operative assessment of laparoscopic skills (GOALS) [21]
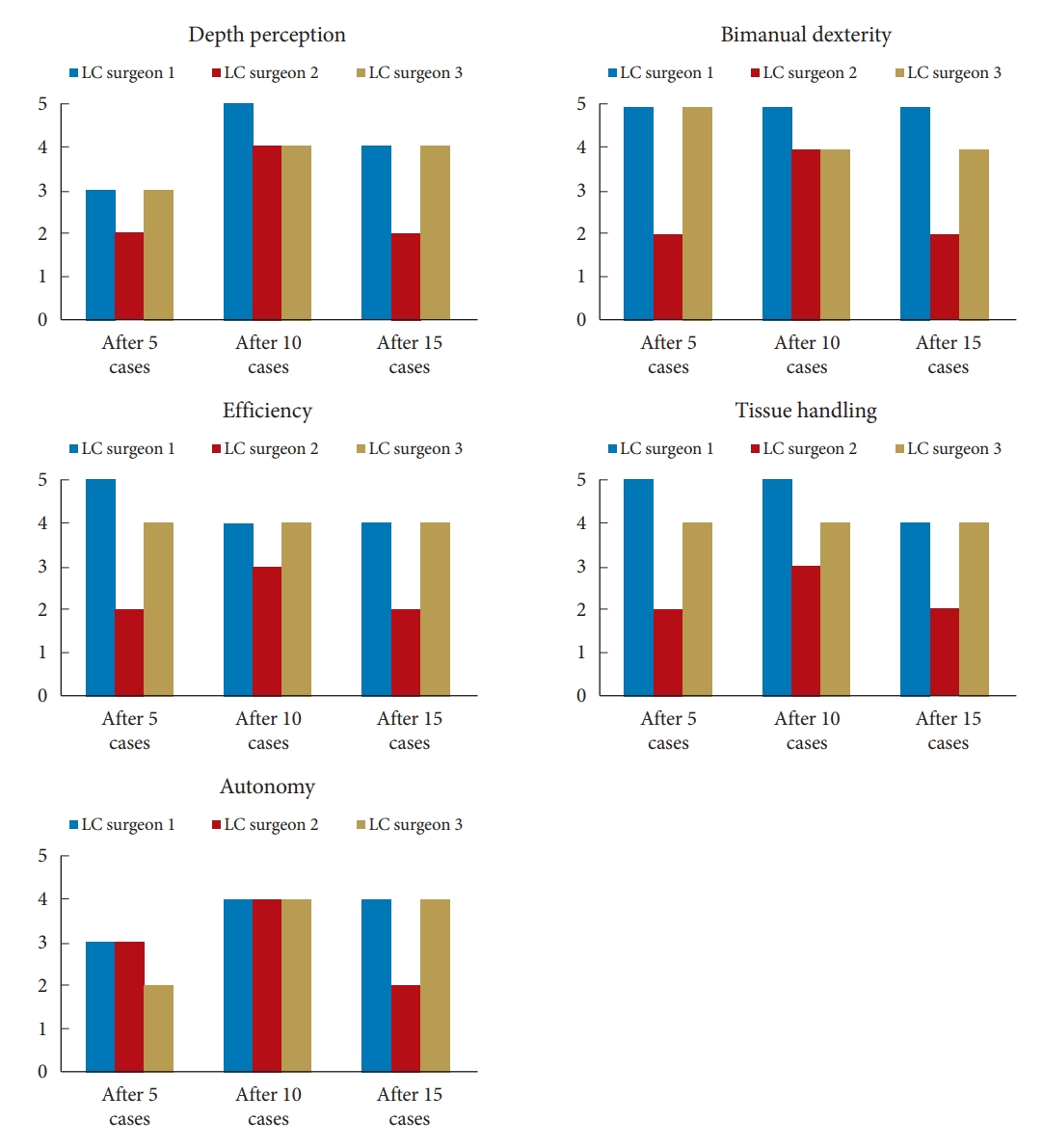
This questionnaire was specifically validated to grade overall technological proficiency for laparoscopic skills. As it was estimated that its domains would also be applicable to endoscopic surgery (i.e., depth-perception, bimanual dexterity, efficiency, tissue handling, and autonomy), it was also used in the current study. The GOALS were scored by the senior surgeon on a 1 to 5 Likert scale.
Measurements were conducted before the cadaveric workshop and were then repeated after each 5 cases up to case 20. At baseline, demographics, and expectations of the learning curve, were collected. Then, after each 5 cases up to case 20, the OSATS, 10-item checklist and GOALS were collected. All analyses were conducted with IBM SPSS Statistics ver. 27.0 (IBM Co., Armonk, NY, USA).
From February 2016 to April 2019, 613 patients were randomized between microdiscectomy and PTED (Fig. 1). Of the 304 cases assigned to PTED, 161 were assigned to the 3 learning curve surgeons. Learning curve surgeons had tenures ranging from 8 to 11 years (Table 1). At baseline, the learning curve surgeons expected to have a learning curve of 20 to 25 cases. On a 0 to 10 scale, learning curve surgeons scored the (1) difficulty of PTED a 7.8, (2) need for theoretical training a 6.6; and (3) the need for practical training a 9.5.
Fig. 2 gives an overview of the scores on the OSATS after each 5 cases up to case 20, as scored by the learning curve surgeons themselves. All 8 domains and the overall scores showed improvements between the first 5 and last 5 cases (Table 2). Biggest improvements between the first 5 cases and the last 5 cases, were seen in the domains ŌĆśtime and motionŌĆÖ by 2.0 points, ŌĆśrespect for tissueŌĆÖ by 1.7 points, and ŌĆśknowledge and handling of instrumentsŌĆÖ by 1.7 points. Scores of the senior surgeon were less sensitive to detect the change in the OSATS domains. Differences in OSATS scores as assessed by the learning curve surgeons versus the senior surgeon, ranged from 0 to 1.3.
The results of the 10-item specific checklist are shown in Fig. 3. By the fifth case, all 3 learning curve surgeons did not perform 2 steps of the PTED procedure, while 1 to 3 steps were performed inadequately. By case 10, all 3 learning curve surgeons performed all tasks but all 3 performed 3 to 4 cases inadequately. In case 15, one surgeon performed all 10 steps adequately. Of the remaining 2 surgeons, one performed 1 task inadequate and the other 2 tasks.
