- Search
|
|
||
Abstract
Objective
To develop a nomogram for the prediction of tracheostomy in patients with traumatic cervical spinal cord injury (TCSCI).
Methods
A total of 689 TCSCI patients were included in our study. First, the variable selection was performed using between-group comparisons and LASSO regression analysis. Second, a multivariate logistic regression analysis (MLRA) with a step-by-step method was performed. A nomogram model was developed based on the MLRA. Finally, the model was validated on the training set and validation set.
Results
The nomogram prediction model incorporated 5 predictors, including smoking history, dislocation, thoracic injury, American Spinal Injury Association (ASIA) grade, and neurological level of injury (NLI). The area under curve in the training group and in the validation group were 0.883 and 0.909, respectively. The Hosmer-Lemeshow test result was p = 0.153. From the decision curve analysis curve, the model performed well and was feasible to make beneficial clinical decisions.
Traumatic cervical spinal cord injury (TCSCI) is a devastating disease that leads to lifelong disability and long-term risk of medical complications [1-3]. TCSCI often results in acute respiratory failure [4]. Many researchers have demonstrated that early tracheostomy (≤ 7 days from intubation) can bring many benefits to patients with TCSCI [4-7]. For example, early tracheostomy may reduce mechanical ventilation (MV) time and allow for more comfortable and efficient breathing. To take advantage of these benefits and allocate resources accordingly, it is important for surgeons to have a tool to predict whether a patient might need a tracheostomy.
Although several factors for tracheostomy have been identified through multivariate logistic regression analysis (MLRA) and classification and regression tree (CART) model [8-11], early prediction of tracheostomy in TCSCI patients is still difficult. The nomogram is an essential part of modern medicine and is considered a reliable and practical predictive tool [12,13]. The nomogram can visually display the results of MLRA, and can also predict the probability through a simple picture representation [14-16]. To the best of our knowledge, no nomogram prediction model of tracheostomy has been reported in TCSCI patients. The purpose of this study was to develop and validate a simple and convenient nomogram model for predicting tracheostomy after TCSCI.
