- Search
|
|
||
Abstract
Objective
We attempted to investigate the potential risk factors of recurrent lumbar disc herniation (rLDH) after tubular microdiscectomy.
Methods
We retrospectively analyzed the data of patients who underwent tubular microdiscectomy. The clinical and radiological factors were compared between the patients with and without rLDH.
Results
This study included 350 patients with lumbar disc herniation (LDH) who underwent tubular microdiscectomy. The overall recurrence rate was 5.7% (20 of 350). The visual analogue scale (VAS) score and Oswestry Disability Index (ODI) at the final follow-up significantly improved compared with those preoperatively. There was no significant difference in the preoperative VAS score and ODI between the rLDH and non-rLDH groups, while the leg pain VAS score and ODI of the rLDH group were significantly higher than those of the non-rLDH group at final follow-up. This suggested that rLDH patients had a worse prognosis than non-rLDH patients even after reoperation. There were no significant differences in sex, age, body mass index, diabetes, current smoking and drinking, disc height index, sagittal range of motion, facet orientation, facet tropism, Pfirrmann grade, Modic changes, interdisc kyphosis, and large LDH between the 2 groups. Univariate logistic regression analysis revealed that rLDH was associated with hypertension, multilevel microdiscectomy, and moderate-severe multifidus fatty atrophy (MFA). A multivariate logistic regression analysis indicated that MFA was the sole and strongest risk factor for rLDH after tubular microdiscectomy.
Lumbar disc herniation (LDH) is a very common lumbar degenerative disease and imposes a significant burden on patients worldwide [1]. The lifetime incidence of LDH is estimated to be between 13% and 40%, with major socioeconomic implications [2]. LDH is rare before the age of 20, and its incidence reaches a peak around the age of 50 and then declines gradually [3]. The incidence of LDH did not differ between the sexes [2]. However, different professions or sports may influence incidence of LDH. For example, the machine operators and carpenters are more likely to suffer from LDH than sedentary office workers [4]. Awkward working postures, such as bending or twisting the torso for a long time, or frequent exposure to strenuous physical activity can increase the incidence of LDH [5,6]. Additionally, except jogging and walking, overall physical exercise and most physical activities will not increase the incidence rate of LDH [5].
Conservative treatment is usually recommended at the onset of disease [7]. Surgical treatment such as microdiscectomy is usually recommended when conservative treatment fails [8]. However, its complications, especially recurrent LDH (rLDH), have been reported to occur in 5%–15% of patients after primary surgery [9]. Patients undergoing reoperation tend to have longer operative times or hospital stays [10,11], more difficult procedures [12], and a poorer prognosis or quality of life [13-16] than do patients undergoing primary surgery. Therefore, it is necessary to identify patients with LDH at risk for surgical revision prior to the initial surgery.
Current clinical studies have identified some possible related or risk factors for the recurrence of LDH [17-65]. In terms of clinical factors, studies have found that sex, age, obesity, smoking, and diabetes may be risk factors for rLDH [18,20-27]. In terms of radiological factors, it was found that the degree of disc degeneration, Modic changes, disc height, facet direction, and sagittal range of motion (sROM) are related to rLDH [21,28-31]. Nevertheless, the current reality is that whether these clinical or radiological variables do affect rLDH remains controversial. For example, the sex of female was found to be a risk factor for rLDH [20], while some studies have found the opposite outcomes [21-23]. There are also different conclusions about the relationship between age and rLDH [18,24-27]. Furthermore, in addition to some variables that have been extensively studied previously, we hypothesize that some common but not studied variables such as interdisc kyphosis, large LDH, and multifidus fatty atrophy (MFA) may to be related to rLDH in this study.
rLDH is a complex process involving biomechanics and social behavior. A single consideration may be inadequate for this complex process. Thus, a comprehensive analysis of clinical and radiological variables for rLDH was developed for better surgical planning and assessment of the prognosis in this study.
We retrospectively analyzed the data from patients who underwent microdiscectomy in a single spine center by one qualified surgeon from December 2016 to December 2020. This study was approved by the Ethics Committee of Xinqiao Hospital of the Army Medical University (2022-499-01).
The inclusion criteria were as follows: (1) microdiscectomy for LDH and (2) follow-up duration of > 1 year. The exclusion criteria were as follows: (1) extreme lateral disc herniation or calcified disc herniation and (2) follow-up duration of < 1 year. The extreme lateral disc herniation was defined as a herniated disc located outside the intervertebral foramen.
We collected data on the basic information and clinical outcomes of the patients, including sex, age, body mass index (BMI), diabetes, hypertension, current smoking and drinking, and multilevel microdiscectomy (≥ 2 levels). Additionally, we collected the low back pain and leg pain visual analogue scale (VAS) [66] scores and Oswestry Disability Index (ODI) [67] of the patients preoperatively and at the final follow-up. All clinical data were recorded by qualified clinical follow-up staff. The follow-up methods included outpatient clinic visits and telephone interviews. For the patients who were followed up through outpatient clinic visits, we completed the ODI questionnaire face-to-face. For those who were followed up through telephone interviews, we completed the ODI questionnaire by asking them question-by-question. In addition, the postoperative low back pain and leg pain VAS scores were evaluated. For the patients with recurrent symptoms, we re-examined their lumbar magnetic resonance imaging (MRI) scans to determine whether they had rLDH. rLDH was defined as reherniation in the same segment and the same side on repeated MRI consistent with this symptom after at least 1 month of symptom relief after surgery. In the previous studies, the pain-free interval is inconsistent, ranging from 2 weeks to 6 months [44]. We took one month as the minimum pain-free interval after prior surgery in this study. The “recurrent symptoms” which we defined must be similar to or more serious than those before the primary surgery, especially lower limb symptoms. Mild back pain or remnant paresthesia will not be defined as a recurrence.
