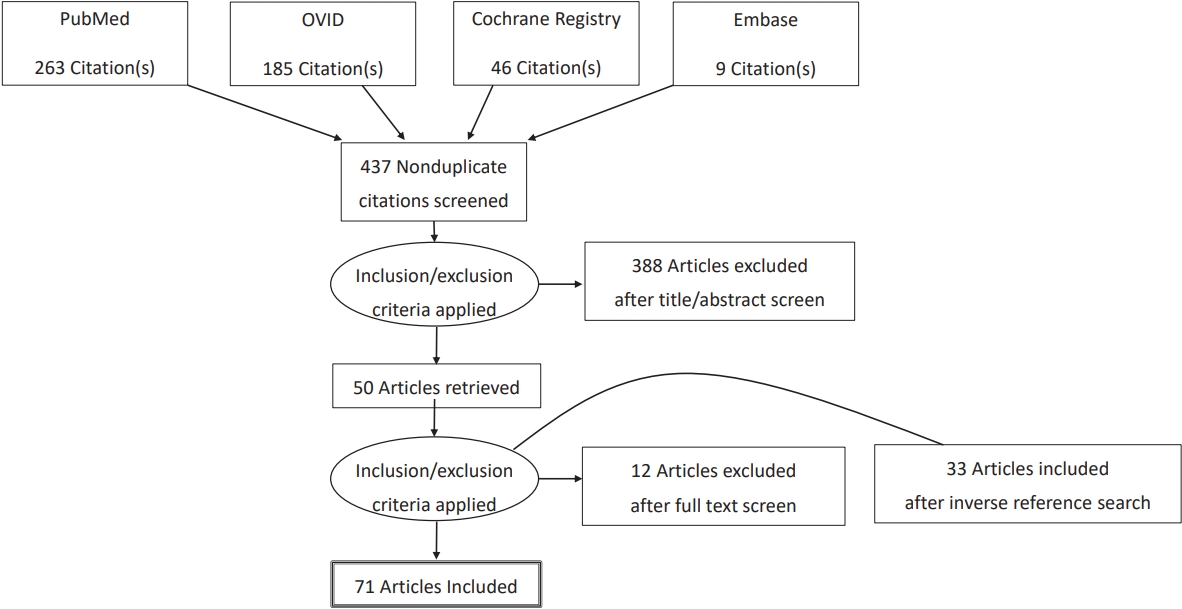
- Search
|
|
||
Abstract
Supplementary Materials
NOTES
ACKNOWLEDGEMENTS
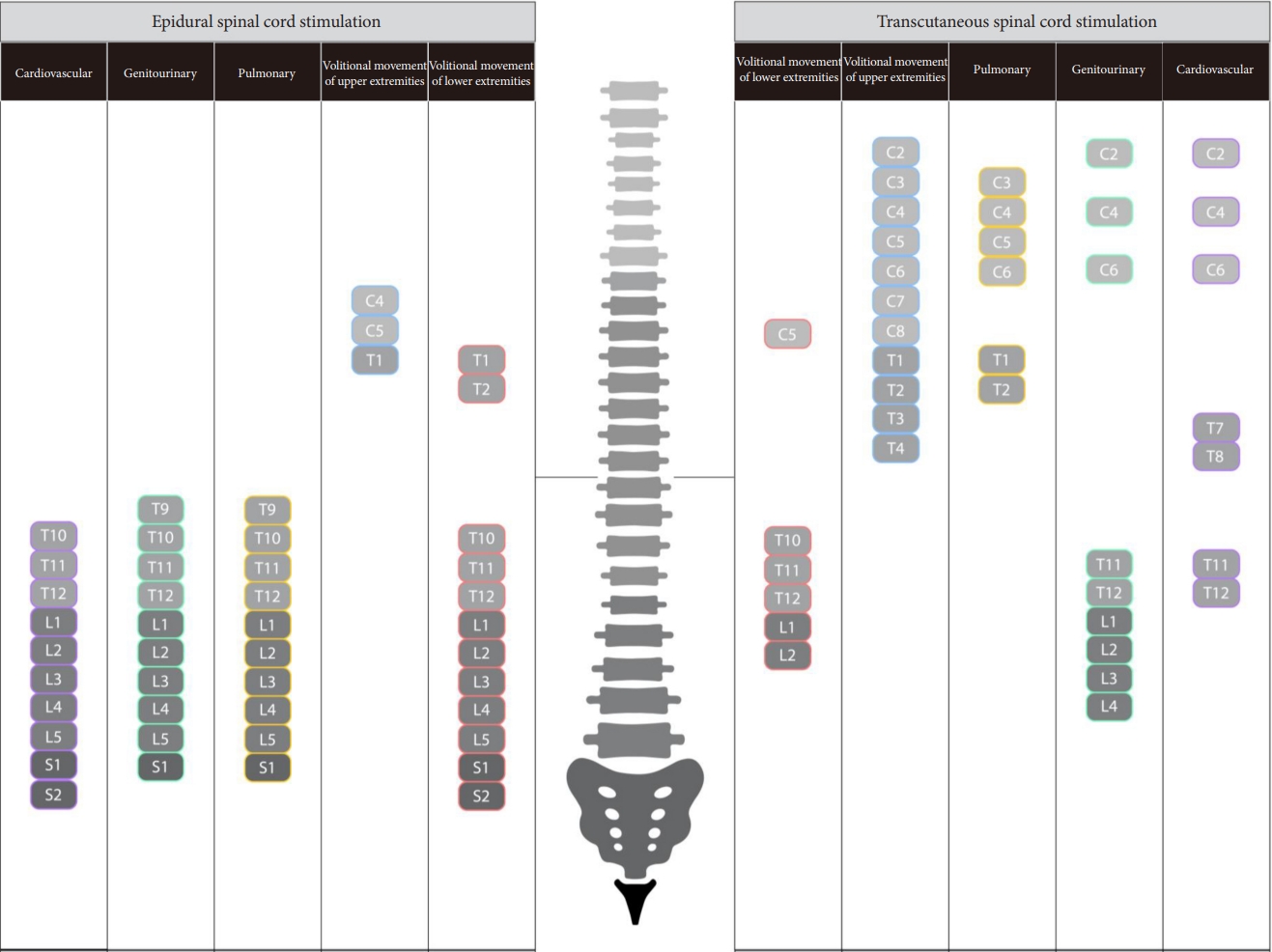
Fig.┬Ā3.
Table┬Ā1.
