- Search
Abstract
Intraosseous pneumatocyst is a benign, gas-filled, cystic lesion, and is commonly encountered in iliac bone or sacrum. Other locations of this lesion following trauma are rare, and only a handful of isolated cases have been reported. The pathogenesis and etiologies of this uncommon entity are various and it can present a diagnostic challenge. Only four previous cases have described the natural course of intravertebral pneumatocysts. Here, the authors report a rare case of traumatic pneumatocyst, which resolved rapidly without further complication. Possible pathogenic mechanisms are discussed and reviews of literatures are included.
Intraosseous gas collection is observed in various pathologic conditions, including osteomyelitis by gas-forming organisms, vertebral collapse due to osteonecrosis, neoplasms, and post-traumatic conditions2,3,11). Intraosseous pneumatocysts are frequently observed in the ilium or sacrum adjacent to the sacroiliac joint. However, intraosseous pneumatocysts, involving a gas-filled cystic lesion of uncertain origin in bone, are relatively rare, and traumatic pneumatocysts in the cervical spine are extremely rare3,4). In fact, only four cases have described the natural course of this rare entity, which remains unclear6,8,10).
Here, we report a unique case of traumatic pneumatocyst in the cervical spine that exhibited spontaneous, rapid resolution, and include reviews of literatures.
A 54-year-old man with severe neck pain was referred to our emergency room following a high-speed motorcycle accident. The patient had no previous history of anticoagulant therapy or hematological coagulopathy, and was in good health before this episode. On physical examination, he was alert and fully oriented. No neurologic abnormalities were found for cranial nerves or the cerebellar system. Brain computed tomography (CT) revealed no evidence of any abnormality. However, lamina fractures of C6 and C7 and an irregular lesion of around 10├Ś10├Ś10mm filled with gas in the C6 vertebral body were visualized by CT (Fig. 1). The lesion did not communicate with the spinal canal or intervertebral disc. Conservative treatment including bed rest, O2 inhalation, and medication for pain relief was administered. A follow-up CT scan taken 3 days after injury revealed that the intravertebral gas had completely resolved with no further complication (Fig. 2). The patient remained in good health and was free of neurological deficits during the 3-month follow-up period.
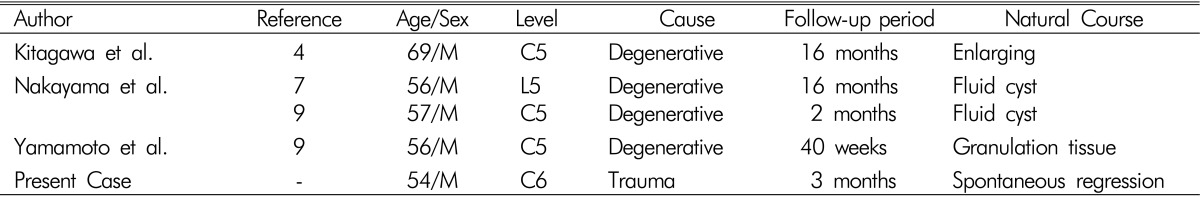
Intraosseous pneumatocyst is a rare condition in which a gas-filled cystic lesion of uncertain origin occupies bone2). However, they are rarely detected in vertebral bodies, and to our knowledge, only few cases have been reported in the body of cervical vertebrae, and most of these cases occurred in the setting of spondylosis (Table 1)5,6,7,9). Although percutaneous injection of bone graft substitute material for treatment of a symptomatic pneumatocysts was reported as a treatment option, they are nearly always treated conservatively1). Several authors have stated that the sizes of pneumatocysts remain stable based on radiological examinations. However, Nakayama et al.8) reported two pneumatocysts, one in the cervical spine and the other in the lumbar spine, that spontaneously progressed to fluid-filled cysts, 6-16 months after initial presentation. Yamamoto et al.10) reported a cervical pneumatocyst that changed to a fluid-filled cyst and that was subsequently replaced by granulation tissue, as shown by magnetic resonance imaging at 40-weeks, and Kitagawa et al.6) reported the first enlarging pneumatocyst as determined by 16-month follow-up. To the best of our knowledge, our case of a traumatic pneumatocyst in the C6 vertebral body is the first to shown rapid resolution by 3 day follow-up CT. Although the etiology of cervical pneumatocyst is unclear, except for those associated with pathological conditions, a number of authors have hypothesized about its origins and natural courses. The gas inside a pneumatocyst is primarily nitrogen, and some authors have suggested that negative pressure within the lesion (due to some unknown mechanism) causes the release of nitrogen from surrounding soft tissues or articular joints8,9). Gas in degenerated intervertebral discs, known as the "vacuum phenomenon", is often observed in the degenerated spine, and extension of gas from an intervertebral disc into a vertebral body through a defect in a degenerated endplate could possibly cause an intravertebral pneumatocyst9). Furthermore, the radiolucent and osteolytic images of pneumatocysts in plain radiographs may mimic metastatic lesions. CT is the most useful radiological tool for the correct diagnosis of pneumatocysts, which exhibit no contrast enhancement on CT images. Traumatic intravertebral pneumatocysts are benign innocuous lesions that need to be differentiated from other gas-containing lesions of the spine, including those caused by osteomyelitis, osteonecrosis, or neoplasms.
References
1. Formby PM, Kang DG, Potter BK, Forsberg JA. Treatment of symptomatic intraosseous pneumatocyst using intraoperative navigation. Orthopedics 2015 38:e244-e247. PMID: 25760515.