All included patients underwent lumbar radiography, computed tomography, and MRI before surgery. The radiological variables assessed included the herniated disc Pfirrmann grade [68], Modic changes [69], disc height index (DHI), sROM [30], facet orientation (FO) [70], facet tropism (FT) (Fig. 1) [70], interdisc kyphosis, large LDH, and degree of MFA (Fig. 2C) [71]. Pfirrmann grades I, II, and III are defined as low grades and Pfirrmann grades IV and V as senior grades. Modic change is divided into 3 types based on different intervertebral signals on MRI. Type I: hypointense signal in T1-weighted imaging (T1WI) and hyperintense signal in T2-weighted imaging (T2WI). Type II: hyperintense signal in T1WI and hyperintense signal in T2WI. Type III: hypointense signal in T1WI and hypointense signal in T2WI. DHI was defined as the ratio of the disc height to the lower vertebral body height on the lumbar lateral x-ray of the herniated disc segment (Fig. 3A, B). sROM was defined as the value of the hyperextension intervertebral angle minus the hyperflexion intervertebral angle on the lumbar lateral x-ray of the herniated disc segment (Fig. 3C, D). FO was defined as the mean value of the right and left facet joint angle degrees (Fig. 1). FT was defined as the absolute value of the difference between the right and left facet joint angle degrees (Fig. 1). Large LDH was defined as the herniated disc account for over 50% of the spinal canal area on axial MRI (Fig. 2A, B). Interdisc kyphosis was defined as lordosis angle of the intervertebral space at the surgical segment in the lateral x-ray is less than 0°. If it is greater than or equal to 0°, it does not belong to interdisc kyphosis (Fig. 3E, F). MFA is divided into 4 grades based on the multifidus muscle’s cross-sectional area on herniated disc level (Fig. 2D, G). That is, 0%–10% fatty infiltration (normal), 10%–30% fatty infiltration (mild), 30%–50% fatty infiltration (moderate), and more than 50% fatty infiltration (severe). All radiological factors were measured and assessed by 2 qualified radiologists blinded to the research design. All numerical results were expressed as the mean values of the radiological variables measured by the 2 radiologists. All radiological variables that need to be measured were completed through Surgimap software (Nemaris, New York, NY, USA). For the degree of MFA, we originally preformed the quantitative measurements of muscle fatty atrophy based on the quantification. The mean value of the measurements by the 2 radiologists was adopt. Then, we performed the qualitative analysis according to the quantitative values. These cases were classified as normal, mild, moderate, and severe MFA according to the fatty infiltration ratio.
All patients underwent standardized tubular microdiscectomy according to our previously reported method [72,73] performed by one qualified surgeon (HB) in a single spine center. Patients were placed in prone position after general anesthesia. After positioning of the surgical segment, an incision was made approximately 1 cm lateral to the midline on the symptomatic side of the identified surgical segment. A surgical pathway to the lumbar spine was created by inserting the sequential dilators through the multifidus. We usually implanted a tapered retractor with a diameter of 20–22 mm on the upper end and a diameter of 16–18 mm on the opposite end (Bosscom Technology, Chongqing, China) (Fig. 4A). In this procedure, we removed the inferior edge of the lower lamina and the inner edge of the inferior articular process. The overlying ligamentum flavum was then excised and the nerve root was exposed. Then, the herniated disc was exposed and removed under a microscope (Carl Zeiss, Inc., Oberkochen, Germany) (Fig. 4B). We do not destroy the disc of origin in the process of removing the herniation. The surgical philosophy is to remove a herniated disc with minimal disruption of the normal disc under a microscope (limited discectomy).
The Kolmogorov-Smirnov test was used to test the distribution of the data. Normally distributed data were analyzed using the t-test and nonnormally distributed data using the Wilcoxon Mann-Whitney U-test. Initially, we compared the differences in the clinical and radiological outcomes between the non-rLDH and rLDH groups using a univariate analysis. Student t-test or the Wilcoxon Mann-Whitney test was used to examine the differences in age, BMI, DHI, sROM, FO, and FT. The chi-square or Fisher exact test was used to examine the differences in sex, diabetes, hypertension, current smoking and drinking, disc degeneration, Modic changes, multilevel microdiscectomy, MFA, interdisc kyphosis, and large LDH.
Thereafter, we performed univariate and multivariate logistic regression analyses to assess the relationship between rLDH and the independent variables with a p-value of < 0.2. The Omnibus tests of model coefficients were used to test the effectiveness of this multivariate logistic regression analysis model. The Hosmer-Lemeshow test was used to evaluate whether the model makes full use of the existing information, fits the model to the greatest extent, and explains the variation of the model. The statistical significance level was set at a p-value of < 0.05. Statistical analysis was performed using IBM SPSS Statistics ver. 21.0 (IBM Co., Armonk, NY, USA). The forest plot of the multivariable analysis was drawn by the Graphpad Prism 6.0 (Graphpad Software Inc., San Diego, CA, USA).
A total of 506 patients were initially enrolled. Among them, 104 patients with lack of clinical or radiological data, 34 patients with calcified disc herniation, and 18 patients with extreme lateral disc herniation were excluded. Finally, 350 patients who met the inclusion criteria from December 2016 to December 2020 were included in this study. Among them, 330 patients were classified into the non-rLDH group and 20 patients (5.7%) into the rLDH group. In 20 patients with rLDH, the time from primary surgery to recurrence is 2 to 54 months (mean, 26.5 months). The follow-up time after recurrence was 6–58 months (mean, 24.2 months).
A total of 208 patients were men, and 142 were women. The mean age, BMI, and follow-up time were 48.5 ± 14.4 years, 24.5 ± 3.4 kg/m2, and 37 ± 12.5 months, respectively. The mean lower back and leg VAS scores and ODI at the final follow-up significantly improved compared with those preoperatively. Among the rLDH patients, 9 patients underwent tubular microdiscectomy again, 6 patients cases underwent minimally invasive transforaminal lumbar interbody fusion (Mis-TLIF), 4 patients underwent TLIF, and 1 patient underwent conservative treatment. Although the preoperative VAS score and ODI in the rLDH group were not significantly different from those in the non-rLDH group, the leg VAS score (p = 0.01) and ODI (p = 0.002) at the final follow-up in the rLDH group (get additional treatment after recurrence) were significantly higher than those in the non-rLDH group. This suggested This suggested that despite reoperation in the majority of rLDH patients, they had a worse prognosis than non-rLDH patients.
The outcomes of the univariate analysis are shown in Tables 1 and 2. In terms of the clinical factors, we did not find significant differences in sex, age, BMI, diabetes, or current smoking and drinking between the non-rLDH and rLDH groups (p > 0.05). Hypertension (p = 0.025) and multilevel microdiscectomy (p = 0.014) were more common in the rLDH group than in the non-rLDH group.
