 |
 |
- Search
|
|
||
See commentary "Commentary on “Selection of Optimal Lower Instrumented Vertebra for Adolescent Idiopathic Scoliosis Surgery”" in Volume 20 on page 808.
Abstract
Adolescent idiopathic scoliosis (AIS) affects approximately 2% of adolescents across all ethnicities. The objectives of surgery for AIS are to halt curve progression, correct the deformity in 3 dimensions, and preserve as many mobile spinal segments as possible, avoiding junctional complications. Despite ongoing development in algorithms and classification systems for the surgical treatment of AIS, there is still considerable debate about selecting the appropriate fusion level. In this study, we review the literature on fusion selection and present current concepts regarding the lower instrumented vertebra in the selection of the fusion level for AIS surgery.
Adolescent idiopathic scoliosis (AIS) affects 1%–3% of children in the at-risk population of those aged 10–16 years [1]. Surgical intervention for AIS is usually recommended for patients whose curves progress despite nonoperative management [2,3]. The main objectives of the surgical treatment of AIS are to achieve coronal and sagittal balance, preserve motion segments, and avoid complications such as coronal decompensation, curve progression, junctional kyphosis, the adding-on (AO) phenomenon, and revision surgery [4-7]. The selection of the fusion level is the single most important factor influencing the result of AIS surgery [8]. Inappropriately selecting the extent of fusion can result in undercorrection or overcorrection of the main and compensatory curves, which may lead to a failure to stabilize the index curve [9-11]. Moreover, it may exacerbate unfused curves and cause trunk imbalance and decompensation [8,12].
There has been considerable debate about the appropriate fusion-level selection for AIS. Selecting the appropriate lower instrumented vertebra (LIV) is essential for avoiding distal junctional problems such as distal junctional kyphosis (DJK) and AO [13]. Before the development of the Harrington rod in the late 1950s, based on the reports of Hibbs et al. [14,15], the lower end vertebra (LEV) with neutral rotation was recommended as the ideal LIV to prevent AO. Starting with these reports, various LIV selection methods have been studied. In this review, we discuss how LIV selection has developed historically and describe up-to-date concepts regarding optimal LIV selection in AIS surgery.
The traditional fusion level, recommended by Harrington et al. [16,17] and called the Harrington Stable Zone, was to fuse 1 vertebra above and 2 below the endpoints of the Cobb measurement, with instrumentation in the stable zone based on bending, traction, and intraoperative radiographs. The first treatment-based AIS classification system was developed in 1983 by King et al. [8]. This system, based on the extensive experience of Dr. John Moe in the surgical treatment of AIS patients with Harrington rod instrumentation, divides curves into 5 types and gives guidelines and recommendations for which levels should be instrumented according to these types in order to preserve as much motion as possible [18]. However, this system is limited because it is only based on the coronal plane, lacks a defined isolated thoracolumbar curve type, and has relatively poor to fair inter- and intraobserver reliability [19].
To overcome the limitations of King-Moe classification, Lenke et al. [19] introduced a classification system redefining how arthrodesis levels are selected. The classification combines 6 coronal curve types (1 through 6), with 3 lumbar modifiers (A, B, or C) and 3 sagittal thoracic modifiers (minus, normal, or plus). It requires not only standing coronal and lateral full spine radiographs, but also supine side-bending films. The spinal column regions evaluated in this classification are proximal thoracic, main thoracic, and thoracolumbar (TL/L). The authors recommended that the major curve, namely the curve with the largest Cobb angle, should always be included in the fusion extent. If the curve is regarded as nonstructural (corrects to < 25° as measured on side-bending radiographs and/or with kyphosis of <20° between T2–5 and T10–L2), it does not have to be included in the fusion.