| Study | Design | Site | Subjects (n) | Sex | Age (yr), mean┬▒SD | Age (yr), range | Level of injury | AIS | Time (yr), mean ┬▒ SD | SCI length (yr), range |
|---|---|---|---|---|---|---|---|---|---|---|
| Barolat et al. [19] (1986) | Case report | Philadelphia, PA, USA | 1 | M | 22 | 22 | C5 | C | 0.75 | 0.75 |
| Katz et al. [20] (1991) | Case series | Richmond, VA, USA | 33 | 31M, 2F | - | 24ŌĆō66 | C4ŌĆōT10 | AŌĆōD | - | 0.6ŌĆō31.5 |
| Herman et al. [21] (2002) | Case report | Phoenix, AZ, USA | 1 | M | 43 | 43 | C6 | C | 3.5 | 3.5 |
| Carhart et al. [22] (2004) | Case report | Phoenix, AZ, USA | 1 | M | 43 | 43 | C5ŌĆōC6 | C | 3.5 | 3.5 |
| Jilge et al. [23] (2004) | Case series (retrospective) | Vienna, Austria | 5 | 2M, 3F | 27.6 ┬▒ 3.4 | 24ŌĆō34 | C4ŌĆōT10 | 4A, 1B | 4.8 ┬▒ 3.4 | 2ŌĆō8 |
| Minassian et al. [24] (2004) | Case series (retrospective) | Vienna, Austria | 10 | 7M, 3F | 26.9 ┬▒ 11.7 | 18ŌĆō58 | C4ŌĆōT10 | 8A, 2B | 2.7 ┬▒ 1.3 | 1ŌĆō5 |
| Ganley et al. [25] (2005) | Case series | Tempe, AZ, USA | 2 | 2M | 45.4 ┬▒ 2.5 | 43ŌĆō48 | C6ŌĆōT8 | C | 5.8 ┬▒ 2.3 | 3.5ŌĆō8.0 |
| DiMarco et al. [26] (2006) | Case report | Cleveland, OH, USA | 1 | M | 52 | 52 | C5ŌĆōC6 | C | 7 | 7 |
| Huang et al. [27] (2006) | Case series | Tempe/Phoenix, AZ, USA | 2 | 2M | 45.5 ┬▒ 3.5 | 43ŌĆō48 | C5ŌĆōT8 | C | 5.8 ┬▒ 3.2 | 3.5ŌĆō8 |
| DiMarco et al. [67,68] (2009) | Clinical trial | Cleveland, OH, USA | 9 | 8M, 1F | 41 ┬▒ 11.5 | 23ŌĆō52 | C3ŌĆōC6 | - | 13.1 ┬▒ 11.3 | 1ŌĆō34 |
| Harkema et al. (2011) [28] | Case report | Louisville, KY/Los Angeles, CA, USA | 1 | M | 23 | 23 | C7 | B | 3 | 3 |
| Moshonkina et al. [29] (2012) | Case series | St. Petersburg, Russia | 4 | 1M, 3F | 42 ┬▒ 15.7 | 22ŌĆō58 | C5ŌĆōL1 | 2A/B, 1B, 1B/C | - | - |
| Hofstoetter et al. [30] (2013) | Case report | Vienna, Austria | 1 | F | 29 | 29 | T9 | D | 11 | 11 |
| Angeli et al. [7] (2014) | Case series | Louisville, KY/Los Angeles, CA, USA | 4 | 4M | 26.9 ┬▒ 4 | 23ŌĆō32 | C6ŌĆōT6 | 2A, 2B | 3.0 ┬▒ 1 | 2.2ŌĆō4.2 |
| Hofstoetter et al. [31] (2014) | Case series | Vienna, Austria | 3 | 2M, 1F | 32.7 ┬▒ 4.1 | 28ŌĆō38 | C5ŌĆōT9 | D | 10.6 ┬▒ 1.5 | 9ŌĆō12 |
| Sayenko et al. [32] (2014) | Case series | Louisville, KY/Los Angeles, CA, USA | 3 | 3M | 26.3 ┬▒ 4.9 | 23ŌĆō32 | C7ŌĆōT4 | 1A, 2B | 3.3 ┬▒ 1.0 | 2.2ŌĆō4.2 |
| Bedi and Arumugam [33] (2015) | Case report | Punjab, India | 1 | M | 25 | 25 | L1 | C | 2.5 | 2.5 |
| Gerasimenko et al. [34] (2015) | Case series | St. Petersburg, Russia/Los Angeles, CA, USA | 5 | - | - | - | - | - | - | - |
| Hofstoetter et al. [35] (2015) | Case series | Vienna, Austria | 3 | 2M, 1F | 32.6 ┬▒ 5.0 | 28ŌĆō38 | C5ŌĆōT9 | D | 10.6 ┬▒ 1.5 | 9ŌĆō12 |
| Rejc et al. [36] (2015) | Case series | Louisville, KY/Los Angeles, CA, USA | 4 | 4M | 27 ┬▒ 4.2 | 24ŌĆō33 | C7ŌĆōT4 | 2A, 2B | 3.0 ┬▒ 1 | 2.2ŌĆō4.2 |
| Bedi and Arumugam [37] (2016) | Case report | Punjab, India | 1 | M | 25 | 25 | T12 | C | - | - |
| Lu et al. [38] (2016) | Case series | Los Angeles, CA, USA | 2 | 2M | 19┬▒1 | 18ŌĆō20 | C5ŌĆōC6 | B | 2.3 ┬▒ 0.4 | 2ŌĆō2.5 |
| Minassian et al. [39] (2016) | Case series | Vienna, Austria | 4 | 3M, 1F | 39.5 ┬▒ 17.1 | 26ŌĆō64 | C8ŌĆōT8 | A | 3.5 ┬▒ 1.7 | 1.7ŌĆō4.8 |
| Gad et al. [40] (2017) | Case report | Los Angeles, CA, USA | 1 | M | 40 | 40 | T9 | A | 4 | 4 |
| Grahn et al. [41] (2017) | Case report | Rochester, MN, USA | 1 | M | 26 | 26 | T6 | A | 3 | 3 |
| Rejc et al. [42] (2017) | Case report | Louisville, KY/Los Angeles, CA, USA | 1 | M | 32 | 32 | C7 | B | 4.2 | 4.2 |
| Rejc et al. [43] (2017) | Case series | Louisville, KY/Los Angeles, CA, USA | 4 | 4M | 27 ┬▒ 4.2 | 24ŌĆō33 | C7ŌĆōT4 | 2A, 2B | 3.0 ┬▒ 1 | 2.2ŌĆō4.2 |
| Angeli et al. [44] (2018) | Case series | Louisville, KY, USA | 4 | 3M, 1F | 25.8 ┬▒ 4.5 | 22ŌĆō32 | C5ŌĆōT4 | 2A, 2B | 3.1 ┬▒ 0.4 | 2.2ŌĆō3.3 |
| Aslan et al. [45] (2018) | Case series | Louisville, KY, USA | 7 | 7M | 26.7 ┬▒ 4.1 | - | C5ŌĆōT4 | 4A, 3B | 2.7 ┬▒ 0.5 | 2.0ŌĆō3.5 |
| DiMarco et al. [46] (2018) | Case report | Cleveland, OH, USA | 1 | M | 50 | 50 | C4 | - | 2 | 2 |
| Formento et al. [47] (2018) | Case series | Laussane, Switzerland | 3 | 3M | 36.7 ┬▒ 9.6 | 28ŌĆō47 | C4ŌĆōC7 | 2C, 1D | 5.3 ┬▒ 1.2 | 4ŌĆō6 |
| Freyvert et al. [69] (2018) | Clinical trial | Los Angeles, CA, USA | 6 | 4M, 2F | 19.1 ┬▒ 1.3 | 18ŌĆō21 | C2ŌĆōC6 | B | 2.3 ┬▒ 0.9 | 1.5ŌĆō3.8 |
| Gad et al. [70] (2018) | Clinical trial | Los Angeles, CA, USA | 6 | 5M, 1F | 40.2 ┬▒ 16.6 | 20ŌĆō62 | C4ŌĆōC8 | 2B, 4C | 10.0 ┬▒ 7.1 | 1.1ŌĆō21 |
| Gill et al. [48] (2018) | Case report | Rochester, MN, USA | 1 | M | 26 | 26 | T8 | A | 3 | 3 |
| Harkema et al. [71] (2018a) | Clinical trial | Louisville, KY, USA | 4 | 3M, 1F | 30.8 ┬▒ 4.1 | 24ŌĆō35 | C4 | 3A, 1B | 6.5 ┬▒ 1.6 | 3.8ŌĆō8 |