2. Grunshaw ND, Carey BM. Case report: gas within a cervical vertebral body. Clin Radiol 1994 49:653-654. PMID: 7955897.


3. Hall FM, Turkel D. Case report 536: Intraosseous pneumocyst of the ilium. Skeletal Radiol 1989 18:127-128. PMID: 2717951.


4. Karadick D, Eason MA. Vertebral pneumatocyst mimicking susceptibility artifact on MR imaging. AJR Am J Roentgenol 1998 170:221PMID: 9423641.


5. Kim CH. Pneumorrhachis and paraspinal air with vacumn disc: case report and literature review. J Korean Neurosurg Soc 2007 42:490-491. PMID: 19096597.



6. Kitagawa T, Fujiwara A, Tamai K, Kobayashi N, Saiki K, Omata S, et al. Enlarging vertebral body pneumatocysts in the cervical spine. AJNR 2003 24:1707-1710. PMID: 13679296.


7. Larsen JL, Smievoll AI. Gas in a cervical vertebral body. A case report with CT confirmation. Eur J Radiol 1988 8:98-99. PMID: 3383864.

8. Nakayama T, Ehara S, Hama H. Spontaneous progression of vertebral intraosseous pneumatocysts to fluid-filled cysts. Skeletal Radiol 2001 30:523-526. PMID: 11587521.


9. Sunder S, Prasad R. Vertebral body pneumatocysts in the cervical spine - A case report. Apollo Medicine 2008 5:121-124.

10. Yamamoto T, Yoshiya S, Kurosaka M, Nagira K, Takabatake M, Hamamoto H, et al. Natural course of an intraosseous pneumatocyst of the cervical spine. AJR Am J Roentgenol 2002 179:667-669. PMID: 12185040.


11. Yun SM, Suh BS, Park JS. Symptomatic epidural gas-containing cyst from intervertebral vacuum phenomenon. Korean J Spine 2012 9:365-368. PMID: 25983848.




- TOOLS
-
METRICS

-
- 1 Crossref
- Scopus
- 8,298 View
- 69 Download
-
Journal Impact Factor 3.8
SURGERY: Q1
CLINICAL NEUROLOGY: Q1
- Related articles in NS
-
The Art of Diagnosis in the Cervical Spine2020 December;17(4)
Sudden Paraplegia Caused by Nontraumatic Cervical Disc Rupture: A Case Report2017 December;14(4)
Spontaneous Resolution of Spinal Epidural Hematoma: A Case Report.2008 June;5(2)
Atypical Presentation of Cervical 3-4 Disc Herniation - A Case Report -2007 June;4(2)
Metastatic Mixed Germ Cell Tumor at the Intramedullary Cervical Spine -A Case Report-2007 June;4(2)