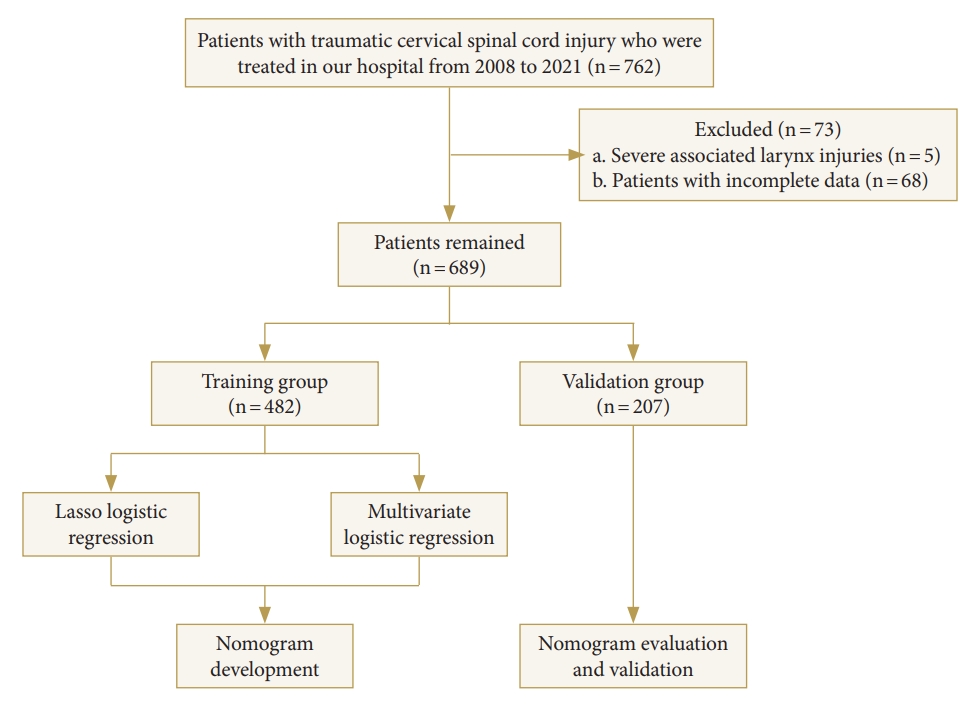
This was a retrospective study. This study was based on data from a university hospital in Chongqing, China between January 2008 to December 2021. It was approved by the Ethics Committee of our hospital. TCSCI was diagnosed by taking into account a history of trauma, symptoms, consciousness, sensory and motor, complete neurological testing, and imaging findings such as computed tomography and/or magnetic resonance imaging [17]. The decision to perform a tracheostomy was made by the spine surgeon in conjunction with the intensive care unit physician and was made when prolongation of the MV was expected, considering the patient’s neurologic function, respiratory function, age, concomitant injury, and other factors. Tracheostomy was performed if any of the following criteria were met: (1) the patient was retained in a transoral tracheal tube and failed to evacuate MV after several attempts; (2) the patient had a lot of sputum and poor coughing power, requiring retention of an artificial airway to drain sputum. All assessments were performed by experienced senior physicians on admission. The overall flow chart is shown in Fig. 1.
A total of 762 patients with TCSCI in the department of orthopedics were analyzed. The inclusion criteria were as follows: (1) clear history of trauma, (2) well-diagnosed cervical spinal cord injury, and (3) complete medical records. The exclusion criteria were as follows: (1) larynx injuries, (2) patients who underwent tracheostomy at other hospital, and (3) incomplete medical records. Finally, 689 patients were included in the study sample.
The relevant patient’s data were recorded, including sex, age, smoking history, dislocation, diabetes mellitus, hypertension, preexisting lung disease, brain injury, American Spinal Injury Association (ASIA) impairment scale grade, neurological level of injury (NLI), and thoracic injury. ASIA impairment scale grade was assessed using the ASIA standards [18]. ASIA impairment scale grade was divided into grades A and B–D. NLI was divided into C1–4 and C5–8. The dislocation