| Harkema et al. [72] (2018b) | Clinical trial | Louisville, KY, USA | 4 | 3M, 1F | 30.8 ┬▒ 4.1 | 24ŌĆō35 | C4 | 3A, 1B | 6.5 ┬▒ 1.6 | 3.8ŌĆō8 |
| Herrity et al. [49] (2018) | Case series | Louisville, KY, USA | 5 | 5M | - | - | C4ŌĆōC5, T4 | 3A, 2B | 5.9 ┬▒ 1.9 | - |
| Inanici et al. [73] (2018) | Clinical trial | Seattle, WA, USA | 1 | M | 62 | 62 | C3ŌĆōC4 | D | 2 | 2 |
| Niu et al. [74] (2018) | Clinical trial | Los Angeles, CA, USA | 5 | 5M | 31 ┬▒ 10.6 | 22ŌĆō43 | C5ŌĆōT4 | A-B | 8.8 ┬▒ 7.5 | 5ŌĆō13 |
| Phillips et al. [50] (2018) | Case series | Los Angeles, CA, USA | 5 | - | - | - | C5ŌĆōT2 | 3A, 2B | >3 | >3 |
| Powell et al. [51] (2018) | Case series | Louisville, KY, USA | 6 | 4M, 2F | 45.8 ┬▒ 14 | 26ŌĆō59 | C6ŌĆōL1 | 4C, 2D | 15.7 ┬▒ 13.4 | 4.6ŌĆō41.1 |
| Rath et al. [52] (2018) | Case series | Los Angeles, CA, USA | 8 | 7M, 1F | 29.4 ┬▒ 7.7 | 23ŌĆō47 | C4ŌĆōT9 | 6A, 2C | 7.3 ┬▒ 3.3 | 2ŌĆō13 |
| Wagner et al. [2] (2018) | Case series | Laussane, Switzerland | 3 | 3M | 36.7 ┬▒ 9.6 | 28ŌĆō47 | C4ŌĆōC8 | 2C, 1D | 5.3 ┬▒ 1.2 | 4ŌĆō6 |
| Walter et al. [53] (2018) | Case report | Vancouver, BC, Canada | 1 | M | 32 | 32 | C5 | B | 6 | 6 |
| West et al. [54] (2018) | Case report | Vancouver, BC, Canada | 1 | M | Early 30s | Early 30s | C5 | B | - | - |
| Calvert et al. [75] (2019) | Clinical trial | Rochester, MN, USA | 2 | 2M | 31.5 ┬▒ 7.8 | 26ŌĆō37 | T3ŌĆōT6 | A | 4.5 ┬▒ 2.1 | 3ŌĆō6 |
| Cheng et al. [55] (2019) | Case series | Pasadena, CA/Louisville, KY, USA | 2 | - | - | - | - | A | - | ŌĆō |
| Darrow et al. [76] (2019) | Clinical trial | Minneapolis, MN, USA | 2 | 2F | 50 ┬▒ 2.8 | 48ŌĆō52 | T4ŌĆōT8 | A | 7.5 ┬▒ 3.5 | 5ŌĆō10 |
| Knikou et al. [56] (2019) | Case series | New York, NY, USA | 10 | 7M, 3F | 36.3 ┬▒ 11.2 | 19ŌĆō51 | C6ŌĆōT12 | 2A, 2B, 1C, 5D | 8.8 ┬▒ 8.1 | 2ŌĆō28 |
| Nightingale et al. [57] (2019) | Case report | Vancouver, BC, Canada | 1 | M | 33 | 33 | C5 | B | 5 | 5 |
| Sayenko et al. [77] (2019) | Clinical trial | Los Angeles, CA, USA | 15 | 12M, 3F | 31.2 ┬▒ 8.7 | 23ŌĆō53 | C4ŌĆōT12 | 11A, 1B, 3C | 6.0 ┬▒ 3.2 | 2ŌĆō13 |
| Terson de Paleville et al. [58] (2019) | Case series | Louisville, KY, USA | 4 | 4M | 27.3 ┬▒ 3.7 | 22.7ŌĆō31.6 | C5ŌĆōT5 | 3A, 1B | 2.6 ┬▒ 0.3 | 2.3ŌĆō2.9 |
| Alam et al. [78] (2020) | Clinical trial | Hong Kong, China | 1 | F | 48 | 48 | C7 | - | 21 | 21 |
| DiMarco et al. [59] (2020) | Case series | Cleveland, OH, USA | 10 | 10M | 40.4 ┬▒ 12.1 | 27ŌĆō58 | C2ŌĆōT1 | - | 7.1 ┬▒ 10.7 | 3ŌĆō37 |
| Gad et al. [60] (2020) | Case report | Los Angeles, CA, USA | 1 | M | 39 | 39 | C5 | A | 9 | 9 |
| Gill et al. [79] (2020) | Clinical trial | Rochester, MN, USA | 2 | - | 31.5 ┬▒ 7.8 | 26ŌĆō37 | T3ŌĆōT6 | A | 4.5 ┬▒ 2.1 | 3ŌĆō6 |
| Gorgey et al. [80] (2020) | Clinical trial | Richmond, VA, USA | 1 | 1M | 26 | 26 | C7 | C | 2 | 2 |
| Pe├▒a Pino et al. [81] (2020) | Clinical trial | Minneapolis, MN, USA | 7 | 4M, 3F | 42 ┬▒ 11.4 | 30ŌĆō60 | T4ŌĆōT8 | 6A, 1B | 7.7 ┬▒ 4.8 | 3ŌĆō17 |
| Wiesener et al. [61] (2020) | Case series | Berlin, Germany | 2 | - | 49 ┬▒ 12.7 | 40ŌĆō58 | T5ŌĆōT6 | A | 23 ┬▒ 18.4 | 10ŌĆō36 |
| Wu et al. [82] (2020) | Clinical trial | Bronx, NY, USA | 9 | 7M, 2F | 45.9 ┬▒ 13.7 | 22ŌĆō64 | C2ŌĆōC8 | 1B, 4C, 4D | 10.8 ┬▒ 5.9 | 1ŌĆō17 |
| Beck et al. [62] (2021) | Case series | Rochester, MN, USA | 2 | 2M | 31.5 ┬▒ 5.5 | 26ŌĆō37 | T3ŌĆōT6 | A | 4.5 ┬▒ 1.5 | 3ŌĆō6 |
| Calvert et al. [63] (2021) | Case series | Los Angeles, CA/Rochester, MN, USA | 9 | 8M, 1F | 27.1 ┬▒ 4.1 | 22ŌĆō36 | C5ŌĆōT6 | 5A, 1B, 3C | 6.1 ┬▒ 3.1 | 2ŌĆō13 |
| DiMarco et al. [83] (2021) | Clinical trial | Cleveland, OH, USA | 5 | 5M | - | 30ŌĆō50 | C3ŌĆōT1 | A | - | 2ŌĆō4 |
| Estes et al. [84] (2021) | Clinical trial | Atlanta, GA, USA | 8 | 6M, 2F | 44.4 ┬▒ 15.7 | 18ŌĆō63 | C1ŌĆōC7 | 2C, 6D | 0.3 ┬▒ 0.1 | 0.1ŌĆō0.5 |
| Herrity et al. [85] (2021) | Clinical trial | Louisville, KY, USA | 10 | 8M, 2F | 27.9 ┬▒ 4.7 | 20ŌĆō51 | C3ŌĆōT4 | 6A, 4B | 4.4 ┬▒ 2.3 | 1ŌĆō15 |
| Ib├Ī├▒ez et al. [64] (2021) | Case series | Louisville, KY, USA | 5 | 5M | 31.9 ┬▒ 10.7 | 24ŌĆō52 | C4ŌĆōT4 | 3A, 2B | 7.8 ┬▒ 5.2 | 2.2ŌĆō16.6 |
| Inanici et al. [86] (2021) | Clinical trial | Seattle, WA, USA | 6 | 4M, 2F | 42 ┬▒ 14 | 28ŌĆō62 | C3ŌĆōC5 | 2B, 2C, 2D | 4.6 ┬▒ 3.8 | 1.5ŌĆō12 |
| Linde et al. [87] (2021) | Clinical trial | Rochester, MN, USA | 2 | 2M | 31.5 ┬▒ 5.5 | 26ŌĆō37 | T3ŌĆōT6 | A | 4.5 ┬▒ 1.5 | 3ŌĆō6 |
| Mesbah et al. [65] (2021) | Case series | Louisville, KY, USA | 20 | 15M, 5F | 31.0 ┬▒ 9.6 | 19.9ŌĆō60.6 | C3ŌĆōT4 | 14A, 6B | 6.3 ┬▒ 3.4 | 2.4ŌĆō16.6 |
| Squair et al. [66] (2021) | Case report | Calgary, Alberta, Canada | 1 | M | 38 | 38 | C5 | A | 1 | 1 |
| Smith et al. [88] (2022) | Clinical trial | Louisville, KY, USA | 11 | 8M, 3F | - | 21ŌĆō45 | C2ŌĆōT1 | 6A, 5B | 5.1 ┬▒ 2.2 | 2.4ŌĆō8.6 |
Table┬Ā2.