However, even with a better classification of AIS, the selection of fusion levels remains highly variable and is a hot topic in spinal deformity research [8,19-23]. The selection of the LIV has been a matter of debate, and the optimal positioning is often difficult to identify or predict [20]. To date, numerous studies have been conducted to identify the optimal LIV for AIS surgery. Suk et al. [24] have suggested that the LIV should be selected based on the relative position of the neutral vertebra (NV). They recommended selecting the NV when it is either the same as or 1 level distal to the LEV of the main curve, and NV-1 if more than 2 levels separate the LEV from the NV. Nonetheless, due to its low inter- and intraobserver reliability, the application of the NV for selecting the optimal LIV shows limitations [25]. Parisini et al. [26] investigated the rotation of the lumbar vertebra just below the LEV as an important factor, like the position of the stable vertebra (SV), for selecting fusion levels in single thoracic curves in which the lumbar compensatory curve did not cross the midline. If the rotation of the first vertebra just below the LEV is in the same direction as the thoracic curve, and if the SV and LEV show a difference of more than 2 levels, then L2 or L3 is recommended as the LIV. However, if the rotation of the first vertebra just below the LEV is in the opposite direction, and if the SV and LEV show a difference of no more than 2 levels, then the LIV can be selected 2 or 3 levels below the SV. Wang et al. [27] reported that the selection of the LIV correlated strongly to the presence of distal AO in Lenke 1A curves and stated that the best outcomes resulted from choosing as the LIV the first vertebra in the cephalad direction from the sacrum whose deviation from the central sacral vertebral line (CSVL) was more than 10 mm. Their reasoning was that this method might not only prevent distal AO, but also preserve more lumbar motion and growth potential. Sarlak and colleagues argued that the tilt of L3 and L4 in the coronal plane may play a significant role in determining the distal fusion level in Lenke 1A curves [7,28]. They recommended that the distal fusion level should be extended to at least LEV-1 in Lenke 1A curves with L3 as NV, while it might be necessary to go down to the LEV with L3 vertebral tilt [28]. However, choosing the appropriate LIV for major thoracic curves with lumbar type C is still debatable. Takahashi et al. [5] focused on choosing fusion levels for selective thoracic fusion of AIS with specific Lenke types [7]. The authors identified 3 curve patterns according to the relative positions of the SV and LEV in Lenke 1B, 1C, or 3C curves. They recommended choosing the LIV 1 level distal to the SV/LEV when the SV and LEV are the same, in order to achieve the greatest correction of thoracic and lumbar curves as well as trunk shift, and choosing the LIV as either the SV or at least 1 level distal to it if the SV is below the LEV.
Recent studies have investigated the last touched vertebra (LTV) to assist in determining the LIV [20,29]. The LTV is the most cephalad TL/L vertebra (T12–L5) of the lowest structural curve that is touched by CSVL. Matsumoto et al. [29] investigated the occurrence of postoperative AO and related factors in Lenke 1A curves. They suggested that the LIV should be extended to or beyond the LTV to avoid the development of postoperative AO. Lenke et al. [30] reported that selecting the LTV as the LIV for Lenke 1A curves produced acceptable radiographic results at a minimum 5-year follow-up. Fischer et al. [13], who evaluated the optimal LIV on the basis of rotation or the CSVL, proposed using either the LTV or a vertebra within 2 levels proximal to the NV as the LIV.