In terms of the radiological factors, we did not find significant differences in the DHI, sROM, FO, FT, Pfirrmann grade, Modic changes, interdisc kyphosis rate, and large LDH rate between the non-rLDH and rLDH groups (p > 0.05). However, we found that moderate-severe MFA was more common in the rLDH group than in the non-rLDH group (p = 0.005). Additionally, the interobserver reliability of the radiological categorical factors (Pfirrmann grade, Modic changes, Large LDH, Interdisc kyphosis, MFA) are shown in Table 3. All the variables get very good interobserver reliability.
We included factors with p-values of < 0.2 (sex, age, hypertension, multilevel microdiscectomy, Modic changes, MFA) and performed univariate and multivariate logistic regression analyses (Tables 4, 5). The univariate logistic regression analysis revealed that rLDH was significantly associated with hypertension, multilevel microdiscectomy, and moderate-severe MFA. The multivariate logistic regression analysis revealed that moderate-severe MFA was the sole and strongest risk factor for rLDH (p = 0.021; odds ratio, 3.414; 95% confidence interval [CI], 1.190–8.253). In the Omnibus tests of model coefficients, p = 0.01 indicated that this multivariate logistic regression predictive model was valid. In the Hosmer-Lemeshow test, p = 0.306 indicated that the goodness of fit of this model was good. The outcome of this model indicated that after homogenization for other factors, the recurrence probability of LDH combined with moderate-severe MFA was approximately 3.414 times that of LDH combined with normal-mild MFA.
Finally, we compared the sex, age, rates of diabetes hypertension, current smoking, and drinking between the normal-mild MFA group and the moderate-severe MFA group (Table 6). We found that the age and BMI, rates of female, diabetes, hypertension, current smoking of the moderate-severe MFA group were slightly higher than those of the normal-mild MFA group. However, there was no statistical difference in these variables.
The uncertainty of rLDH is unsettling for both surgeons and patients, as reoperation may result in a worse clinical outcome or quality of life than initial surgery [12-15]. Therefore, it is necessary to establish a predictive model of rLDH for the evaluation of patient prognosis. At present, studies have found some clinical or radiological factors related to rLDH after lumbar decompressive surgery (Table 7) [17-65]. In addition to some previously studied factors, we also included some presumed related but not confirmed variables. In this study, we first explored whether current drinking, multilevel microdiscectomy, degree of MFA, interdisc kyphosis, and large LDH were associated with rLDH.
The relationships between sex, age, and rLDH have been widely studied. Most studies have not found an association between sex and rLDH [21,24,26-28,30,35]. However, Oh et al. [20] found that female sex is a risk factor for rLDH, while some studies found men to be more likely to experience recurrence than women [21-23]. Li et al. [23] and Ziegler et al. [24] found that younger age is a risk factor for rLDH. Yurac et al. [25] also found that an age of < 35 years was a risk factor for requiring revision surgery, whereas Siccoli et al. [18] found that patients aged > 35 years had rLDH earlier. Additionally, Yao et al. [26,27] and Kienzler et al. [55] both found that an age of ≥ 50 years was a risk factor for rLDH. Therefore, the correlation between rLDH and sex or age remains controversial. In this study, we found no significant differences in sex (p = 0.068) and age (p = 0.054) between the rLDH and non-rLDH groups. Therefore, the effects of sex and age on rLDH are weak in this study. Therefore, our results do not support the correlation between sex or age and rLDH.
It seems common to make a subjective link between obesity and rLDH, as a higher BMI generates a greater load on the lumbar discs. Indeed, there are also many studies confirming the association between BMI and rLDH. In most of these studies, a higher BMI was found to be a risk factor for rLDH [19,25-30,32-36], although some studies have arrived at the opposite conclusion [17]. In this study, we did not find differences in the BMI between the 2 groups. This changed our previous notion that patients with obesity are more prone to experiencing recurrence than their counterparts. The relationship between the BMI and rLDH should not be overinterpreted in terms of obesity until sufficient evidence is available. However, for patients with obesity, weight control is recommended to reduce the load on the spine.
Although diabetes has been reported as a risk factor for rLDH in previous studies [28,37,38], some studies have not found an association between diabetes and rLDH [22,31,35]. Only 1 previous study by Li et al. [28] found a correlation between hypertension and rLDH. In this study, we found that hypertension was more common in the rLDH group than in the non-rLDH group (p = 0.025), while diabetes showed no difference between the 2 groups. Nonetheless, whether patients with hypertension or diabetes have a higher recurrence rate remains controversial, as no specific biological mechanism by which hypertension or diabetes affects rLDH has been identified.
More than one previous study found smoking to be a risk factor for rLDH [19,28,38-41]. Unlike some previous studies, we did not find a significant difference in current smoking between the rLDH and non-rLDH groups (p = 0.519). The relationship between current drinking and rLDH has not been previously studied. This study did not find any correlation between current drinking habits and rLDH. The correlation between drinking and rLDH does not seem to be as significant as that with other diseases, such as femoral head necrosis or cirrhosis.
The relationship between surgical segments and rLDH has not been studied previously. Our study found that the rLDH group had a significantly higher rate of multilevel decompressive surgery than the non-rLDH group, suggesting that multilevel decompressive surgery may be associated with rLDH. A possible explanation is that more spinal stability is removed in multilevel surgery, which leads to a higher recurrence rate than that in single-level surgery.
Kim et al. [31] first reported higher DHI and sROM as risk factors for rLDH. Except for some negative reports, most studies found an association between rLDH and a higher DHI or sROM [18,22,23,28-31,42-45]. One explanation is that a higher DHI indicates more disc materials used, leading to an increased probability of rLDH. Another explanation is that a higher DHI may indicate a larger sROM, which has been found to be associated with rLDH in previous studies [30,31,45]. We did not find differences in the DHI or sROM between the 2 groups in this study. One possible reason for this is that we performed primary fusion surgery in some patients with large sROMs who were reluctant to accept any possibility of recurrence. This might have resulted in less patients with large sROM in single decompression group and ultimately lead to the nonsignificant difference in the sROM between the 2 groups.