| Study | Intervention | Stimulator type | Lead placement | No. of electrodes/ lead | Stimulation parameters | Location | Stimulation frequency | Stimulation pulse width | Stimulation amplitude | Stimulation pattern | Stimulation optimization |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Barolat et al. [19] (1986) | eSCS | Clinical technology corporation | Percutaneous | 1 | Tonic stimulation | T1ŌĆōT2 | 75 Hz | 250 ╬╝s | - | - | - |
| Katz et al. [20] (1991) | eSCS | Medtronic | Paddle | 4 | Tonic stimulation | - | - | - | - | - | Parameters optimized for spasticity |
| Herman et al. [21] (2002) | eSCS+BWST therapy | Medtronic | Percutaneous | 4 | Tonic stimulation | Lumbar enlargement | - | - | - | - | A variety of electrical parameter sets were examined |
| Carhart et al. [22] (2004) | eSCS+PWBT therapy | Medtronic | Percutaneous | 4 | Tonic stimulation | T10ŌĆōT12 | 40ŌĆō60 Hz | 800 ╬╝s | Amplitude at midpoint between sensory and motor threshold values | Continuous, charge-balanced, monophasic pulse trains | - |
| Jilge et al. [23] (2004) | eSCS | Medtronic | Percutaneous | 4 | Tonic stimulation | T12ŌĆōL1 | 5ŌĆō60 Hz | 210ŌĆō450 ╬╝s | 1-10 V | Pulse trains | - |
| Minassian et al. [24] (2004) | eSCS | Medtronic | Percutaneous | 4 | Tonic stimulation | T10ŌĆōT12 | 2.2ŌĆō50 Hz | - | 1-10 V | Single pulse, paired pulsesŃĆēand pulse trains | - |
| Ganley et al. [25] (2005) | eSCS+ locomotor training | Percutaneous | 4 | Tonic stimulation | T10ŌĆōT12 | 20ŌĆō60 Hz | 800 ╬╝s | Amplitudes between sensory and motor thresholds in S1 and at motor threshold for S2 | - | Adjusted on an individual basis | |
| DiMarco et al. [26] (2006) | eSCS | NeuroControl | Percutaneous | 1 | Tonic stimulation | T9, T11, L1 | 53 Hz | 150 ╬╝s at T9, 200 ms at T11 and L1 | 40 V | Pulse train with stimulation trigger controlled by patient | - |
| Huang et al. [27] (2006) | eSCS+partial weight bearing treadmill therapy | Medtronic | Percutaneous | 4 | Tonic stimulation | T10ŌĆōL2 | 20ŌĆō40 Hz | 800 ╬╝s | 3-8.5 V | Pulse train | - |
| DiMarco et al. [67,68] (2009) | eSCS | - | Percutaneous | 1 | Tonic stimulation | T9, T11, L1 | 30ŌĆō40 Hz | 150ŌĆō200 ╬╝s | 30-40 V | Pulse train | - |
| Harkema et al. [28] (2011) | eSCS+stand training | Medtronic | Paddle | 16 | Tonic stimulation | L1ŌĆōS1 | Stimulation for standing caudal L5-S1 at 15 Hz’╝ø stimulation for manually facilitated stepping: 30-40 Hz | 210 or 450 ╬╝s | 7.5 V | Different stimulation protocols for different activities: both involve tonic stimulation. | - |
| Moshonkina et al. [29] (2012) | eSCS+ locomotor training | Cooner Wire Co. | Percutaneous | 2-4 | Tonic stimulation | L2ŌĆōL4, S2 | 1-12 Hz | - | - | Carried out 2 times for 30 min in addition to the routine pharmacotherapy | - |
| Angeli et al. [7] (2014) | eSCS+ locomotor training | Medtronic | Paddle | 16 | Tonic stimulation | L1ŌĆōS1 | 25-30 Hz | - | - | - | Stimulation parameters optimized to target primary motor pool activation areas. |
| Sayenko et al. [32] (2014) | eSCS | Medtronic | Paddle | 16 | Tonic stimulation | L1ŌĆōS2 | 2 Hz | 210 ╬╝s | 0.5-10 V | Spatially selective, rectangular, biphasic pulse waveform | All modified for individual patients |
| Rejcet al. [36] (2015) | eSCS+ locomotor training | Medtronic | Paddle | 16 | Tonic stimulation | L1ŌĆōS1 | 25-60 Hz | - | 1.0-9.0 V | - | Adjustments made to electrode configurations to activate specific motor neuron pools |
| Lu et al. [38] (2016) | eSCS | Boston Scientific | Paddle | 16 | Tonic stimulation | C4/C5ŌĆōT1 | 2-40 Hz | 210 ╬╝s | 0.1-10.0 mA | Biphasic stimulation | Optimized for greatest hand motor responses |
| Grahn et al. [41] (2017) | eSCS+ locomotor training | Medtronic | Paddle | 16 | Tonic stimulation | Lumbar enlargement | - | - | - | - | Active electrode configurations and stimulation parameters were adjusted to allow volitional control. |
| Rejcet al. [42] (2017) | eSCS+ locomotor training | Medtronic | Paddle | 16 | Tonic stimulation | L1ŌĆōS1 | Stimulation for standing: 40-60 Hz at T1ŌĆōT2, T3ŌĆōT8. Stimulation for stepping: 30ŌĆō55 Hz at T2ŌĆōT3, T5ŌĆōT6, T7ŌĆōT9. Stimulation for voluntary movement: 30ŌĆō65 Hz at T1ŌĆōT3. | - | Stimulation for standing: 0.6ŌĆō1.0 V at T1ŌĆōT2, T3ŌĆōT8. Stimulation for stepping: 0.7-3.5V at T2ŌĆōT3, T5ŌĆōT6, T7-T9. Stimulation for voluntary movement: 0.4ŌĆō2.2 V at T1ŌĆōT3. | - | Varied electrode configuration for left/right side and specific activities. |
| Rejcet al. [43] (2017) | eSCS+ locomotor training | Medtronic | Paddle | 16 | Tonic stimulation | L1ŌĆōS1 | Starting stimulation parameters of frequency 2 Hz | - | 0.1-5 V | - | Parameters modulated synergistically to find stimulation frequency that elicited continuous (non-rhythmic) EMG pattern. |
| Angeli et al. [44] (2018) | eSCS+ locomotor training | Medtronic | Paddle | 16 | Tonic stimulation | L1ŌĆōS1/S2 | 2 Hz | 450 ╬╝s | 0.1 V ramping incrementally | - | Stimulation configurations selected to promote standing or stepping. |
| Aslan et al. [45] (2018) | eSCS | Medtronic | Paddle | 16 | Tonic stimulation | T11ŌĆōL1 | - | - | - | - | In standing experiments, voltage, frequency, and configuration of the electrode array were unique to each participant and optimized for over-ground standing. |
| DiMarco et al. [46] (2018) | eSCS | - | Percutaneous | 2 | Tonic stimulation | T9, T11 | 50 Hz | 0.2 ms | 40 V | Pulse train with monopolar stimulation at T9 or bipolar stimulation at T9/T11 | |
| Formento et al. [47] (2018) | eSCS | Medtronic | Paddle | 16 | Tonic stimulation | Lumbosacral | 40 Hz | - | 3-9 mA | - | Spatially specific stimulation parameters optimized to target primary motor pool activation areas that were key in movement. |
| Gill et al. [48] (2018) | eSCS+ locomotor training | Medtronic | Paddle | 16 | Tonic stimulation | T11ŌĆōL1 | 15-40 Hz | 210 ╬╝s | - | BiphasicŃĆēcharge-balanced pulses | Parameters modified to enable voluntary control. |
| Harkema et al. [71] (2018) | eSCS | Medtronic | Paddle | 16 | Tonic stimulation | T11ŌĆōL1 | - | 450 ╬╝s | - | - | Configurations (anode and cathode electrode selection, voltage, frequency) were identified to maintain systolic blood pressure within the desired range, then adjusted as needed. |
| Harkema et al. [72] (2018) | eSCS | Medtronic | Paddle | 16 | Tonic stimulation | T11ŌĆōL1 | - | 450 ╬╝s | - | - | Configurations (anode and cathode electrode selection, voltage, frequency) were identified to maintain systolic blood pressure within the desired range, then adjusted as needed. |
| Herrity et al. [49] (2018) | eSCS+activity-based recovery training | Medtronic | Paddle | 16 | Tonic stimulation | L1ŌĆōS1 | 30 Hz | 450 ╬╝s | Voltage was ramped up slowly (0.1 V increments) | - | All stimulation at the lower end of the stimulator array optimized for a single patient, then carried over to other patients |
| Wagner et al. [2] (2018) | eSCS+ locomotor training+ gravity assist device | Medtronic | Paddle | 16 | Spatiotemporal modulation | T11ŌĆōL1 | 20-60 Hz | - | - | Trains of spatially selective stimulation with timing that coincided with intended movement | - |
| Walter et al. [53] (2018) | eSCS | Medtronic | Paddle | 16 | Tonic stimulation | T11ŌĆōL1 | - | - | - | Trains of spatially selective stimulation with timing for specific actions pre-programmed | Participant could adjust intensity of program manually as needed |
| West et al. [54] (2018) | eSCS | Medtronic | Paddle | 16 | Tonic stimulation | T11ŌĆōL1 | 35 Hz | 300 ╬╝s | 3.5 V | - | - |
| Calvert et al. [75] (2019) | eSCS+ locomotor training | Medtronic | Paddle | 16 | Tonic stimulation | T11ŌĆōL1 | 40 Hz | 210 ╬╝s | - | Trains of spatially selective stimulation with timing for specific actions | - |
| Cheng et al. [55] (2019) | eSCS+stand training | Medtronic | Paddle | 16 | Tonic stimulation | L1ŌĆōS1 | 25 Hz | 200 ╬╝s | Stimuli optimized with machine learning algorithm | ||