was defined as traumatic cervical facet dislocation confirmed by radiological examination. Preexisting lung diseases included chronic obstructive pulmonary disease, bronchial asthma, and restrictive lung disease. According to World Health Organization, smoking was defined as continuous or cumulative smoking for 6 months or more in a lifetime [19].
All patients were randomized into training and validation groups, in a 7:3 ratio for nomogram construction and validation. Pearson chi-square test and LASSO regression analysis were used to screen variables. The screened variables were brought into MLRA in a step-by-step method to determine the independent predictors. Based on the MLRA, a nomogram prediction model of tracheostomy was constructed. The area under curve (AUC) was calculated in training and validation groups to measure the predictive accuracy of the nomogram model. The calibration curve and Hosmer-Lemeshow test were performed to assess the predictive ability of the nomogram. The decision curve analysis (DCA) was performed to evaluate the predictive model. All analyses and nomogram development were performed using R ver. 4.2.0 (R Foundation for Statistical Computing, Vienna, Austria). A p-value of < 0.05 was considered statistically significant.
In the training group, 482 patients with TCSCI, and 74 patients (15.4%) underwent tracheostomy. The baseline characteristics of patients in the training group are shown in Table 1. A comparison of patients with and without tracheostomy is shown in Table 2. Compared with the nontracheostomy group, the tracheostomy group presents a significant difference in age ≥ 60 years, sex, smoking history, dislocation, ASIA impairment scale, NLI, and thoracic injury (p < 0.05).
The variables screened by LASSO regression analysis were: age, smoking history, dislocation, ASIA impairment scale grade, NLI, and thoracic injury (Fig. 2A, B). Their optimal coefficients were 0.029, 0.297, 0.847, 1.830, 1.097, and 0.535, respectively. These 6 variables selected by the LASSO regression with nonzero coefficients were included in the MLRA analysis. The results of the MLRA are given in Table 3. Five variables, including smoking history, dislocation, thoracic injury, ASIA impairment scale grade, and NLI, showed significant statistical differences.