The concepts of FO and FT were first proposed by Noren [70]. A few studies have found a relationship between FO and lumbar degenerative diseases [74]. Some studies have found that an increase in the difference in the angle of the left and right facet joints, that is, an increase in FT, may alter the normal spinal biomechanics, resulting in spinal degeneration or LDH [75-77]. However, Grogan et al. [78] found that FT is not associated with LDH. Additionally, the relationship between FO, FT, and rLDH has only been mentioned in a few studies [23,44,46]. The multicenter retrospective study by Li et al. [23] found that a higher FO and a lower FT were risk factors for rLDH. However, the retrospective matching case-control study by Shi et al. [44] did not find a correlation between rLDH and FO or FT. In this study, we did not find any differences between the rLDH and non-rLDH groups, suggesting that FO, FT, and rLDH were not correlated with each other. Therefore, we do not believe that a smaller FO or a larger FT can predict rLDH.
Whether the disc degeneration grade and Modic changes affect rLDH is still widely debated. Some studies have found that moderate disc degeneration is associated with rLDH [22,28,30,31,47], while Kim et al. [34] and Jia et al. [48] have found that more severe disc degeneration is a risk factor for rLDH. However, different studies may have used the Pfirrmann grade [68] or modified Pfirrmann grade [79] to evaluate disc degeneration, which makes some data comparisons difficult. Many studies have reported a correlation between Modic changes and rLDH [24,26,28,29,38,49,50]. However, although the rLDH group (45%) had a higher rate of Modic changes than the non-rLDH group (28.8%) in our study, the difference was not significant (p = 0.123). The probable cause is that many patients with endplate inflammation undergo primary fusion surgery because of low back pain, which may result in a potential decrease in the rate of patients with rLDH with Modic changes.
In addition to the abovementioned clinical and radiological factors, we analyzed some other common radiological factors, including interdisc kyphosis and large LDH. Contrary to our previous predictions, we found no difference in interdisc kyphosis between the 2 groups (p = 0.748). Park et al. [50] found that smaller-sized herniated discs were associated with rLDH. McGirt et al. [51,52] found that less disc removal was associated with rLDH. Although the rLDH group (10%) had a lower rate of large LDH than the non-rLDH group (22.4%) in this study, the difference was not significant (p = 0.303). This suggests that more discectomies may reduce the probability of rLDH [50-52]. However, limited discectomy has now become mainstream because aggressive discectomy may lead to intractable low back pain and lower satisfaction [51-53].
Previous studies have found a correlation between multifidus and low back pain, leg pain and even disc degeneration scale [71,80-83]. However, the relationship between the degree of MFA and rLDH has not been studied previously. In this study, we found moderate-severe MFA was the sole and strongest risk factor for rLDH. The recurrence probability of LDH combined with moderatesevere MFA was approximately 3.414 times that of LDH combined with normal-mild MFA. The multifidus is an important spinal stabilizing structure [84-88]. In patients with moderate-severe MFA, a minor surgical procedure may lead to further aggravated MFA, thereby destabilizing the spine and ultimately leading to an increased probability of recurrence. Although tubular microdiscectomy is a very minimally invasive procedure, it is still unavoidable to perform microdiscectomy through the multifidus muscle. Therefore, although minimally invasive decompressive surgery can significantly improve the pain in patients with moderate-severe MFA, the high potential recurrence probability cannot be ignored. Additionally, we do not recommend open discectomy for LDH patients as this procedure can exacerbate multifidus destruction. For patients with moderate and severe MFA, the preoperative education to the patient will become more targeted. The correct and regular back muscle exercise may be a way to lower the risk of postoperative rLDH although there is no direct evidence presently.
Although the data for this study were collected prospectively, the retrospective nature of the analysis introduced inevitable bias. The number of positive cases (rLDH) in this study was limited, which might have led to statistical bias. The recurrence of LDH is a complex biomechanical process and may be affected by many social behaviors, clinical and radiological factors, and this study was unable to incorporate all possible factors into the analysis. Additionally, many of the previously studied variables such as sex, age, BMI, diabetes, smoking or sROM, IDH, Pfirrmann’s Grade, Modic change are somewhat controversial. We can find positive or negative results for almost all variables in previous studies. Of course, these results may depend on many factors, such as the type of variables included, the type and number of cases, differences in surgical methods, and even statistical methods, etc. In addition, the herniation types, including “protrusion,” “subligamentous,” “extrusion,” and “sequestration” were not included in this study because not all surgical records contained descriptions of the specific location of disc herniation. Furthermore, this study can only provide intraobserver reliability for all radiological variables without providing interobserver reliability, as the 2 radiologists only evaluated all the radiological variables one time. This study included some possible clinical or radiological factors based on our own clinical experiences. The inclusion of factors based on clinical experience is inherently biased, although this is unavoidable in most models for risk factor prediction. Finally, this study lacks short-middle term outcomes of patients to elucidate the recovery process of postoperative low back pain and leg pain.
This study investigated the risk factors for recurrence after microdiscectomy in patients with LDH. Although there were significant differences in the rates of hypertension, multilevel microdiscectomy, and the degree of MFA between the rLDH and non-rLDH groups, we found that moderate-severe MFA was the sole and strongest risk factor of rLDH. This finding can serve as an important reference for surgeons in formulating surgical strategies and the assessment of prognosis.
NOTES
Fig. 1.
One line was drawn on the midaxial plane of the vertebra, and 2 lines were tangent to each articular process of the facet joint. The facet joint angles on axial plane were α and β. The facet orientation was defined as (α+β)/2; The facet tropism is defined as |α-β|.
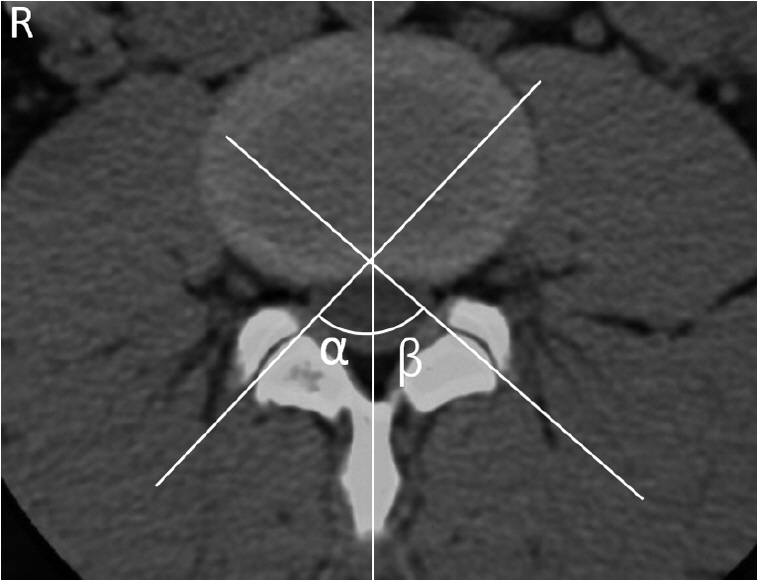
Fig. 2.
(A, B) The ratio of the area of the herniated disc (in the blue area) divided by the area of the spinal canal (in the white area) >50% was defined as large lumbar disc herniation (LDH), otherwise it was non-large LDH. (C) The ratio of the area of the multifidus fatty atrophy (MFA) (in the blue area) divided by the area of the multifidus (in the white area). (D-G) The degree of MFA was shown (normal: 0%–10% fatty infiltration, mild: 10%–30% fatty infiltration, moderate: 30%–50% fatty infiltration, severe: >50% fatty infiltration).