| Darrow et al. [76] (2019) | eSCS | Abbott | Paddle | 16 | Tonic stimulation | L1ŌĆōS2 | 16-400 Hz | 200-500 ms | 2-15 mA | - | Optimization for specific locations and activities depending on positionality |
| Nightingale et al. [57] (2019) | eSCS | Medtronic | Paddle | 16 | Tonic stimulation | T11ŌĆōL1 | Abdominal program: 40 Hz. Cardiovascular program: 35 Hz. | Abdominal program: 420 ms. Cardiovascular program: 300 ms. | Abdominal program: 3.5-6.0 V. Cardiovascular program: 3.5-6.0 V. | Spatially directed differences in stimulation configuration. | - |
| Terson de Paleville et al. [58] (2019) | eSCS+ locomotor training | Medtronic | Paddle | 16 | Tonic stimulation | L1ŌĆōS1 | Simulation for standing (10-40 Hz) vs stepping (25-45 Hz) | - | - | - | - |
| DiMarco et al. [59] (2020) | eSCS | - | Percutaneous | 2 | Tonic stimulation | T9ŌĆōT11 | 50 Hz | 0.2 ms | 40 V | - | |
| Gill et al. [79] (2020) | eSCS + body weight supported treadmill training | Medtronic | Paddle | 16 | Tonic stimulation | T11ŌĆōL1 | 20-30 Hz | 200-450 ╬╝s | 2.0-4.1 V | Activity-specific spatially directed stimulation | - |
| Gorgey et al. [80] (2020) | eSCS+ exoskeletal-assisted walking training | Medtronic | Paddle | 16 | Tonic stimulation | T12ŌĆōS2 | 40 Hz | - | 4-8 V | Spatially selective stimulus | Modified based on patient performance |
| Pe├▒a Pino et al. [81] (2020) | eSCS | Abbott | Paddle | 16 | Tonic stimulation | T12ŌĆōL1 | - | - | - | Activity-specific spatially directed stimulation based on patient selection of preprogrammed settings | - |
| Beck et al. [62] (2021) | eSCS+task-specific training | Medtronic | Paddle | 16 | Tonic stimulation | Lumbosacral | - | - | - | - | Parameters were adjusted to enhance motor performance for standing or stepping |
| Calvert et al. [63] (2021) | eSCS | Medtronic | Paddle | 16 | Tonic stimulation | T11ŌĆōL1 | - | - | - | - | Electrode configurations enabled specific motor activation. |
| DiMarco et al. [83] (2021) | eSCS | - | Percutaneous | 2 | Tonic stimulation | T9ŌĆōT11 | 50 Hz | - | 20-30V | - | - |
| Herrity et al. [85] (2021) | eSCS+activity-based recovery training | Medtronic | Paddle | 16 | - | L1ŌĆōS1 | - | - | - | - | - |
| Ib├Ī├▒ez et al. [64] (2021) | eSCS+activity-based recovery training | Medtronic | Paddle | 16 | Tonic stimulation | T11ŌĆōL1 | - | - | - | - | Parameters optimized based on individualized maps of motor pools activation |
| Linde et al. [87] (2021) | eSCS+ locomotor training | Medtronic | Paddle | 16 | Tonic stimulation | Lumbosacral | - | - | - | - | Stimulation parameters optimized for movement (determined by participants) |
| Mesbah et al. [65] (2021) | eSCS+ activity-based recovery training | Medtronic | Paddle | 16 | Tonic stimulation | T12ŌĆōL2 | 2 Hz or 30 Hz | 450 or 1,000 ╬╝s | - | Bipolar electrode stimulation using a single adjacent anode and cathode as well as wide field configurations | Further optimization for individual joint movement. |
| Squair et al. [66] (2021) | eSCS | Medtronic | Paddle | 16 | Tonic stimulation | T10ŌĆōT12 | - | - | - | - | Parameters optimized to recruit the lower thoracic spinal segments and increase blood pressure |
| Smith et al. [88] (2022) | eSCS+activity-based recovery training | Medtronic | Paddle | 16 | Tonic stimulation | Lumbosacral | - | - | - | - | Stimulation parameter optimized to activate specific motor neuron pools |
Table┬Ā3.
| Study | Intervention | Stimulator type | Stimulation parameters | Location | Stimulation frequency | Stimulation pulse width | Stimulation amplitude | Stimulation pattern | Stimulation optimization |
|---|---|---|---|---|---|---|---|---|---|
| Hofstoetter et al. [30] (2013) | tSCS + treadmill stepping | Schwa-Medico | Tonic stimulation | T11ŌĆōT12 | 30 Hz | 2-ms width (1 ms per phase) | 18 V | Charge-balanced, symmetric, biphasic rectangular pulses | - |
| Hofstoetter et al. [31] (2014) | tSCS | Schwa-Medico | Tonic stimulation | T11ŌĆōT12 | 50 Hz | 2 ms | Intensities producing paresthesias but no motor responses in lower limbs | Biphasic pulses for 30 min | - |
| Bed! et al. [33] (2015) | tSCS + locomotor training | - | Tonic stimulation | T10ŌĆōL1 | Stimulations with carrier frequency of 2.5 kHz modulated to ŌĆ£beatŌĆØ frequency of 20 Hz | - | Amplitude raised to elicit sensory stimulation | Carrier modulated to ŌĆ£beatŌĆØ frequency | - |
| Gerasimenko et al. [34] (2015) | tSCS | NeuroRecovery Technologies Inc. | Tonic stimulation | C5, T11, L1 | Carrier frequency of 10 kHz at 5-40 Hz | 0.5-1.0 ms | 30-200 mA | Biphasic rectangular bursts with carrier frequency administered at beat frequency with spatial specificity for different motor neuron pool activation | - |
| Hofstoetter et al. [35] (2015) | tSCS + treadmill stepping | Schwa-Medico | Tonic stimulation | T11ŌĆōT12 | 30 Hz | 1 ms | Target intensities defined as to produce paresthesias covering most of the lower limb dermatome yet subthreshold for leg muscle activation | Charge-balanced, symmetric, biphasic rectangular pulses | - |
| Bed! et al. [37] (2016) | tSCS | - | Tonic stimulation | T10ŌĆōL1 | Stimulations with carrier frequency of 2.5 kHz modulated to ŌĆ£beatŌĆØ frequency of 30-90 Hz | - | Raised to elicit sensory stimulation | Carrier modulated to ŌĆ£beatŌĆØ frequency | - |
| Minassian et al. [39] (2016) | tSCS + robotic-driven gait orthosis | Schwa-Medico | Tonic stimulation | T11ŌĆōT12 | 30 Hz stimulation | 1 ms | - | Rectangular, monophasic paired pulses (interstimulus interval 30 ms, 50 ms, 100 ms) or single pulses | - |
| Gad et al. [40] (2017) | tSCS + exoskeleton + buspirone | - | Tonic stimulation | T11ŌĆōT12, Co1 | 30 Hz at T11 and/or 5 Hz at Co1 | - | - | - | - |
| Freyvert et al. [69] (2018) | tSCS + buspirone | - | Tonic stimulation | C5 | 5-30 Hz | - | 20-100 mA | - | - |
| Gad et al. [70] (2018) | tSCS + functional task training | NeuroRecovery Technologies Inc. | Tonic stimulation | C3ŌĆōC4, C6ŌĆōC7 | 30 Hz with carrier frequency of 10 kHz | 1 ms | 70-210 mA | Carrier modulated to ŌĆ£beatŌĆØ frequency with biphasic waveform or monophasic waveform | - |
| Inanici et al. [73] (2018) | tSCS + PT | NeuroRecovery Technologies Inc. | Tonic stimulation | C3ŌĆōC4, C6ŌĆōC7 | Pulses at frequency of 30 Hz with carrier frequency of 10 kHz | 1 ms | 80-120 mA | Carrier frequency modulated to ŌĆ£beatŌĆØ frequency | - |
| Niu et al. [74] (2018) | tSCS | Mag Venture | Tonic stimulation | T11ŌĆōL3/L4 | 1 Hz or 30 Hz | 250 ╬╝s | - | Trains of biphasic single pulse, continuous stimulation for sessions of three periods of 4 min continuous stimulation with a 30s break in between | - |
| Phillips et al. [50] (2018) | tSCS | ValuTrode | Tonic stimulation | T7ŌĆōT8 | 30 Hz | 1 ms | 10-70 mA | Monophasic pulses for at least 1 min | - |
| Powell et al. [51] (2018) | tSCS | NeuroConn | Tonic stimulation | T10ŌĆōT11 | - | - | 2.5 mA | 5 pulses for 20 min with interstimulus interval of 5 sec | - |
| Rath et al. [52] (2018) | tSCS | ValuTrode | Tonic stimulation | T11ŌĆōT12, L1ŌĆōL2 | ŌĆ£BeatŌĆØ frequency of 30 Hz over T11 and 15 Hz during stimulation over L1, with each pulse filled with a carrier frequency of 10 kHz | 1 ms | 10-150 mA | Monophasic, rectangular pulses with carrier frequency modulated to ŌĆ£beatŌĆØ frequency | - |
| Knikou et al. [56] (2019) | tSCS | Digit imer | Tonic stimulation | T10ŌĆōL1/L2 | 0.2 Hz | 1 ms | Subthreshold and suprathreshold intensities | Monophasic stimuli for 16+ sessions of 60 min | - |
| Sayenko et al. [77] (2019) | tSCS + locomotor training | ValuTrode | Tonic stimulation | T11ŌĆōT12, L1ŌĆōL2 | 0.2ŌĆō30 Hz with each pulse filled by a carrier frequency of 10 kHz | 1 ms | Up to 150 mA | Monophasic pulses with each pulse filled by a carrier frequency | - |
| Alam et al. [78] (2020) | tSCS + locomotor training | Digit imer | Tonic stimulation | T11, L1 | 9.4 kHz burst signal delivered at 0.5ŌĆō30 Hz | 100 ╬╝s to 1 ms | Dependent on activity (90-120 mA) | Biphasic stimulation with burst duration at T11 and L1 | - |