Using these 5 variables, a nomogram model for predicting tracheostomy was developed (Fig. 3). Each factor corresponded to a score at the top of the nomogram, and the total score was calculated and compared to the bottom of the nomogram to predict tracheostomy risk. The AUC in the training group was 0.883. The best cutoff point was 0.124 (sensitivity, 0.838; specificity, 0.770) (Fig. 4A), which indicated that the discrimination of the nomogram model was good. The calibration curve of the nomogram model revealed satisfactory consistency (Fig. 5A).
Twenty-eight patients (13.5%) in the validation group underwent tracheostomy. The result of the Hosmer-Lemeshow test was p = 0.153. The AUC in the validation group was 0.909. The best cutoff point was 0.136 (sensitivity, 0.893; specificity, 0.777) (Fig. 4B), which indicated that the discrimination of the nomogram model was good. The calibration curve of the nomogram model revealed satisfactory consistency in the validation group (Fig. 5B).
The study presented 102 of 689 TCSCI patients who underwent tracheostomy to comprehensively screen the independent risk factors. In the MLRA analysis, dislocation, thoracic injury, ASIA grade A, NLI, and smoking history were associated with tracheostomy in TCSCI patients. Based on these results, a nomogram model was developed. Then, the model was validated on the training set and validation set. This nomogram model showed that dislocation, thoracic injury, ASIA grade A, NLI at C1–4, and smoking history were key predictors. This study provided a relatively reliable nomogram model. It exhibited relatively good discrimination and calibration capabilities.
The ASIA grade A has been regarded as an essential predictor for tracheostomy in TCSCI patients [10,20-26]. It was also an important predictor in the CART model for predicting tracheostomy [8]. In the results of Childs et al. [27], they even suggested early tracheostomy in all patients with ASIA A. Consistent with previous research, the present MLRA results revealed that the ASIA grade A was a significant predictor of tracheostomy. In this nomogram prediction model, the score corresponding to ASIA grade A was the highest.