Fig. 3.
(A, B) Disc height index was defined as disc height divided by upper vertebral body height (b/a). (C, D) Sagittal range of motion was defined as hyperextension angle – hyperflexion angle (α-β). (E, F) α ≥0° and <0° on lateral lumbar spine x-rays were defined as interdisc lordosis and interdisc kyphosis.

Fig. 4.
(A) The surgical tapered retractor was placed during the operation. (B) The nerve root (white arrow) is compressed by the herniated disc (yellow arrow) under microscope.

Table 1.
Comparison of clinical variables between the 2 groups
Table 2.
Comparison of radiological variables between the 2 groups
Table 3.
Interobserver reliability of the radiological variables
Table 4.
Univariate logistic regression analysis of rLDH
Table 5.
Multivariate logistic regression analysis of rLDH
Table 6.
Comparison of outcomes between the normal-mild MFA and moderate-severe MFA groups
Table 7.
A review of risk or related factors of rLDH
| Study | Risk or related factors | |
|---|---|---|
| Clinical study | ||
| Carragee et al. [54] (2003) | Annular competence (massive posterior annular loss), type of herniation (extruded fragments) | |
| Kara et al. [47] (2005) | Lack of regular exercise | |
| McGirt et al. [51] (2009) | Larger annular defects, less disc removal | |
| Kim et al. [31] (2009) | Smoking, disc degeneration scale, higher DHI and sROM | |
| Meredith et al. [36] (2010) | Obesity | |
| Moliterno et al. [17] (2010) | Surgical methods (open discectomy), lower BMI | |
| Oh et al. [20] (2012) | Female, type of disc herniation (previous extruded and sequestrated disc) and traumatic events | |
| Kim et al. [56] (2013) | Surgical procedure (laminectomy) | |
| Shimia et al. [21] (2013) | Male, taller height, heavy works and being smoker | |
| Matsumoto et al. [57] (2013) | Caudally migrated LDH | |
| Kim et al. [22] (2015) | Male, a large annular defect, moderate disk degeneration, a large sROM, a small RT, a low iliac crest height index | |
| Leven et al. [35] (2015) | Younger age | |
| Miwa et al. [40] (2015) | Current smoking, occupational lifting | |
| Chang et al. [58] (2016) | Uncorrected scoliosis of young adults (< 40 years) | |
| Yao et al. [26] (2016) | Age (≥ 50 years), obesity (BMI ≥ 25 kg/m2) and Modic change | |
| Yurac et al. [25] (2016) | A subligamentous disc herniation and patient’s age < 35 years | |
| Yao et al. [27] (2017) | Older age (≥ 50 years), obesity (BMI ≥ 25 kg/m2), learning curve of the surgeon (< 200 cases) and central location of herniation | |
| Willhuber et al. [42] (2017) | Higher DHI and percentage of spinal canal, facet joint degeneration | |
| Yaman et al. [29] (2017) | Higher disc height and higher BMI, Modic changes | |
| Ikuta et al. [37] (2017) | Diabetes | |
| Belykh et al. [30] (2017) | Smoking, higher BMI, higher DHI, sROM, lower central angle of lumbar lordosis, Pfirrmann grade 3, Grogan sclerosis grades 3 and 4 | |
| Fotakopoulos et al. [32] (2018) | Higher BMI, history of injury | |
| Li et al. [23] (2018) | Male, younger age, current smoking, higher BMI, occupational lifting, trauma, surgical procedures (bilateral laminectomy or total laminectomy), herniation type (transligamentous extrusion), higher DHI, lower FO, lager FT | |
| Wu et al. [33] (2018) | Obesity | |
| Andersen et al. [41] (2018) | Smoking | |
| Lee et al. [59] (2019) | PLL tear and subarticular herniation | |
| Shin et al. [43] (2019) | Lumbosacral transitional vertebrae and a higher sROM | |
| Ziegler et al. [24] (2019) | Younger age and type 2 Modic changes | |
| Park et al. [50] (2019) | Smaller-sized herniated discs | |
| Kim et al. [34] (2019) | Higher BMI, senior degeneration scale, combined herniated nucleus pulposus, and early ambulation | |
| Li et al. [46] (2020) | Decrease of FO and increase of FT | |
| Jalil et al. [60] (2020) | Foraminal disc herniation, retrolisthesis | |
| Ding et al. [39] (2020) | Age (older), current smoking, Scheuermann disease | |
| Zhao et al. [49] (2021) | Superior endplate concave angle, sacral slope, Modic changes, sROM, extension intervertebral angle, and lumbar lordosis, DHI, retrolisthesis | |
| Siccoli et al. [18] (2021) | Older patients (> 35 years had rLDH earlier) | |
| Kienzler et al. [55] (2021) | Age ≥ 50 years and moderate disc degeneration | |
| Jia et al. [48] (2021) | The course of disease, Pfirrmann grade, Modic change, and migration grade | |
| Li et al. [28] (2021) | Hypertension, diabetes, a history of smoking, a history of performing intense physical labor, Pfirrmann grade 3, Modic changes (type 2), herniation in the form of extrusion, a higher DHI and rROM | |
| Shi et al. [44] (2021) | Lower grade of surgical-level disc degeneration, senior grade of adjacent-level disc degeneration, a high DHI, and a large sROM | |
| Siccoli et al. [19] (2022) | Overweight and smoking | |
| Ono et al. [38] (2022) | Lower disc height, smoking, diabetes, subligamentous extrusion type, and Modic change | |
| Review and meta-analysis | ||
| McGirt et al. [52] (2009) | Limited disc removal | |
| Watters 3rd et al. [53] (2009) | Conservative discectomy | |
| Shin [61] (2014) | Diabetes, family history, history of external injury, duration of illness and BMI | |
| Huang et al. [62] (2016) | Smoking, disc protrusion, and diabetes | |
| Hlubek et al. [63] (2017) | Younger age, lack of a sensory or motor deficit, and a higher baseline ODI | |
| Yin et al. [64] (2018) | Older age (≥ 50 years), obesity (BMI ≥ 25 kg/m2), upper lumbar disc and central disc herniation | |
| Miller et al. [65] (2018) | Larger annular defect | |
| Brooks et al. [45] (2020) | Higher DHI and sROM, Modic changes | |
DHI, disc height index; sROM, sagittal range of motion; BMI, body mass index; PLL, posterior longitudinal ligament; LDH, lumbar disc herniation; IHI, iliac crest height index; RT, relative thickness of the transverse process of L5 vertebra; FO, facet orientation; FT, facet tropism; rLDH, recurrent lumbar disc herniation; ODI, Oswestry Disability Index.
REFERENCES
1. Ravindra VM, Senglaub SS, Rattani A, et al. Degenerative lumbar spine disease: estimating global incidence and worldwide volume. Global Spine J 2018;8:784-94.