Fig. 4 gives an overview of the results on the GOALS. In general, the GOALS did not detect big differences between the cases. The biggest improvements in scores were found in the domains ŌĆ£depth-perceptionŌĆØ and ŌĆ£autonomy.ŌĆØ All other 3 domains showed comparable results, mainly for surgeons 1 and 3.
The current study presents the prospective results of the learning process of 3 surgeons, who had never performed PTED before. Other studies prospectively evaluating the learning curve process are lacking.
In total, the 3 learning curve surgeons performed a total of 161 cases. Based on self-assessment, surgeons improved mostly in the domains ŌĆ£time and motion,ŌĆØ ŌĆ£respect for tissue,ŌĆØ and ŌĆ£knowledge and handling of instruments.ŌĆØ Learning curve surgeons were more able to detect differences in performances on the OSATS than the senior surgeon. Based on the GOALS, the biggest improvements could be seen in ŌĆ£depth-perceptionŌĆØ and ŌĆ£autonomy.ŌĆØ Based on the 10-item specific checklist, all surgeons performed all 10 steps by case 10, while only one surgeon performed all steps adequately by case 15.
A remarkable finding of this study is that self-assessment of the learning curve surgeons was more responsive to change compared to OSATS scores given by the senior surgeon. An explanation for this might be that the senior surgeon scored multiple surgeons in a long-time span and more scored around the mean, while the learning curve surgeons themselves were only involved with their own learning process and therefore more adequately noticed improvements on various domains.
Another unexpected finding was that according to the GOALS, only surgeon 2 showed a decrease in scores between the 10th and the 15th case. An explanation for this is that during the trial enrollment, the operating room at the hospital of surgeon 2 was closed temporarily which has also resulted in a lower recruitment. Therefore, surgeon 2 performed 32 cases at the same time span other surgeons performed 43 to 147 cases. Perhaps, the closure of the operating room might have resulted in a temporary set-back in the learning process.