| Gad et al. [60] (2020) | tSCS | SpineX | Tonic stimulation | C3-C4, C5-C6,T1-T2 | Carrier pulse (10 kHz) combined with a low frequency (30 Hz) burst pulse | 1 ms | - | High frequency biphasic carrier pulse combined with a low frequency burst pulse | - |
| Wiesener et al. [61] (2020) | tSCS + FES + swim training | RehaMove | Tonic stimulation | T11-T12 | 50 Hz | 1 ms | - | Biphasic pulses | - |
| Wu et al. [82] (2020) | tSCS | Digitimer | Tonic stimulation | T2-T4 (posteriorly), C4-C5 (anteriorly) | 0.2 Hz | - | - | Pulses delivered in pseudorandom order or in pairs with 40 ms interstimulus intervals | - |
| Calvert et al. [63] (2021) | tSCS | Digitimer | Tonic stimulation | T11-L2 | 0.2 and 2 Hz | 1 ms | 0-150 mA | Monophasic rectangular pulses | - |
| Estes et al. [84] (2021) | tSCS + locomotor training | Empi Continuum | Tonic stimulation | T11-T12 | 50-Hz pulse | - | Highest intensity tolerated by patients or upon reporting paresthesias | Biphasic pulse for 30 min | - |
| Inanici et al. [86] (2021) | tSCS + functional task training | NeuroRecovery Technologies Inc. | Tonic stimulation | C2+C4 or C4+C6, anterior iliac crests of pelvis | 30-Hz base with 10 kHz overlapping frequency | 1 ms | 0-120 mA | Carrier modulated to ŌĆ£beatŌĆØ frequency | - |
Table┬Ā4.
| Study | Intervention | Type of outcome studied | Measured outcome | Complications |
|---|---|---|---|---|
| Barolat et al. [19] (1986) | eSCS | Volitional: EMG, spasticity | Complete abolition of the spasms, voluntary contraction and relaxation of left quadriceps with eSCS, augmentatory effect on deep tendon reflexes in the lower extremities | None noted |
| Katz et al. [20] (1991) | eSCS | GU: EMG, bladder volume, peak urinary flow | Postoperative changes in the lower urinary tract function were noted in 6 patients. Urodynamic parameters did not change significantly following implantation in the remaining 17 patients. | - |
| Herman et al. [21] (2002) | eSCS + BWST therapy | Volitional: gait analysis, whole body metabolic rate, BWS, TSW, OGW, HCA, IWS, sense of effort, spasticity | Immediate improvement in the subject's gait rhythm. After months of training, performance in speed, endurance, and metabolic responses gradually converged with/without eSCS at short distances. Performance with eSCS was superior at long distances. | None noted |
| Carhart et al. [22] (2004) | eSCS + PWBT therapy | Volitional: EMG, gait analysis, BWS, TSW, IWS, Borg scale for sense of effort | Reduction in sense of effort for over ground walking from 8/10 to 3/10 (Borg scale) and doubled walking speed | Discomfort at 100Hz stimulation |
| Jilge et al. [23] (2004) | eSCS | Volitional (changes in muscle activity): EMG, induced movement | Enabled initiation and retention of lower-limb extension, elicited posterior root muscle-reflex responses | None noted |
| Minassian et al. [24] (2004) | eSCS | Volitional (changes in muscle activity): EMG, induced movement | Recruitment of lower-limb muscles in segmental-selective way, characteristic of posterior root stimulation; stimulation at 5-15 and 25-50 Hz elicited sustained tonic and rhythmic activity respectively. | None noted |
| Ganley et al. [25] (2005) | eSCS + locomotor training | Volitional: EMG, gait analysis, BWS, TSW, OGW, HCA, IWS, sense of effort | Both patients were able to walk faster and further with stimulation than without stimulation. | None noted |
| DiMarco et al. [26] (2006) | eSCS | Pulmonary: airway pressure, air flow rate, volume of respiratory secretions | Combined T9+L1 stimulation increased airway pressure and expiratory flow rate to 132 cm H2O and 7.4 L/s respectively | None noted |
| Huang et al. [27] (2006) | eSCS + partial weight bearing treadmill therapy | Volitional: EMG, gait analysis, BWS, TSW, OGW, IWS, Borg scale for sense of effort | Acute modulations in muscle activities of both patients with stimulation but differences in observed pattern, magnitude, and spectral content of EMGs. | None noted |
| DiMarco et al. [67,68] (2009) | eSCS | Pulmonary: airway pressure, air flow rate, volume of respiratory secretions | During stimulation, mean maximum airway pressure generation and peak airflow rates 137 ┬▒ 30 cm H2O and 8.6┬▒1.8L/s respectively. | One nonfunctional lead in each subject, skin breakdown and infection near receiver in one subject, mild leg jerks during SCS (well tolerated), temporary asymptomatic autonomic dysreflexia in three subjects which abated completely with continued SCS |
| Harkema et al. [28] (2011) | eSCS + stand training | Volitional and GU: EMG, gait analysis, BWS, A/1 stand, A/1 step, proprioception, bladder storage and voiding | Recovery of supraspinal control of some leg movements only during epidural stimulation 7 months after implantation. | None noted |
| Moshonkina et al. [29] (2012) | eSCS + locomotor training | Volitional: EMG, BWS, IWS | Thresholds of muscle responses were significantly lower with bipolar stimulation than the thresholds determined with monopolar stimulation of a single segment. | None noted |
| Angeli et al. [7] (2014) | eSCS + locomotor training | Volitional: EMG, gait analysis, BWS, TSW, ASIA score | Achieved recovery of intentional movement of legs during epidural stimulation | None noted |
| Sayenko et al. [32] (2014) | eSCS | Volitional: EMG, BWS | Selective topographical recruitment of proximal and distal leg muscles during rostral and caudal stimulation of lumbar spinal cord | None noted |
| Rejc et al. [36] (2015) | eSCS + locomotor training | Volitional: EMG, BWS, A/l stand | Achieved full weight-bearing standing with continuous EMG patterns in lower limbs during stimulation | Discomfort (abdominal contractions) caused by stimulation |
| Lu et al. [38] (2016) | eSCS | Volitional: EMG, handgrip force | Improved hand strength (approximately three-fold) and volitional hand control with stimulation | None noted |
| Grahn et al. [41] (2017) | eSCS + locomotor training | Volitional: EMG, A/I stand | eSCS with activity-specific training enabled (1) volitional control of task-specific muscle activity, (2) volitional control of rhythmic muscle activity to produce steplike movements while side-lying, and (3) independent standing. | None noted |
| Rejc et al. [42] (2017a) | eSCS + locomotor training | Volitional: EMG, gait analysis, BWS, A/I stand, STS | Progressive recovery of voluntary leg movement and standing without stimulation, re-emergence of muscle activation patterns sufficient for standing | None noted |
| Rejc et al. [43] (2017b) | eSCS + locomotor training | Volitional: EMG, gait analysis, BWS, A/I stand, STS | Improved standing (4/4) and stepping (3/4) ability with stimulation and stand/step training. | None noted |
| Angeli et al. [44] (2018) | eSCS + locomotor training | Volitional: EMG, gait analysis, I. sit, BWS, A/I stand, TSW, OGW, IWS, proprioception | All (4/4) achieved independent standing and trunk stability with stimulation after 287 sessions, some (2/4) achievement of over ground walking with stimulation | One hip fracture during training, one mild drainage from surgery site, one ankle edema |
| Aslan et al. [45] (2018) | eSCS | Cardiovascular: EMG, plethysmography’╝ī BP, BP regulation during ortho stasis, HR | In three patients with arterial hypotension, eSCS applied while supine and standing maintained blood pressure at 119/72┬▒7/14 mmHg compared to 70/45┬▒5/7 mmHg without eSCS. | None noted |
| DiMarco et al. [46] (2018) | eSCS | Pulmonary: airway pressure, air flow rate, volume of respiratory secretions | Paw increased from 20 cm H2O (8.6% predicted) during spontaneous efforts to 84 cm H2O at FRC and 103 cm H2O at TLC during bipolar (T9ŌĆōT11) SCS and 61 cm H2O at FRC and 86 cm H2O at TLC with monopolar (T9) SCS. | Temporary development of asymptomatic autonomic dysreflexia resolving after 5-6 weeks |