2. Stafford MA, Peng P, Hill DA. Sciatica: a review of history, epidemiology, pathogenesis, and the role of epidural steroid injection in management. Br J Anaesth 2007;99:461-73.


4. Riihimäki H, Tola S, Videman T, et al. Low-back pain and occupation. A cross-sectional questionnaire study of men in machine operating, dynamic physical work, and sedentary work. Spine (Phila Pa 1976) 1989;14:204-9.

5. Miranda H, Viikari-Juntura E, Martikainen R, et al. Individual factors, occupational loading, and physical exercise as predictors of sciatic pain. Spine (Phila Pa 1976) 2002;27:1102-9.


6. Sørensen IG, Jacobsen P, Gyntelberg F, et al. Occupational and other predictors of herniated lumbar disc disease-a 33-year follow-up in the Copenhagen male study. Spine (Phila Pa 1976) 2011;36:1541-6.


7. Vialle LR, Vialle EN, Suarez Henao JE, et al. Lumbar disc herniation. Rev Bras Ortop 2015;45:17-22.



8. Kreiner DS, Hwang SW, Easa JE, et al. An evidence-based clinical guideline for the diagnosis and treatment of lumbar disc herniation with radiculopathy. Spine J 2014;14:180-91.


10. Suk KS, Lee HM, Moon SH, et al. Recurrent lumbar disc herniation: results of operative management. Spine (Phila Pa 1976) 2001;26:672-6.

11. Ahn J, Tabaraee E, Bohl DD, et al. Primary versus revision single-level minimally invasive lumbar discectomy: analysis of clinical outcomes and narcotic utilization. Spine (Phila Pa 1976) 2015;40:E1025-30.

12. Inada T, Nishida S, Kawaoka T, et al. Analysis of revision surgery of microsurgical lumbar discectomy. Asian Spine J 2018;12:140-6.




13. Mehren C, Wanke-Jellinek L, Korge A. Revision after failed discectomy. Eur Spine J 2020;29:14-21.


14. Fritzell P, Knutsson B, Sanden B, et al. Recurrent versus primary lumbar disc herniation surgery: patient-reported outcomes in the Swedish Spine Register Swespine. Clin Orthop Relat Res 2015;473:1978-84.


15. Lubelski D, Senol N, Silverstein MP, et al. Quality of life outcomes after revision lumbar discectomy. J Neurosurg Spine 2015;22:173-8.


16. Kapetanakis S, Gkantsinikoudis N, Charitoudis G. The Role of full-endoscopic lumbar discectomy in surgical treatment of recurrent lumbar disc herniation: a health-related quality of life approach. Neurospine 2019;16:96-104.




17. Moliterno JA, Knopman J, Parikh K, et al. Results and risk factors for recurrence following single-level tubular lumbar microdiscectomy. J Neurosurg Spine 2010;12:680-6.


18. Siccoli A, Schröder ML, Staartjes VE. Association of age with incidence and timing of recurrence after microdiscectomy for lumbar disc herniation. Eur Spine J 2021;30:893-8.



19. Siccoli A, Staartjes VE, Klukowska AM, et al. Overweight and smoking promote recurrent lumbar disk herniation after discectomy. Eur Spine J 2022;31:604-13.



20. Oh JT, Park KS, Jung SS. Surgical results and risk factors for recurrence of lumbar disc herniation. Korean J Spine 2012;9:170-5.



21. Shimia M, Babaei-Ghazani A, Sadat BE, et al. Risk factors of recurrent lumbar disk herniation. Asian J Neurosurg 2013;8:93-6.



22. Kim KT, Lee DH, Cho DC, et al. Preoperative risk factors for recurrent lumbar disk herniation in L5-S1. J Spinal Disord Tech 2015;28:E571-7.


23. Li Z, Yang H, Liu M, et al. Clinical characteristics and risk factors of recurrent lumbar disk herniation: a retrospective analysis of three hundred twenty-one cases. Spine (Phila Pa 1976) 2018;43:1463-9.

24. Ziegler DS, Carreon L, Andersen MO, et al. The association between preoperative MRI findings and surgical revision within three years after surgery for lumbar disc herniation. Spine (Phila Pa 1976) 2019;44:818-25.