However, in clinical practice, if the CSVL touches the LTV slightly, choosing the proper LIV can be challenging. Qin et al. [31] proposed the concept of the last substantially touched vertebra (LSTV), defined as the vertebra nearest where the CSVL either intersects the pedicle outline or is medial to the pedicle outline. Shen and colleagues argued that both the SV and LSTV could be relevant for LIV and showed favorable outcomes in the management of Lenke 1A curves [32]. Cho et al. [20] reported that Lenke 1A-R curves (L4 vertebral tilt to the right) were 2.2 times more likely to experience AO than 1A-L (L4 vertebral tilt to the left) curves and recommended selecting the LSTV as the LIV for Lenke 1A-R. Qin et al. [33] asserted that Lenke type 2 curves could be categorized analogously into 2A-R (L4 vertebral tilt to the right) and 2A-L (L4 vertebral tilt to the left). They proposed that to avoid distal AO, the LIV should be extended to LSTV (usually located upper or mid lumbar area) for 2A-R, and to LSTV+1 (usually located in the TL junction area) for 2A-L.
For AIS patients with a major TL/L curve, the spine surgeon’s goal is to apply a shorter fusion strategy that preserves distal motion segments maximally while minimizing the risks of lower back pain and long-term disc degeneration in the lower fusion segment. According to earlier investigations, no clinical or radiological difference was observed in relation to the distal fusion level (L3 vs. L4, LEV vs. LEV+1) [34,35]. However, recent long-term follow-up studies comparing L3 LIV to L4 LIV demonstrated that the latter led to worse experiences of back pain than the former [36,37]. Additionally, a ≥ 40-year follow-up study revealed that patients with spines fused to L4 were more likely to undergo an additional surgical procedure than those fused to L3 [38].
Therefore, in order to achieve a better long-term prognosis, it is still believed that the preservation of one additional distal segment may be necessary. In 2014, Kim et al. [39], who analyzed 66 patients with TL/L AIS, concluded that L3 could serve as the LIV when preoperative L3 crosses the midsacral line with less than grade II rotation on bending-posture radiographs, although other patients fused to L4 also showed favorable outcomes. Chang et al. [40] distinguished the LIV selection of TL/L AIS depending on the flexibility of the TL curve in a subsequent study. The LIV should be set to L3 (LEV) if the curve is flexible (L3 crosses the CSVL with rotation of grade II), whereas LIV should be set to L4 (LEV+1) if the curve is rigid (L3 does not cross the CSVL or the rotation exceeds grade II). Lee et al. [41] argued that the LTV is a significant element in determining the appropriate correction rate and development of adjacent disc wedging. They suggested that if LEV≥ L3 and LTV≥ L4, distal fusion at L3 could be feasible for preserving the lumbar motion segments. Therefore, caution is required when choosing the distal fusion level if LEV≤ L4 and LTV= L5. The results of studies on LIV selection in AIS are summarized in Table 1.
Because there are several methods for selecting the optimal LIV, no consensus has been reached. However, spinal fusion should affect as short a segment as possible to preserve distal mobility. Several recent studies have been conducted on LIV selection using positional radiographs.
Kim et al. [42] pointed out that the LTV on a preoperative supine radiograph can be an optimal LIV in most types of AIS surgery to maximize mobility. Radiographs are easy to take while a patient is supine, which resembles the intraoperative posture, because spinal curves are reduced to a more relaxed state without a meaningful impact from gravity and the patient’s body weight. The study included consecutive patients who underwent corrective surgery for AIS. The Scoliosis Research Society (SRS)-22 questionnaire and postoperative serial standing radiographs were utilized to evaluate clinical and radiographic outcomes. The patients were classified into 4 groups according to the relationship of the locations of the LIV, LTV, and LSTV on upright radiographs and the LTV on supine radiographs. In group 1, the upright LTV and supine LTV were the same. Group 1 was subdivided into group 1A and group 1B according to whether the LTV and LSTV differed