Due to diaphragm and/or intercostal muscle dysfunction, NLI was considered to be another important predictor for tracheostomy in TCSCI patients [25,28-31]. Tanaka et al. [32] suggested that tracheostomy may be required in patients with NLI C4 or above. The present study also classified NLI into C1–4 and C5–8. Consistent with previous studies, the score corresponding to NLI at C1–4 were also high in our nomogram prediction model.
This predictive model also included dislocation, smoking history, and thoracic injury. Cervical dislocations mostly cause spinal cord compression and dramatic neurological deficits. Mu et al. [26] also found that facet dislocation was a significant risk factor for tracheostomy in patients with TCSCI. Smoking increases susceptibility to pulmonary infection and the development of cigarette smoke-induced lung diseases [33]. Similarly, Nakashima et al. [11] found that one of the risk factors for tracheostomy was smoking history. One intriguing finding of the study was that thoracic injury was a predictor of tracheostomy. In the nomogram prediction model, thoracic injury corresponds to a score roughly around 50, between smoking history and dislocation.
Several risk variables associated with tracheostomy were presented in other studies, but not included in the present study. Some authors found that age was a statistically significant risk factor and that older age groups were more likely to undergo tracheostomy [10,21,26,34,35]. Controversially, other authors argued that age is not a risk factor [8,11,20,22,24,25,32]. Some scholars have introduced the forced vital capacity (FVC) variable in their prediction models [9,10]. However, using FVC for the predicted predictions has some shortcomings. For example, those who suffer great injury had to receive a tracheostomy may not have acceptable and reproducible pulmonary function test results [8,36].
There are 3 limitations to this study. First, this study was based on retrospective data from a single-specialty spine injury center, so the level of evidence is limited. Second, indications for tracheostomy in patients with TCSCI varied between institutions. Third, although the population was relatively large, the patients were from a single hospital. So, representation needs to be further improved.