25. Yurac R, Zamorano JJ, Lira F, et al. Risk factors for the need of surgical treatment of a first recurrent lumbar disc herniation. Eur Spine J 2016;25:1403-8.



26. Yao Y, Liu H, Zhang H, et al. Risk factors for the recurrent herniation after microendoscopic discectomy. World Neurosurg 2016;95:451-5.


27. Yao Y, Liu H, Zhang H, et al. Risk factors for recurrent herniation after percutaneous endoscopic lumbar discectomy. World Neurosurg 2017;100:1-6.


28. Li Y, Wang B, Li H, et al. Adjuvant surgical decision-making system for lumbar intervertebral disc herniation after percutaneous endoscopic lumber discectomy: a retrospective nonlinear multiple logistic regression prediction model based on a large sample. Spine J 2021;21:2035-48.


29. Yaman ME, Kazancı A, Yaman ND, et al. Factors that influence recurrent lumbar disc herniation. Hong Kong Med J 2017;23:258-63.


30. Belykh E, Krutko AV, Baykov ES, et al. Preoperative estimation of disc herniation recurrence after microdiscectomy: predictive value of a multivariate model based on radiographic parameters. Spine J 2017;17:390-400.


31. Kim KT, Park SW, Kim YB. Disc height and segmental motion as risk factors for recurrent lumbar disc herniation. Spine (Phila Pa 1976) 2009;34:2674-8.


32. Fotakopoulos G, Makris D, Kotlia P, et al. Recurrence is associated with body mass index in patients undergoing a single-level lumbar disc herniation surgery. J Clin Med Res 2018;10:486-92.



33. Wu J, Zhang C, Lu K, et al. Percutaneous endoscopic lumbar reoperation for recurrent sciatica symptoms: a retrospective analysis of outcomes and prognostic factors in 94 patients. World Neurosurg 2018;109:e761-9.


34. Kim HS, You JD, Ju CIl. Predictive scoring and risk factors of early recurrence after percutaneous endoscopic lumbar discectomy. Biomed Res Int 2019;2019:6492675.




35. Leven D, Passias PG, Errico TJ, et al. Risk factors for reoperation in patients treated surgically for intervertebral disc herniation: a subanalysis of eight-year SPORT data. J Bone Joint Surg Am 2015;97:1316-25.


36. Meredith DS, Huang RC, Nguyen J, et al. Obesity increases the risk of recurrent herniated nucleus pulposus after lumbar microdiscectomy. Spine J 2010;10:575-80.


37. Ikuta K, Tarukado K, Masuda K. Characterization and risk factor analysis for recurrence following microendoscopic diskectomy for lumbar disk herniation. J Neurol Surg A Cent Eur Neurosurg 2017;78:154-60.


38. Ono K, Ohmori K, Yoneyama R, et al. Risk factors and surgical management of recurrent herniation after full-endoscopic lumbar discectomy using interlaminar approach. J Clin Med 2022;29 11:748.



39. Ding Y, Lv S, Li G, et al. Scheuermann’s disease as a risk factor for lumbar disc herniation recurrence. J Coll Physicians Surg Pak 2020;30:584-9.


40. Miwa S, Yokogawa A, Kobayashi T, et al. Risk factors of recurrent lumbar disk herniation: a single center study and review of the literature. J Spinal Disord Tech 2015;28:E265-9.

41. Andersen SB, Smith EC, Støttrup C, et al. Smoking is an independent risk factor of reoperation due to recurrent lumbar disc herniation. Global Spine J 2018;8:378-81.



42. Willhuber GC, Kido G, Mereles M, et al. Factors associated with lumbar disc hernia recurrence after microdiscectomy. Rev Esp Cir Ortop Traumatol 2017;61:397-403.


43. Shin EH, Cho KJ, Kim YT, et al. Risk factors for recurrent lumbar disc herniation after discectomy. Int Orthop 2019;43:963-7.



44. Shi H, Zhu L, Jiang ZL, et al. Radiological risk factors for recurrent lumbar disc herniation after percutaneous transforaminal endoscopic discectomy: a retrospective matched case-control study. Eur Spine J 2021;30:886-92.



45. Brooks M, Dower A, Jalil MF, et al. Radiological predictors of recurrent lumbar disc herniation: a systematic review and meta-analysis. J Neurosurg Spine 2020;27:1-11.

46. Li Z, Gui G, Zhang Y, et al. Are facet joint parameters risk factors for recurrent lumbar disc herniation? A pilot study in a Chinese population. J Clin Neurosci 2020;77:36-40.


47. Kara B, Tulum Z, Acar U. Functional results and the risk factors of reoperations after lumbar disc surgery. Eur Spine J 2005;14:43-8.



48. Jia M, Sheng Y, Chen G, et al. Development and validation of a nomogram predicting the risk of recurrent lumbar disk herniation within 6 months after percutaneous endoscopic lumbar discectomy. J Orthop Surg Res 2021;16:274.




49. Zhao C, Zhang H, Wang Y, et al. Nomograms for predicting recurrent herniation in PETD with preoperative radiological factors. J Pain Res 2021;14:2095-109.




50. Park CH, Park ES, Lee SH, et al. Risk factors for early recurrence after transforaminal endoscopic lumbar disc decompression. Pain Physician 2019;22:E133-8.


51. McGirt MJ, Ambrossi GL, Datoo G, et al. A prospective cohort study of close interval computed tomography and magnetic resonance imaging after primary lumbar discectomy: factors associated with recurrent disc herniation and disc height loss. Spine (Phila Pa 1976) 2009;34:2044-51.

52. McGirt MJ, Ambrossi GL, Datoo G, et al. Recurrent disc herniation and long-term back pain after primary lumbar discectomy: review of outcomes reported for limited versus aggressive disc removal. Neurosurgery 2009;64:338-44.

53. Watters WC 3rd, McGirt MJ. An evidence-based review of the literature on the consequences of conservative versus aggressive discectomy for the treatment of primary disc herniation with radiculopathy. Spine J 2009;9:240-57.


54. Carragee EJ, Han MY, Suen PW, et al. Clinical outcomes after lumbar discectomy for sciatica: the effects of fragment type and anular competence. J Bone Joint Surg Am 2003;85:102-8.