Some limitations have to be acknowledged. First is the absence of a valid instrument to assess the learning curve process. During this study, the OSATS and the GOALS were used [20,21]. Both of these questionnaires had other goals than they were used for the current study. The OSATS was intended to be an instrument to objectively measure technical skills of surgical residents, while the GOALS was intended specifically to measure laparoscopic skills while performing a cholecystectomy in novice trainees. The latter may also explain why the GOALS failed to measure change in skills for cases as all 3 learning curve surgeons already had some experience holding an endoscope due to performing endoscopic pituitary surgery or arthroscopy. Therefore, the GOALS might have been less sensitive to detect improvements of endoscopic skills in this study population. The 10-item specific checklist did prove to be useful during the training process, as it showed step-by-step mastering of the procedure. However, after 15 cases, it could not detect further improvements in surgical skills. Another limitation is the slow enrollment rate for some centers. For instance, learning curve surgeon 2 performed 32 cases while surgeon 1 performed 86 cases during the same time. This slow enrollment rate might also had consequences for the learning curve of the surgeons as they would perform only one PTED case per month. Strengths of this study include the prospective nature, the inclusion of multiple surgeons with different training backgrounds, and the systematic assessment of the learning process.
Based on these study results, PTED appears to be successfully adopted stepwise by 3 spine-dedicated surgeons. From 15 cases on, most steps of PTED have performed adequately. Validated tools, however, are needed to determine the cutoff when a surgeon should be able to perform PTED on his own.
SUPPLEMENTARY MATERIALS
It can be found via https://doi.org/10.14245/ns.2244334.167. Supplementary material 1. 10-item specific checklist.
NOTES
Fig.┬Ā1.
Flowchart with an overview of the enrollment and follow-up during the PTED-study. PTED, percutaneous transforaminal endoscopic discectomy; OM, open microdiscectomy.
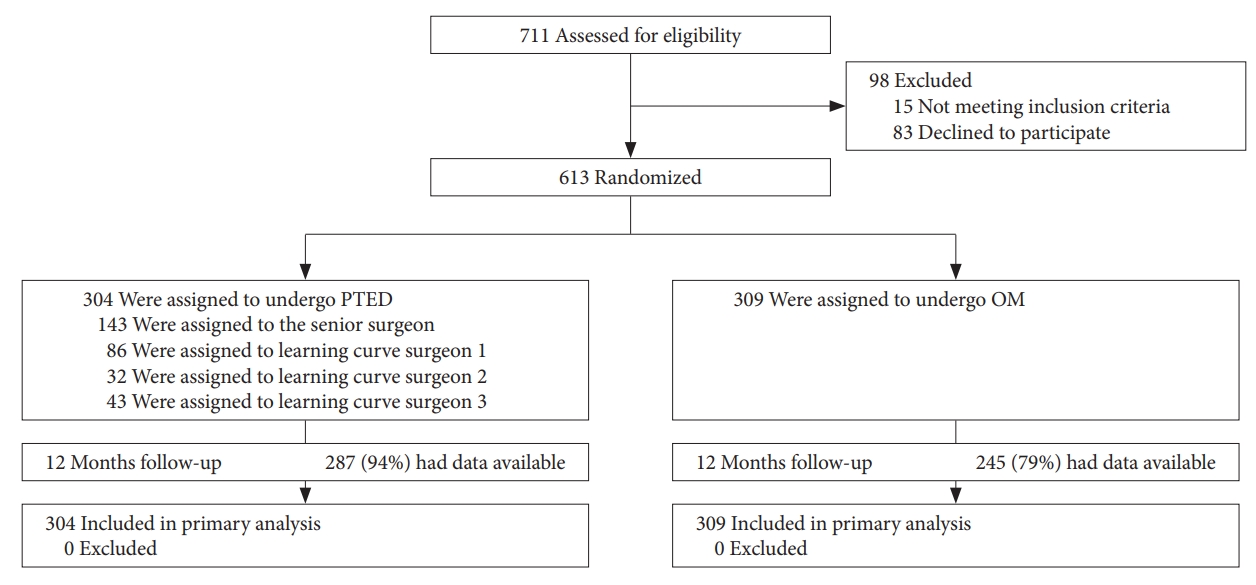
Fig.┬Ā2.
Scores on the objective structured assessment of technical skills on performing percutaneous transforaminal endoscopic discectomy for the different surgeons as scored by themselves and by the experienced surgeon, are shown. LC, learning curve.