The present study developed and validated a nomogram model that can predict tracheostomy in TCSCI patients. The nomogram combining dislocation, thoracic injury, ASIA grade A, NLI, and smoking history was validated as a reliable model for tracheostomy prediction. The present nomogram prediction model can help clinicians take timely and more targeted medical interventions.
NOTES
Fig. 2.
(A) LASSO regression model screening predictors. By verifying the optimal parameter (lambda) in the LASSO model, the partial likelihood deviance (binomial deviance) curve was plotted versus log (lambda), while dotted vertical lines were drawn based on 1 standard error criteria. (B) A coefficient profile plot was produced against the log (lambda) sequence. 1: sex, 2: age, 3: smoking history, 4: dislocation, 5: diabetes mellitus, 6: hypertension, 7: American Spinal Injury Association grade, 8: neurological level of injury, 9: brain injury, 10: thoracic injury, 11: preexisting lung disease. Six variables with nonzero coefficients were selected by optimal lambda.
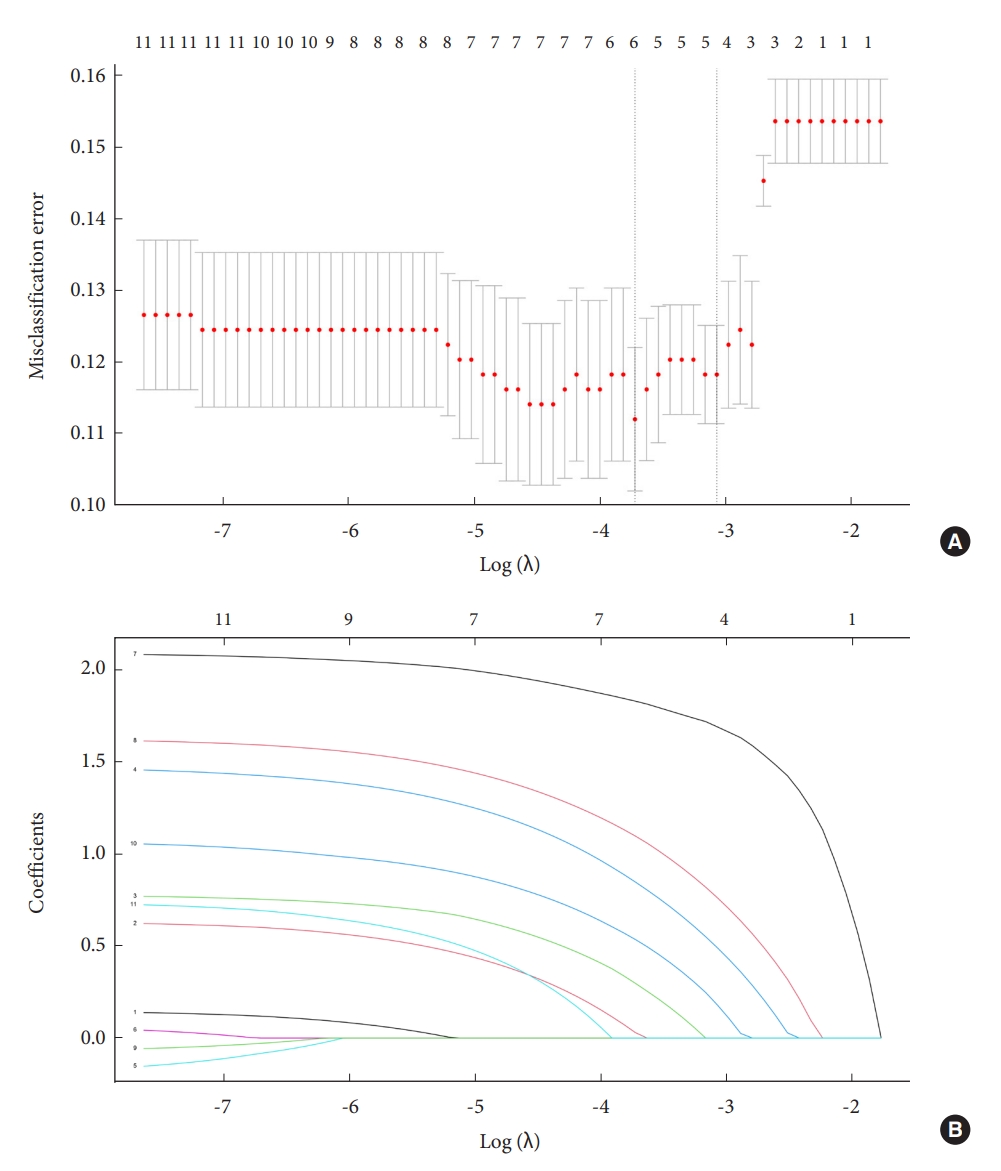
Fig. 3.
The nomogram model for prediction of tracheostomy. ASIA, American Spinal Injury Association; NLI, neurological level of injury.
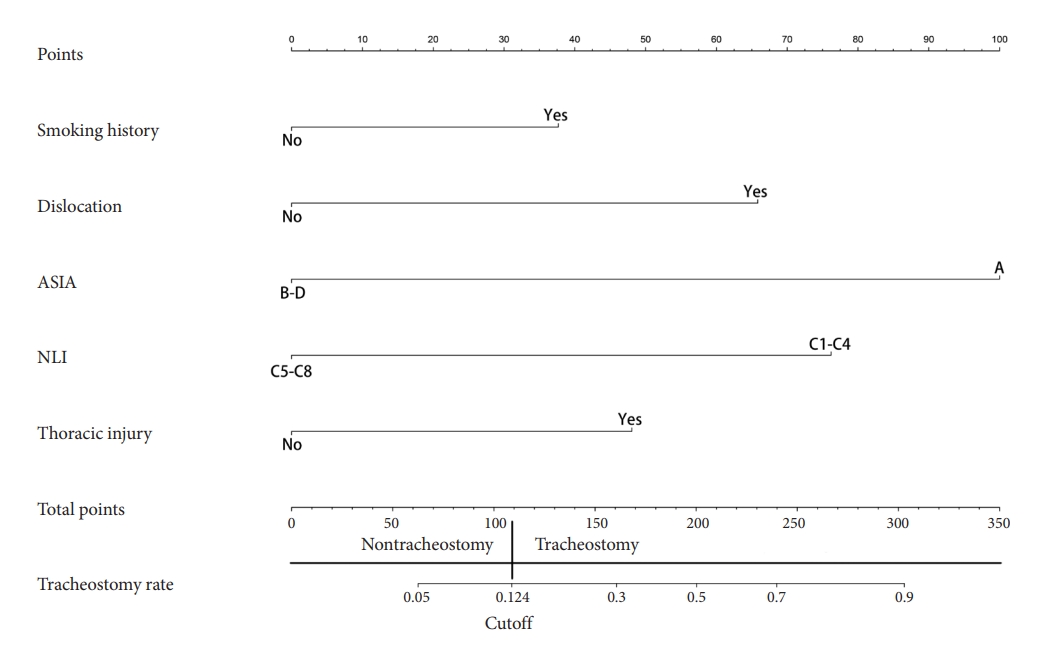
Fig. 4.
Receiver operating characteristic (ROC) curve of the nomogram model. The training group (A) and the validation group (B). AUC, area under the curve.
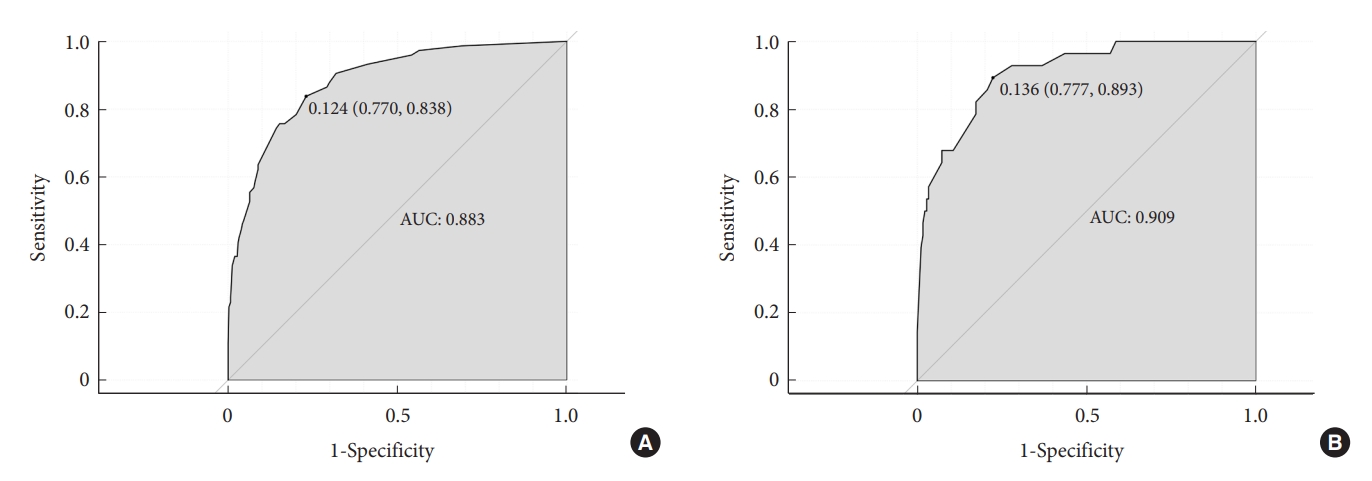
Fig. 5.
Calibration curve to confirm the prediction performance stability of the nomogram. The training group (A) and the validation group (B).
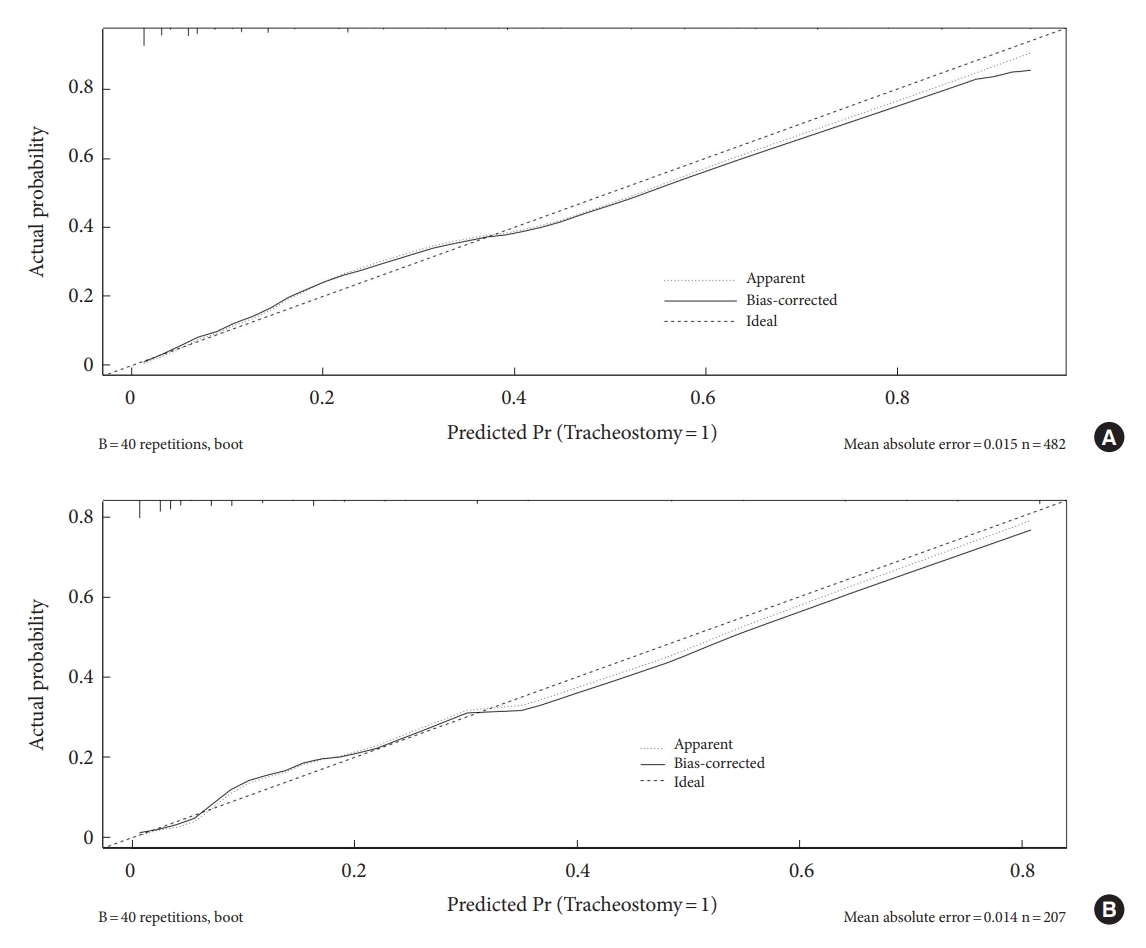
Table 1.
Characteristics of patients with traumatic cervical spinal cord injury in the training and validation groups
Table 2.
Comparison of data between patients with and without tracheostomy in the training group
Table 3.
Multivariate logistic regression analysis performed in a step-by-step method for the tracheostomy in patients with traumatic cervical spinal cord injury in training group
REFERENCES
1. Investigators O, Chikuda H, Koyama Y, et al. Effect of early vs delayed surgical treatment on motor recovery in incomplete cervical spinal cord injury with preexisting cervical stenosis: a randomized clinical trial. JAMA Netw Open 2021;4:e2133604.