| Formento et al. [47] (2018) | eSCS | Volitional: EMG, gait analysis, proprioception | Continuous eSCS prevented 2/3 participants from detecting leg movements. | None noted |
| Gill et al. [48] (2018) | eSCS + locomotor training | Volitional: EMG, gait analysis, BWS, A/I stand, TSW, A/I step, OGW, HCA, IWS, spasticity | Achieved independent bilateral stepping with stimulation | None noted |
| Harkema et al. [71] (2018) | eSCS | Cardiovascular: EMG, BP, BP during orthostasis, HR, plethysmography | Persistent hypotension was resolved in four individuals. | None noted |
| Harkema et al. [72] (2018) | eSCS | Cardiovascular: EMG, BP, BP during orthostasis, HR, plethysmography | Orthostatic hypotension was alleviated in 4 individuals. Improved cardiovascular response was observed after daily eSCS without stimulation. | None noted |
| Herrity et al. [49] (2018) | eSCS + activity-based recovery training | GU: EMG, storage and voiding, urodynamic parameters via cystometry | All 5 patients showed improvements in bladder emptying. | None noted |
| Wagner et al. [2] (2018) | eSCS + locomotor training + gravity assist device | Volitional: EMG, gait analysis, EEG, BWS, STS, A/l step, OGW, HCA, IWS, cycling, proprioception, ASIA score | Re-established adaptive control of paralyzed muscles during overground walking stimulation within one week, regained voluntary control over paralyzed muscles without stimulation, regained walking and cycling ability | None noted |
| Walter et al. [53] (2018) | eSCS | GU: EMG, EKG, external anal sphincter pelvic floor muscle tone and detrusor pressure, Neurogenic Bowel Dysfunction Score, orgasm | Reduced time needed for bowel management, modulated detrusor pressure and external anal sphincter/pelvic floor muscle tone | None noted |
| West et al. [54] (2018) | eSCS | Cardiovascular: EMG, plethysmography’╝ī BP, BP regulation during ortho stasis, cardiac function (contractility, stroke volume, cardiac output), MCA via transcranial doppler | Stimulation resolved the orthostatic hypotension. | None noted |
| Calvert et al. [75] (2019) | eSCS + locomotor training | Volitional: EMG, induced movement | Enabled intentional control of step-like activity in both subjects within first 5 days of testing | None noted |
| Cheng et al. [55] (2019) | eSCS + stand training | Volitional: EMG | Spatiotemporal modulation during SCI patient standing leads to activation of an additional neural circuit, which significantly improves patient standing ability. | None noted |
| Darrow et al. [76] (2019) | eSCS | Volitional, cardiovascular, and GU: EMG, EKG, BP, BP regulation during orthostasis, HR, cardiac function (contractility, stroke volume, cardiac output), MCA, bladder function (storage and voiding, incontinence, synergy), bowel synergy, orgasm | Restoration of cardiovascular function in one patient, achieved orgasm in one patient with and immediately after stimulation, improved bowel-bladder synergy in both patients while restoring volitional urination in one patient | None noted |
| Nightingale et al. [57] (2019) | eSCS | Cardiovascular and pulmonary: body composition, metabolic rate, oxygen consumption | Increased absolute and relative peak oxygen consumption (15%-26%) during exercise with stimulation; peak oxygen pulse increased with stimulation. | None noted |
| Terson de Paleville et al. [58] (2019) | eSCS + locomotor training | Cardiovascular and pulmonary: body composition, metabolic rate, oxygen consumption | Increases in lean body mass with decreases on percentage of body fat, particularly android body fat, and android/gynoid ratio from baseline to post training | None noted |
| DiMarco et al. [59] (2020) | eSCS | Pulmonary: airway pressure, air flow rate, volume of respiratory secretions | Following daily use of SCS, mean inspiratory capacity improved from 1,636┬▒229 to 1,932┬▒239 mL (127%┬▒8% of baseline values) after 20 weeks. Mean maximum inspiratory pressure increased from 40┬▒7 to 50┬▒8 cm H2O (127%┬▒6% of baseline values) after 20 weeks. | None noted |
| Gill et al. [79] (2020) | eSCS + body weight supported treadmill training | Volitional: EMG, gait analysis, BWS, TSW, A/I step, proprioception | During eSCS-enabled BWST stepping, the knee extensors exhibited an increase in motor activation during trials in which stepping was passive compared to active or during trials in which 60% BWS was provided compared to 20% BWS. | None noted |
| Gorgey et al. [80] (2020) | eSCS + exo skeletal-assisted walking training | Volitional: EMG, A/I stand, A/I step, OGW, IWS | After 24 sessions (12 weeks) of exoskeleton-assisted walking with eSCS, swing assistance decreased from 100% to 35%, accompanied by 573 unassisted steps. | None noted |
| Pena Pino et al. [81] (2020) | eSCS | Volitional: EMG, cycling, modified Ashworth scale | Some (4/7) achieved volitional movement with no stimulation. | None noted |
| Beck et al. [62] (2021) | eSCS + task-specific training | GU: EMG, incontinence, storage and voiding, urinary complications, Neurogenic Bladder Symptom Score | In one participant, we observed an increase in episodes of urinary incontinence with worsening bladder compliance and pressures at the end of the study. | None noted |
| Calvert et al. [63] (2021) | eSCS | Volitional: EMG | eSCS decreased the amplitude of evoked responses of both patients when instructed to perform a full leg flexion | None noted |
| DiMarco et al. [83] (2021) | eSCS | Pulmonary and GU: airway pressure generation, bowel management, orgasm | Mean pressure during spontaneous efforts was 30┬▒8 cm H2O. After a period of reconditioning, SCS resulted in pressure of 146┬▒21 cm H2O. | None noted |
| Herrity et al. [85] (2021) | eSCS + activity-based recovery training | GU: storage and voiding, urodynamic parameters via cystometry | There was also a significant improvement change in bladder capacity at posttraining (70┬▒83 mL, p<0.05) and at follow-up (102┬▒120 mL, p<0.05). | None noted |
| Ibanez et al. [64] (2021) | eSCS + activity-based recovery training | Volitional: EMG, A/I stand, STS | Human spinal circuitry receiving eSCS can promote both orderly (according to motor neuron size) and inverse trends of motor neuron recruitment. | None noted |
| Linde et al. [87] (2021) | eSCS + locomotor training | Volitional: Force sensitive resistors, gait analysis, TSW | Two participants, both with sensorimotor complete SCI graded AIS-A, were able to improve independence of the stance. | None noted |
| Mesbah et al. [65] (2021) | eSCS + activity-based recovery training | Volitional: EMG | All individuals with chronic and clinically motor complete SCI that participated in the study (n=20) achieved lower extremity voluntary movements posteSCS implant and prior to any training. | None noted |
| Squair et al. [66] (2021) | eSCS | Cardiovascular: plethysmography, BP, BP regulation during ortho stasis, HR | eSCS led to real-time hemodynamic stabilization during orthostatic challenges | None noted |
| Smith et al. [88] (2022) | eSCS + activity-based recovery training | Volitional: EMG, A/I stand, STS | Participants with spared spinal cord tissue (7/11) achieved some knee independence with eSCS | None noted |
eSCS, epidural spinal cord stimulation; EMG, electromyogram; BWST, body weight supported treadmill training; BWS, body weight support; TSW, treadmill step/walk; OGW, overground walking; HCA, home and community access; IWS, increased walking speed; PWBT, partial body weight bearing treadmill training; GU, genitourinary; A/I, assisted/independent; STS, sit to stand transition; BP, blood pressure; HR, heart rate; FRC, functional residual capacity; TLC, total lung capacity; SCS, spinal cord stimulation; EKG, electrocardiogram; AIS-A, American Spinal Injury Association Impairment Scale grade A.