55. Kienzler JC, Fandino J, Kelft EV, et al. Risk factors for early reherniation after lumbar discectomy with or without annular closure: results of a multicenter randomized controlled study. Acta Neurochir (Wien) 2021;163:259-68.



56. Kim CH, Chung CK, Park CS, et al. Reoperation rate after surgery for lumbar herniated intervertebral disc disease: nationwide cohort study. Spine (Phila Pa 1976) 2013;38:581-90.

57. Matsumoto M, Watanabe K, Hosogane N, et al. Recurrence of lumbar disc herniation after microendoscopic discectomy. J Neurol Surg A Cent Eur Neurosurg 2013;74:222-7.


58. Chang HK, Chang HC, Wu JC, et al. Scoliosis may increase the risk of recurrence of lumbar disc herniation after microdiscectomy. J Neurosurg Spine 2016;24:586-91.


59. Lee JH, Choi KC, Lee JH. Could the splitting of the annulus during percutaneous endoscopic lumbar diskectomy (PELD) be a culprit for recurrent disk herniation?: an analysis of the reherniation pattern after PELD. World Neurosurg 2019;132:e623-9.


60. Jalil MF, Dower A, Tawfik S, et al. MRI predictors of revision surgery after primary lumbar discectomy. J Clin Neurosci 2020;81:442-6.


62. Huang W, Han Z, Liu J, et al. Risk factors for recurrent lumbar disc herniation: a systematic review and meta-analysis. Medicine (Baltimore) 2016;95:e2378.


63. Hlubek RJ, Mundis GM Jr. Treatment for recurrent lumbar disc herniation. Curr Rev Musculoskelet Med 2017;10:517-20.




64. Yin S, Du H, Yang W, et al. Prevalence of recurrent herniation following percutaneous endoscopic lumbar discectomy: a meta-analysis. Pain Physician 2018;21:337-50.

65. Miller LE, McGirt MJ, Garfin SR, et al. Association of annular defect width after lumbar discectomy with risk of symptom recurrence and reoperation: systematic review and meta-analysis of comparative studies. Spine (Phila Pa 1976) 2018;43:E308-15.

66. Chapman JR, Norvell DC, Hermsmeyer JT, et al. Evaluating common outcomes for measuring treatment success for chronic low back pain. Spine (Phila Pa 1976) 2011;36:S54-68.


68. Pfirrmann’s CW, Metzdorf A, Zanetti M, et al. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976) 2001;6:1873-8.
69. Modic MT, Steinberg PM, Ross JS, et al. Degenerative disk disease: assessment of changes in vertebral body marrow with MR imaging. Radiology 1988;166:193-9.


70. Noren R, Trafimow J, Andersson GB, et al. The role of facet joint tropism and facet angle in disc degeneration. Spine (Phila Pa 1976) 1991;16:530-2.


71. Kader DF, Wardlaw D, Smith FW. Correlation between the MRI changes in the lumbar multifidus muscles and leg pain. Clin Radiol 2000;55:145-9.


72. Zhang Y, Chong F, Feng C, et al. Comparison of endoscopeassisted and microscope-assisted tubular surgery for lumbar laminectomies and discectomies: minimum 2-year follow-up results. Biomed Res Int 2019;2019:5321580.




73. Zhu F, Zhang Y, Peng Y, et al. A novel classification based on magnetic resonance imaging for individualized surgical strategies of lumbar disc herniation. Arch Orthop Trauma Surg 2023 Feb 14 doi: 10.1007/s00402-023-04810-4. [Epub].


74. Boden SD, Riew KD, Yamaguchi K, et al. Orientation of the lumbar facet joints: association with degenerative disc disease. J Bone Joint Surg Am 1996;78:403-11.

75. Ishihara H, Matsui H, Osada R, et al. Facet joint asymmetry as a radiologic feature of lumbar intervertebral disc herniation in children and adolescents. Spine (Phila Pa 1976) 1997;22:2001-4.


76. Chadha M, Sharma G, Arora SS, et al. Association of facet tropism with lumbar disc herniation. Eur Spine J 2013;22:1045-52.



77. Karacan I, Aydin T, Sahin Z, et al. Facet angles in lumbar disc herniation: their relation to anthropometric features. Spine (Phila Pa 1976) 2004;29:1132-6.


78. Grogan J, Nowicki BH, Schmidt TA, et al. Lumbar facet joint tropism does not accelerate degeneration of the facet joints. AJNR Am J Neuroradiol 1997;18:1325-9.


79. Griffith JF, Wang YX, Antonio GE, et al. Modified Pfirrmann’s grading system for lumbar intervertebral disc degeneration. Spine (Phila Pa 1976) 2007;32:E708-12.

80. Goubert D, Pauw RD, Meeus M, et al. Lumbar muscle structure and function in chronic versus recurrent low back pain: a cross-sectional study. Spine J 2017;17:1285-96.


81. Seyedhoseinpoor T, Taghipour M, Dadgoo M, et al. Alteration of lumbar muscle morphology and composition in relation to low back pain: a systematic review and meta-analysis. Spine J 2022;22:660-76.


82. Storheim K, Berg L, Hellum C, et al. Fat in the lumbar multifidus muscles - predictive value and change following disc prosthesis surgery and multidisciplinary rehabilitation in patients with chronic low back pain and degenerative disc: 2-year follow-up of a randomized trial. BMC Musculoskelet Disord 2021;18:145.


83. Zotti MGT, Boas FV, Clifton T, et al. Does pre-operative magnetic resonance imaging of the lumbar multifidus muscle predict clinical outcomes following lumbar spinal decompression for symptomatic spinal stenosis? Eur Spine J 2017;26:2589-97.



84. Wilke HJ, Wolf S, Claes LE, et al. Stability increase of the lumbar spine with different muscle groups. A biomechanical in vitro study. Spine (Phila Pa 1976) 1995;20:192-8.

85. Ward SR, Tomiya A, Regev GJ, et al. Passive mechanical properties of the lumbar multifidus muscle support its role as a stabilizer. J Biomech 2009;42:1384-9.



86. Ward SR, Kim CW, Eng CM, et al. Architectural analysis and intraoperative measurements demonstrate the unique design of the multifidus muscle for lumbar spine stability. J Bone Joint Surg Am 2009;91:176-85.




