or were the same, respectively. In group 2, the upright LTV was selected as the LIV, whereas in group 3, the supine LTV was selected. The demographic data showed that there were no significant differences among groups in terms of age, sex, body mass index, preoperative Cobb angle, or Lenke classification. The surgical data showed no significant differences among groups in terms of operative time or estimated blood loss. The clinical outcomes evaluated by the SRS-22 questionnaire showed no significant differences among groups in pain, self-image, mental health, function, or satisfaction scores. Furthermore, poor radiographic outcomes (such as AO, DJK, and proximal junctional kyphosis) were not significantly different at follow-up intervals for each group. The authors concluded that selecting the supine LTV in AIS correction surgery could offer an optimal LIV for most Lenke curves, while maximally preserving motion segments and being simple to apply (Fig. 1).
Similarly, Sarwahi et al. [43] investigated whether conducting fusion to the touched vertebra on prone radiographs with minimal rotation (grade 0 or I) would allow shorter fusion with optimal correction. In the study, patients with minimal rotation in their LTV were selected using prone or standing radiographs. Patients who were fused to a rotated LTV on standing or prone radiographs were categorized as touched vertebra rotated (TVR), while those in the non-TV (NTV) group had the LIV fused proximal to the LTV. The risk of AO was determined based on ≥ 5° of disk wedging. The study compared patients in 2 groups: group A consisted of patients fused to minimally rotated LTV (selected from prone and standing radiographs), and group B included TVR and NTV patients. The study also conducted subanalyses comparing levels saved in TVP (LTV on prone radiographs) and TVS (LTV on standing radiographs) patients, as well as subanalyses for different scoliosis classifications. In addition, radiographs of nonoperative adolescents with scoliosis were analyzed as controls. The results showed a significantly greater number of patients in group B with final disk wedging and LIV translation. Utilizing prone radiographs in TVP patients saved an average of 1 level, while TVS patients saved 1.2 levels. Furthermore, TVP patients had similar radiographic outcomes compared to controls in terms of LIV tilt, disk wedging, and coronal balance. They concluded that choosing a minimally rotated LTV on prone radiographs can preserve levels without sacrificing radiographic outcomes.
Applying positional radiographs to LIV selection could lead to more favorable results when considering other factors supported by research on selecting the LIV. For instance, Lenke 1A-R curves were found to be more susceptible to AO than 1A-L curves [20]. To prevent AO in 1A-R curves, LSTV or LTV+1 has been recommended as the optimal LIV. If LTV is set using a supine radiograph, the lumbar motion segment can be preserved while considering Lenke 1A-R curves (Fig. 2). LIV deviation > 2 cm from CSVL was an independent predictive factor for the prevalence of distal AO or DJK [44]. Consequently, the LIV deviation from CSVL should not exceed 2 cm. When applying positional radiographs in LIV selection, it is possible to select the LIV at a more proximal position when the LIV deviation from the CSVL is less than 2 cm (Fig. 3). Because sacral slanting is frequently observed in patients with AIS, it is a critical consideration in selecting the distal fusion level when corrective surgery is planned [45]. For patients with L4-L (L4 vertebral tilt to the left) and left-sided sacral slanting, stopping fusion at L3 could be sufficient to maintain the correction and preserve more of the lumbar motion segment to balance the residual distal curve, which would reduce the risk of decompensation. Exceptionally, in such an instance, even if the LTV is distal to L3 on supine radiographs, favorable outcomes could be obtained by selecting L3 as the LIV (Fig. 4).