2. Gadot R, Smith DN, Prablek M, et al. Established and emerging therapies in acute spinal cord injury. Neurospine 2022;19:283-96.




3. Sanchez JAS, Sharif S, Costa F, et al. Early management of spinal cord injury: WFNS Spine Committee Recommendations. Neurospine 2020;17:759-84.




4. Flanagan CD, Childs BR, Moore TA, et al. Early tracheostomy in patients with traumatic cervical spinal cord injury appears safe and may improve outcomes. Spine 2018;43:1110-6.


5. Mubashir T, Arif AA, Ernest P, et al. Early versus late tracheostomy in patients with acute traumatic spinal cord injury: a systematic review and meta-analysis. Anesth Analg 2021;132:384-94.


6. Beom JY, Seo HY. The need for early tracheostomy in patients with traumatic cervical cord injury. Clin Orthop Surg 2018;10:191-6.




7. Foran SJ, Taran S, Singh JM, et al. Timing of tracheostomy in acute traumatic spinal cord injury: a systematic review and meta-analysis. J Trauma Acute Care Surg 2022;92:223-31.



8. Hou Y, Lv Y, Zhou F, et al. Development and validation of a risk prediction model for tracheostomy in acute traumatic cervical spinal cord injury patients. Eur Spine J 2015;24:975-84.



9. Berney S, Gordon I, Opdam H, et al. A classification and regression tree to assist clinical decision making in airway management for patients with cervical spinal cord injury. Spinal Cord 2011;49:244-50.



10. Yugué I, Okada S, Ueta T, et al. Analysis of the risk factors for tracheostomy in traumatic cervical spinal cord injury. Spine 2012;37:E1633-8.


11. Nakashima H, Yukawa Y, Imagama S, et al. Characterizing the need for tracheostomy placement and decannulation after cervical spinal cord injury. Eur Spine J 2013;22:1526-32.




12. Balachandran VP, Gonen M, Smith JJ, et al. Nomograms in oncology: more than meets the eye. Lancet Oncol 2015;16:e173-80.