Table┬Ā5.
| Study | Intervention | Type of outcome studied | Measured outcome | Complications |
|---|---|---|---|---|
| Hofstoetter et al. [30] (2013) | tSCS + treadmill stepping | Volitional (changes in muscle activity): EMG, gait analysis, treadmill step/walk | Enhanced voluntary lower limb EMG activities in a step-phase appropriate manner with stimulation, modified coordination of hip and knee movements | None noted |
| Hofstoetter et al. [31] (2014) | tSCS | Volitional (changes in muscle activity): EMG, gait analysis, IWS, spasticity | Increased index of spasticity from pendulum test, increased gait speed during stimulation in two subjects by 39% | None noted |
| Bedi et al. [33] (2015) | tSCS + locomotor training | Volitional: EMG, ASIA score | Improvement in ASIA score of lower limb by 2 points on right side and by 1 point on left side. | None noted |
| Gerasimenko et al. [34] (2015) | tSCS | Volitional: EMG | Induced rhythmic leg movements and corresponding coordinated movement EMG activity in leg muscles with stimulation | None noted |
| Hofstoetter et al. [35] (2015) | tSCS + treadmill stepping | Volitional (changes in muscle activity): EMG, gait analysis, treadmill step/walk | Motor outputs augmentative and step-phase dependent during stimulation, increased hip flexion during swing by 11.3┬░┬▒5.6┬░ across all subjects | None noted |
| Bedi et al. [37] (2016) | tSCS | Volitional: EMG, ASIA score | Increased firing rate of active muscle units during stimulation | None noted |
| Minassian et al. [39] (2016) | tSCS + robotic-driven gait orthosis | Volitional (changes in muscle activity): EMG, gait analysis, treadmill step/walk | Increased number of rhythmically responding muscles, augmented thigh muscle activity, and suppressed clonus with stimulation. | None noted |
| Gad et al. [40] (2017) | tSCS + exo skeleton + bus-pirone | Volitional and cardiovascular: EMG, gait analysis, BP, HR | Increased patient generation of level of effort, improved coordination patterns of the lower limb muscles, smoother stepping motion, increased blood pressure and heart rate | None noted |
| Freyvert et al. [69] (2018) | tSCS + buspirone | Volitional: EMG, handgrip strength, ASIA score, spasticity | Increased mean hand strength by 300% with stimulation and buspirone, some functional improvements persisted after interventions discontinued | None noted |
| Gad et al. [70] (2018) | tSCS + functional task training | Volitional: EMG, handgrip strength | Improved voluntary hand function occurred within a single session in every subject tested. | None noted |
| Inanici et al. [73] (2018) | tSCS + PT | Volitional: EMG, handgrip force, GRASSP score, ASIA score | Graded Redefined Assessment of Strength, Sensation, and Prehension (GRASSP) test score increased 52 points and upper extremity motor score improved 10 points. Sensation recovered on trunk dermatomes, and overall neurologic level of injury improved from C3 to C4. | Mild, painless hyperemia under electrode, self-resolved |
| Niu et al. [74] (2018) | tSCS | GU: EMG, storage and voiding | Bladder function improved in all five subjects, but only during and after repeated weekly sessions of 1 Hz TMSCS. All subjects achieved volitional urination. | None noted |
| Phillips et al. [50] (2018) | tSCS | Cardiovascular: BP, cardiac function (contractility, stroke volume, cardiac output), MCA and PCA velocity | During orthostatic challenge, electrical stimulation completely normalized BP, cardiac contractility, cerebral blood flow, and abrogated all symptoms. | None noted |
| Powell et al. [51] (2018) | tSCS | Volitional: EMG | No significant differences in change of MEP amplitudes but indication of laterality of response. | None noted |
| Rath et al. [52] (2018) | tSCS | Volitional: EMG, gait analysis, BWS | During spinal stimulation, the center of pressure displacements decreased to 1.36┬▒0.98 mm compared with 4.74┬▒5.41 mm without stimulation in quiet sitting. | None noted |
| Knikou et al. [56] (2019) | tSCS | Volitional: EMG | Repeated stimulation increased homosynaptic depression in all SCI subjects. Stimulation decreased the severity of spasms and ankle clonus. | None noted |
| Sayenko et al. [77] (2019) | tSCS + locomotor training | Volitional: EMG, BWS, A/I stand | All participants could maintain upright standing with stimulation, some (7/15) without external assistance applied to the knees or hips, using their hands for upper body balance as needed. | One case of skin breakage due to electrode defect, resolved after a week without stimulation |
| Alam et al. [78] (2020) | tSCS + locomotor training | Volitional: EMG, gait analysis, BWS, A/I stand | After 32 training sessions with tSCS, the patient regained significant leftŌĆÉleg volitional movements and improved pinprick sensation. | None noted |
| Gad et al. [60] (2020) | tSCS | Pulmonary: EMG, airway pressure, air flow rate, volume of respiratory secretions | Improved breathing and coughing ability both during and after stimulation | None noted |
| Wiesener et al. [61] (2020) | tSCS + FES + swim training | Volitional: EMG, swim analysis, increased swimming speed, cycling, spasticity | tSCS support yielded mean decreases of swimming pool lap times by 19.3% and 20.9% for Subjects A and B, respectively. | None noted |
| Wu et al. [82] (2020) | tSCS | Volitional: EMG | Resting motor threshold at the abductor pollicis brevis muscle ranged from 5.5 to 51.0 mA. As stimulus intensity increased, response latencies to all muscles decreased. | Asymptomatic sustained 20% or greater change in mean arterial pressure, self-resolved |
| Calvert et al. [63] (2021) | tSCS | Volitional: EMG | All 4 AIS-B/C participants tested with tSCS demonstrated a reduction in the evoked responses amplitude during stimulation compared to the normalized relaxed value in at least 3 out of 4 of the recorded muscles. | None noted |
| Estes et al. [84] (2021) | tSCS + locomotor training | Volitional: gait analysis, IWS, spasticity | Significant improvements in walking outcomes following the intervention period | Discomfort, tightness in the abdomen and lower back near electrodes |
| Inanici et al. [86] (2021) | tSCS + functional task training | Volitional, cardiovascular, and GU: GRASSP, lateral pinch force, spasticity, HR, storage and voiding | Rapid and sustained recovery of hand and arm function. Muscle spasticity reduced and autonomic functions including heart rate, thermoregulation, and bladder function improved. | Mild allergic skin rash |
tSCS, epidural spinal cord stimulation; EMG, electromyogram; IWS, increased walking speed; AISA, American Spinal Cord Injury Association; BP, blood pressure; HR, heart rate; GU, genitourinary; PCA, posterior cerebral artery; MCA, middle cerebral artery; BWS, body weight support; A/I, assisted/independent; AIS-B/C, American Spinal Injury Association Impairment Scale grade B/C.
REFERENCES

- TOOLS
- Related articles in NS
-
Surgical Considerations to Improve Recovery in Acute Spinal Cord Injury2022 September;19(3)