The selection of the fusion level in AIS surgery has been at the forefront of spine deformity research. One of the most important long-term goals of corrective surgery is to minimize the fusion extent in order to preserve motion segments while achieving a well-balanced spine and limiting disease progression. The selection of the LIV plays an essential role in AIS correction surgery because inappropriate selection may lead to various complications, such as AO or DJK. Although the selection method has not been standardized, recent studies have shown that basing LIV selection on positional radiographs is promising. Applying positional radiographs (standing, supine, and prone) to LIV selection is expected to be of great help to spine surgeons, since it is a simple, universal, and easy-to-apply method to preserve motion segments to the maximal extent possible. Also, there has been increasing research interest in utilizing three-dimensional analysis for LIV selection in AIS surgery recently. Continued research efforts about the application of three-dimensional analysis in LIV selection will contribute to improving the accuracy and efficacy of fusion level determination, ultimately leading to enhanced surgical outcomes and better long-term stability for patients with AIS.
In summary, future criteria for optimal LIV selection should consider curve flexibility and positional status in order to provide an appropriate surgical strategy for preventing postsurgical AO or distal decompensation.
NOTES
Fig. 1.
A representative case of using the LTV on supine radiographs. (A) Preoperative radiographs of a 15-year-old male patient diagnosed with a Lenke 6CN curve. (B) L4 was touched by the CSVL on an upright radiograph, but the supine LTV was L3 on a supine plain radiograph. (C) Based on the supine radiographs, L3 was chosen as the LIV, preserving one level. Clinical outcomes were excellent at the 18-month follow-up. LTV, last touched vertebra; CSVL, central sacral vertical line; LIV, lower instrumented vertebra.
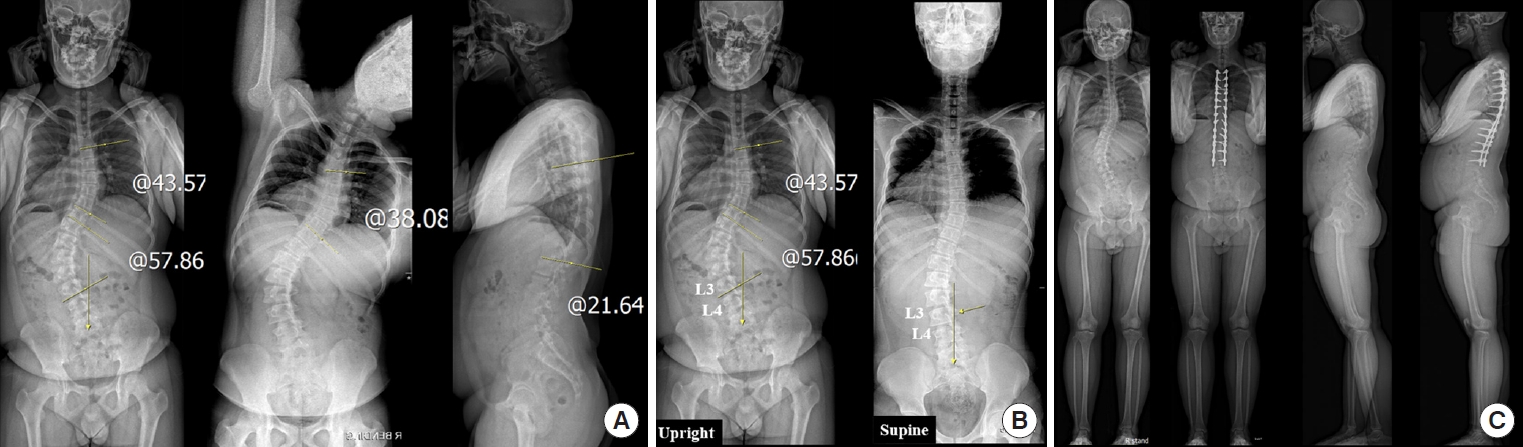
Fig. 2.
A representative case of considering Lenke 1A-R (L4 vertebral tilt to the right) curves. (A) Preoperative radiographs of an 11-year-old female patient diagnosed with a Lenke 1A-R curve. (B) L3 was touched by the CSVL on an upright radiograph, but the supine LTV was L2 on a supine plain radiograph. (C) Since the LTV on supine radiographs was L2, L3 was chosen as the LIV considering Lenke 1A-R curves. At the 1-year follow-up, no AO phenomenon was observed. CSVL, central sacral vertical line; LTV, last touched vertebra; LIV, lower instrumented vertebra; AO, adding-on.
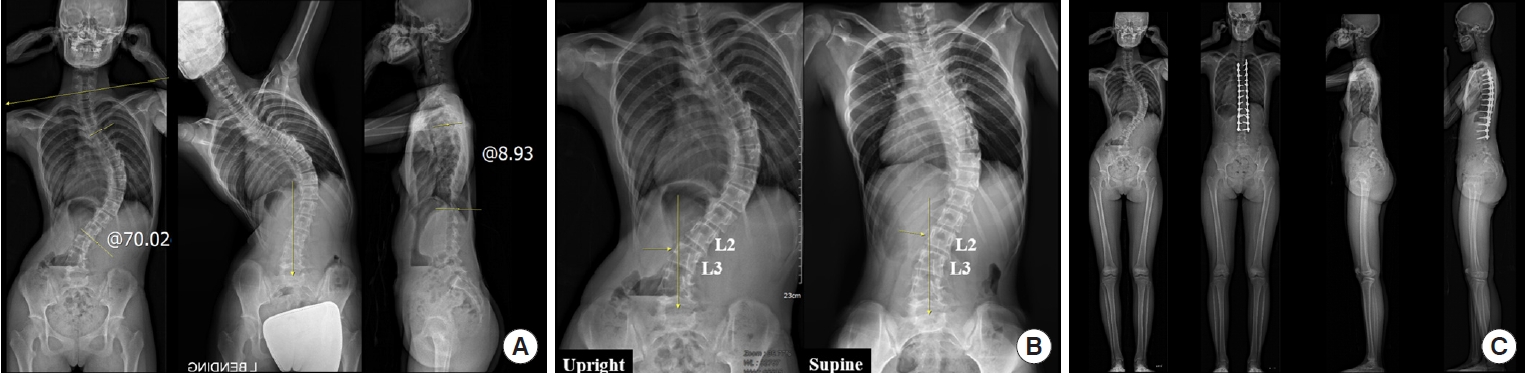
Fig. 3.
A representative case of considering LIV deviation from the CSVL. (A) Preoperative radiographs of a 14-year-old female patient diagnosed with a Lenke 1AN curve. (B) L3 was touched by the CSVL on an upright radiograph, but the supine LTV was L2 on a supine plain radiograph. (C) On an upright radiograph, the L3 deviation from CSVL was less than 1 cm and the L2 deviation was greater than 2 cm, but on a supine radiograph, the L2 deviation from CSVL was less than 2 cm. (D) L2 was chosen as the LIV because the LIV deviation from CSVL did not exceed 2 cm on supine radiographs. At the 1-year follow-up, no AO phenomenon or DJK was observed. LIV, lower instrumented vertebra; CSVL, central sacral vertical line; LTV, last touched vertebra; AO, adding-on; DJK, distal junctional kyphosis.
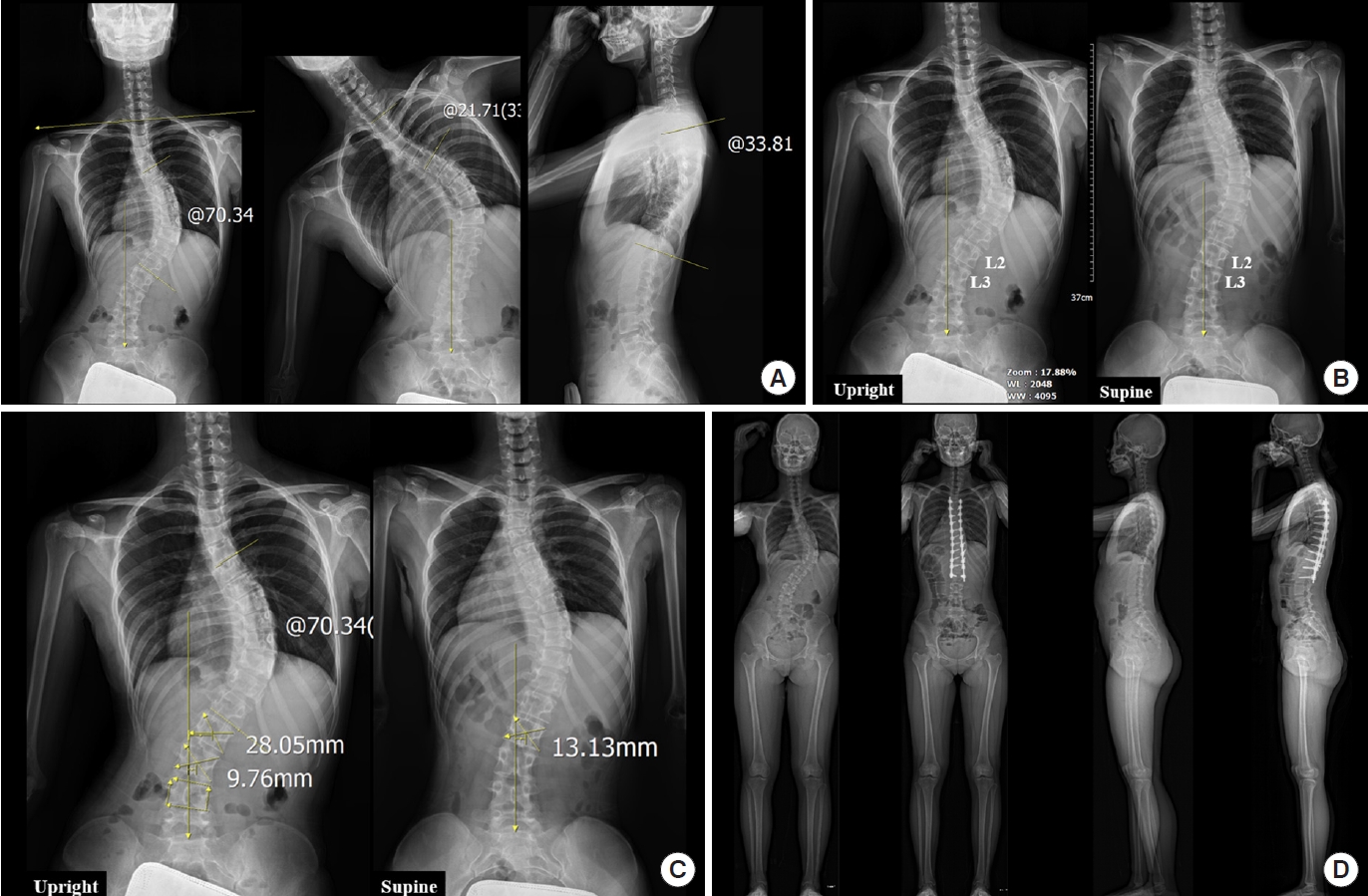
Fig. 4.
A representative case where sacral slanting was continued. (A) Preoperative radiographs of a 16-year-old female patient diagnosed with a Lenke 4CN curve and left-sided sacral slanting. (B) Supine LTV was L4 on a supine plain radiograph. (C) L3 was chosen as the LIV, considering left-sided sacral slanting. As a result, clinical outcomes were excellent at the 4-year follow-up. LTV, last touched vertebra; LIV, lower instrumented vertebra.
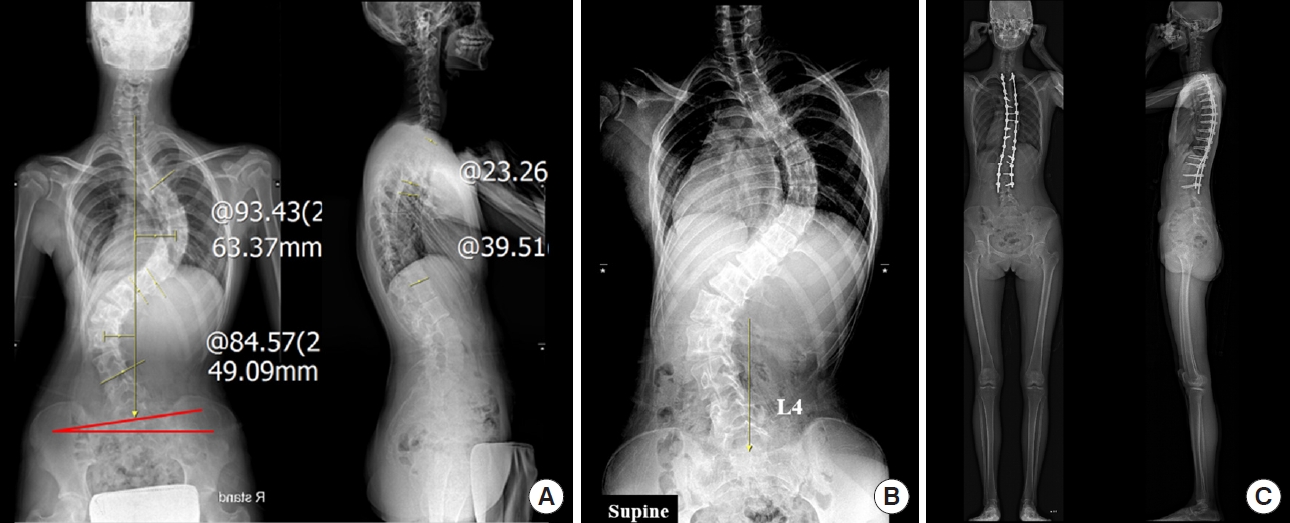
Table 1.
Summary of literatures on LIV selection in AIS
| Study | Curve type | Total No. of patients | Mean age (yr) | Mean follow-up (yr) | Conclusion |
|---|---|---|---|---|---|