Fig.┬Ā4.
Global operative assessment of laparo-/endoscopic skills of the trainee surgeons, as scored by the experienced surgeon. LC, learning curve.
Table┬Ā1.
Demographics of the 3 spine surgeons naive to PTED and the senior surgeon proficient in PTED
Table┬Ā2.
Mean scores of the learning curve surgeons on the OSATS on the first and last assessed cases, divided between self-assessment versus proficient surgeon scoring
REFERENCES
1. Gadjradj PS, Broulikova HM, van Dongen JM, et al. Cost-effectiveness of full endoscopic versus open discectomy for sciatica. Br J Sports Med 2022;56:1018-25.



2. Gadjradj PS, Rubinstein SM, Peul WC, et al. Full endoscopic versus open discectomy for sciatica: randomised controlled non-inferiority trial. BMJ 2022;376:e065846.



3. Gadjradj PS, Arts MP, van Tulder MW, et al. Management of symptomatic lumbar disk herniation: an international perspective. Spine (Phila Pa 1976) 2017;42:1826-34.

4. Gadjradj PS, Harhangi BS, Amelink J, et al. Percutaneous transforaminal endoscopic discectomy versus open microdiscectomy for lumbar disc herniation: a systematic review and meta-analysis. Spine (Phila Pa 1976) 2021;46:538-49.

5. Wu PH, Kim HS, Jang IT. A narrative review of development of full-endoscopic lumbar spine surgery. Neurospine 2020;17(Suppl 1):S20-33.




6. Ren Z, He S, Li J, et al. Comparison of the safety and effectiveness of percutaneous endoscopic lumbar discectomy for treating lumbar disc herniation under epidural anesthesia and general anesthesia. Neurospine 2020;17:254-9.




7. Chung AS, Wang JC. The rationale for endoscopic spinal surgery. Neurospine 2020;17(Suppl 1):S9-12.




8. Gadjradj PS, PTED-study group. Infographic. Endoscopic versus open discectomy for sciatica? Which is more cost-effective? Br J Sports Med 2022 May 18:bjsports-2022-105766https://doi.org/10.1136/bjsports-2022-105766. [Epub].


9. Gadjradj PS, Depauw PR, Schutte PJ, et al. Body image and cosmesis after percutaneous transforaminal endoscopic discectomy versus conventional open microdiscectomy for sciatica. Global Spine J 2022 May 24:21925682221105271https://doi.org/10.1177/21925682221105271. [Epub].

10. Gadjradj PS. Full-endoscopic lumbar disc surgery: the new gold standard? (PhD Academy Award). Br J Sports Med 2022 May 19:bjsports-2022-105434https://doi.org/10.1136/bjsports-2022-105434. [Epub].


11. Ahn Y, Kim CH, Lee JH, et al. Radiation exposure to the surgeon during percutaneous endoscopic lumbar discectomy: a prospective study. Spine (Phila Pa 1976) 2013;38:617-25.

12. Ahn Y, Lee S, Son S, et al. Learning curve for interlaminar endoscopic lumbar discectomy: a systematic review. World Neurosurg 2021;150:93-100.


13. Sun B, Shi C, Xu Z, et al. Learning curve for percutaneous endoscopic lumbar diskectomy in bi-needle technique using cumulative summation test for learning curve. World Neurosurg 2019;129:e586-93.


14. Hsu HT, Chang SJ, Yang SS, et al. Learning curve of full-endoscopic lumbar discectomy. Eur Spine J 2013;22:727-33.




15. Gadjradj PS, Harhangi BS. Percutaneous transforaminal endoscopic discectomy for lumbar disk herniation. Clin Spine Surg 2016;29:368-71.


16. Son S, Ahn Y, Lee SG, et al. Learning curve of percutaneous endoscopic transforaminal lumbar discectomy by a single surgeon. Medicine (Baltimore) 2021;100:e24346.



17. Seiger A, Gadjradj PS, Harhangi BS, et al. PTED study: design of a non-inferiority, randomised controlled trial to compare the effectiveness and cost-effectiveness of percutaneous transforaminal endoscopic discectomy (PTED) versus open microdiscectomy for patients with a symptomatic lumbar disc herniation. BMJ Open 2017;7:e018230.



18. Gadjradj PS, van Tulder MW, Dirven CM, et al. Clinical outcomes after percutaneous transforaminal endoscopic discectomy for lumbar disc herniation: a prospective case series. Neurosurg Focus 2016;40:E3.

19. Gadjradj PS, Arjun Sharma JRJ, Harhangi BS. Quality of conscious sedation using dexmedetomidine during full-endoscopic transforaminal discectomy for sciatica: a prospective case series. Acta Neurochir (Wien) 2022;164:1209-16.




- TOOLS
- Related articles in NS
-
Uniportal, Transforaminal Endoscopic Thoracic Discectomy: Review and Technical Note2023 March;20(1)
Surgeons Learning Curve of Transforaminal Endoscopic Discectomy for Sciatica2022 September;19(3)
Thermographic Assessment of Transforaminal Endoscopic Lumbar Discectomy2005 September;2(3)