13. Mo R, Shi R, Hu Y, et al. Nomogram-based prediction of the risk of diabetic retinopathy: a retrospective study. J Diabetes Res 2020;2020:7261047.




14. Lv J, Liu YY, Jia YT, et al. A nomogram model for predicting prognosis of obstructive colorectal cancer. World J Surg Oncol 2021;19:337.




15. Raghav K, Hwang H, Jacome AA, et al. Development and validation of a novel nomogram for individualized prediction of survival in cancer of unknown primary. Clin Cancer Res 2021;27:3414-21.




16. Liu S, Yu X, Yang S, et al. Machine learning-based radiomics nomogram for detecting extramural venous invasion in rectal cancer. Front Oncol 2021;11:610338.



18. Maynard FM Jr, Bracken MB, Creasey G, et al. International Standards for Neurological and Functional Classification of Spinal Cord Injury. American Spinal Injury Association. Spinal Cord 1997;35:266-74.



19. World Health Organization. Guidelines for controlling and monitoring the tobacco epidemic. Geneva (Switzerland): World Health Organization; 1998.
20. Higashi T, Eguchi H, Wakayama Y, et al. Analysis of the risk factors for tracheostomy and decannulation after traumatic cervical spinal cord injury in an aging population. Spinal Cord 2019;57:843-9.



21. Lee D, Park C, Carriere K, et al. Classification and regression tree model for predicting tracheostomy in patients with traumatic cervical spinal cord injury. Eur Spine J 2017;26:2333-9.



22. McCully BH, Fabricant L, Geraci T, et al. Complete cervical spinal cord injury above C6 predicts the need for tracheostomy. Am J Surg 2014;207:664-8. discussion 8-9.


23. Leelapattana P, Fleming J, Gurr K, et al. Predicting the need for tracheostomy in patients with cervical spinal cord injury. J Trauma Acute Care Surg 2012;73:880-4.


24. Branco BC, Plurad D, Green DJ, et al. Incidence and clinical predictors for tracheostomy after cervical spinal cord injury: a National Trauma Databank review. J Trauma 2011;70:111-5.


25. Long PP, Sun DW, Zhang ZF. Risk factors for tracheostomy after traumatic cervical spinal cord injury: a 10-year study of 456 patients. Orthop Surg 2022;14:10-7.




26. Mu Z, Zhang Z. Risk factors for tracheostomy after traumatic cervical spinal cord injury. J Orthop Surg (Hong Kong) 2019;27:2309499019861809.



27. Childs B, Moore T, Como J, et al. American Spinal Injury Association Impairment Scale predicts the need for tracheostomy after cervical spinal cord injury. Spine 2015;40:1407-13.


28. Berney S, Bragge P, Granger C, et al. The acute respiratory management of cervical spinal cord injury in the first 6 weeks after injury: a systematic review. Spinal Cord 2011;49:17-29.



29. Romero J, Vari A, Gambarrutta C, et al. Tracheostomy timing in traumatic spinal cord injury. Eur Spine J 2009;18:1452-7.




30. Ganuza JR, Oliviero A. Tracheostomy in spinal cord injured patients. Transl Med UniSa 2011;1:151-72.


31. Schilero GJ, Spungen AM, Bauman WA, et al. Pulmonary function and spinal cord injury. Respir Physiol Neurobiol 2009;166:129-41.


32. Tanaka J, Yugue I, Shiba K, et al. A study of risk factors for tracheostomy in patients with a cervical spinal cord injury. Spine 2016;41:764-71.


33. Lugg ST, Scott A, Parekh D, et al. Cigarette smoke exposure and alveolar macrophages: mechanisms for lung disease. Thorax 2022;77:94-101.



34. Harrop JS, Sharan AD, Scheid EH Jr, et al. Tracheostomy placement in patients with complete cervical spinal cord injuries: American Spinal Injury Association Grade A. J Neurosurg 2004;100(1 Suppl Spine):20-3.