| Suk et al. [24] (2003) | King type 3, 4 | 42 | 15.5 | 4.2 | When preoperative NV and EV show no more than 2-level gap differences, fusion down to NV. When the gap is more than two levels, fusion down to NV-1 |
| Parisini et al. [26] (2009) | Lenke type 1A | 31 | 16.3 | Min. 2 | If the rotation of just below the thoracic LEV in the same direction as the thoracic curve, and SV and EV show > 2 level differences, fusion should extended to L2 or L3. Otherwise, SV-2 or SV-3 would be distal fusion level |
| Wang et al. [27] (2011) | Lenke type 1A | 45 | - | 3.6 | Choosing the first vertebra in cephalad direction from sacrum whose deviation from CSVL is more than 10 mm as the LIV provide the best outcome |
| Sarlak et al. [28] (2011) | Lenke type 1A | 36 | 15.8 | 4.3 | Distal fusion level should be extended to LEV-1 in case of neutral L3 vertebra and to LEV in case of L3 vertebral tilt |
| Takahashi et al. [5] (2011) | Lenke type 1B, 1C, 3C | 172 | 14 | 2 | If the SV was below the EV, the LIV should be chosen at least one level distal to the SV. If the SV and the EV are same, the LIV one level below the SV/EV was recommended |
| Cho et al. [20] (2012) | Lenke type 1A | 195 | - | Min. 2 | Selecting the LIV for Lenke type 1A curves should depend on the direction of the L4 tilt |
| For type 1A-R (L4 tilt to right) curves, select an LIV that approaches the NV as well as the LSTV. In type 1A-L (L4 tilt to left) curves, fuse at least one level below the EV | |||||
| Matsumoto et al. [29] (2013) | Lenke type 1A | 112 | 16.1 | 3.6 | Fusion extended at least to the LTV to avoid postoperative AO |
| Lenke et al. [30] (2014) | Lenke type 1A | 65 | - | 5 | Selecting the LTV as the LIV in the Lenke 1A main thoracic pattern, prevented an increase in final CSVL-LIV distance without any AO or angulation/tilt at a minimum 5-year follow-up, and resulted in a significantly better LIV position than when fusing to the LTV-1 level |
| Ding et al. [34] (2014) | - | 60 | 15.4 | Min. 2 | There were no significance differences in the clinical scores between the L3 and the L4 group |
| Sun et al. [35] (2014) | Lenke 5 | 37 | 14.9 | 3.5 | No benefit for fusing to LEV+1 in moderate TL/L idiopathic scoliosis patients than fusing to LEV. TL/L Cobb angle more than 60°, the distal fusion level probably needs to be LEV+1 |
| Kim et al. [39] (2014) | Lenke 5 | 66 | 15.2 | Min. 2 | Fused to L3 showed favorable radiographic outcomes when L3 crosses the midsacral line with rotation of less than grade II in bending film. Otherwise, fusion has to be extended to L4 |
| Lee et al. [41] (2016) | Lenke 3C, 5, 6 | 229 | 15.6 | 3.7 | Fused to L3 may be sufficient if LEV ≥ L3 and LTV ≥ L4 |
| Chang et al. [40] (2017) | Major TL/L curves | 64 | 15.0 | Min. 2 | If the curve is flexible (L3 crosses CSVL with a rotation < grade II), LIV should be selected at L3 (LEV) |
| Fischer et al. [13] (2018) | Lenke type 1, 2 | 544 | 14.7 | 4.1 | LTV or within 2 level proximal to the NV be used as the choice of the LIV |
| Shen et al. [32] (2018) | Lenke type 1A | 55 | 14.2 | Min. 2 | LIV choosing both SV and LSTV can acquire satisfied correction |
| Qin et al. [33] (2020) | Lenke type 2A | 101 | 14.9 | Min. 2 | Extend the fusion level to LSTV in 2A-R (L4 tilt to right) curve and to 1 level distal from LSTV in 2A-L (L4 tilt to left) curve |
| Kim et al. [42] (2022) | Lenke type 1, 2, 3, 4, 5, 6 | 57 | 15.1 | 2.2 | The LTV on preoperative supine radiographs is acceptable as the LIV in AIS surgery to maximize motion segments |
| Sarwahi et al. [43] (2022) | Lenke type 1, 2, 3, 4, 5 | 148 | 14.8 | Min. 2 | Choosing LIV as LTV with minimal rotation on prone radiograph can reduce fusion levels and have comparable radiographic outcomes without AO |
LIV, lower instrumented vertebra; AIS, Adolescent idiopathic scoliosis; NV, neutral vertebra; EV, end vertebra; LEV, lower end vertebra; SV, stable vertebra; Min., minimum; LSTV, last substantially touched vertebra; CSVL, center sacral vertical line; LTV, last touched vertebra; AO, adding-on phenomenon; TL/L, thoracolumbar/lumbar.
REFERENCES
1. Weinstein SL, Dolan LA, Cheng JC, et al. Adolescent idiopathic scoliosis. Lancet 2008;371:1527-37.


2. Szwed A, Kołban M, Jałoszewski M. Results of SpineCor dynamic bracing for idiopathic scoliosis. Ortop Traumatol Rehabil 2009;11:427-32.

3. Razeghinezhad R, Kamyab M, Babaee T, et al. The effect of brace treatment on large curves of 40° to 55° in adolescents with idiopathic scoliosis who have avoided surgery: a retrospective cohort study. Neurospine 2021;18:437-44.




4. Fischer CR, Kim Y. Selective fusion for adolescent idiopathic scoliosis: a review of current operative strategy. Eur Spine J 2011;20:1048-57.




5. Takahashi J, Newton PO, Ugrinow VL, et al. Selective thoracic fusion in adolescent idiopathic scoliosis: factors influencing the selection of the optimal lowest instrumented vertebra. Spine (Phila Pa 1976) 2011;36:1131-41.

6. Goshi K, Boachie-Adjei O, Moore C, et al. Thoracic scoliosis fusion in adolescent and adult idiopathic scoliosis using posterior translational corrective techniques (Isola): is maximum correction of the thoracic curve detrimental to the unfused lumbar curve? Spine J 2004;4:192-201.


7. Kim DH, Hyun SJ, Kim KJ. Selection of fusion level for adolescent idiopathic scoliosis surgery: selective fusion versus postoperative decompensation. J Korean Neurosurg Soc 2021;64:473-85.




8. King HA, Moe JH, Bradford DS, et al. The selection of fusion levels in thoracic idiopathic scoliosis. J Bone Joint Surg Am 1983;65:1302-13.


9. Hyun SJ, Lenke LG, Kim Y, et al. The Incidence of addingon or distal junctional kyphosis in adolescent idiopathic scoliosis treated by anterior spinal fusion to L3 was significantly higher than by posterior spinal fusion to L3. Neurospine 2021;18:457-63.




10. Lee JK, Hyun SJ, Yang SH, et al. Clinical impact and correlations of odontoid parameters following multilevel posterior cervical fusion surgery. Neurospine 2022;19:912-20.




11. Lee JK, Hyun SJ, Yang SH, et al. Reciprocal changes following cervical realignment surgery. Neurospine 2022;19:853-61.




12. Choi HY, Hyun SJ, Lee CH, et al. Safety and efficacy of recombinant human bone morphogenetic protein-2 in multilevel posterolateral lumbar fusion in a prospective, randomized, controlled trial. Neurospine 2022;19:838-46.




13. Fischer CR, Lenke LG, Bridwell KH, et al. Optimal lowest instrumented vertebra for thoracic adolescent idiopathic scoliosis. Spine Deform 2018;6:250-6.


14. Hibbs RA. A report of fifty-nine cases of scoliosis treated by the fusion operation. J Bone Joint Surg 1924;6:3-37.
15. Hibbs RA, Risser JC, Ferguson AB. Scoliosis treated by the fusion operation an end-result study of three hundred and sixty cases. J Bone Joint Surg Am 1931;13:91-104.
16. Harrington PR. Treatment of scoliosis. Correction and internal fixation by spine instrumentation. J Bone Joint Surg Am 1962;44-A:591-610.

17. Majd ME, Holt RT, Castro FP. Selection of fusion levels in scoliosis surgery. J Spinal Disord Tech 2003;16:71-82.


19. Lenke LG, Betz RR, Harms J, et al. Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am 2001;83:1169-81.

20. Cho RH, Yaszay B, Bartley CE, et al. Which Lenke 1A curves are at the greatest risk for adding-on... and why? Spine (Phila Pa 1976) 2012;37:1384-90.


21. Knapp DR Jr, Price CT, Jones ET, et al. Choosing fusion levels in progressive thoracic idiopathic scoliosis. Spine (Phila Pa 1976) 1992;17:1159-65.


22. Lenke LG, Bridwell KH, O'Brien MF, et al. Recognition and treatment of the proximal thoracic curve in adolescent idiopathic scoliosis treated with Cotrel-Dubousset instrumentation. Spine (Phila Pa 1976) 1994;19:1589-97.


23. Newton PO, Faro FD, Lenke LG, et al. Factors involved in the decision to perform a selective versus nonselective fusion of Lenke 1B and 1C (King-Moe II) curves in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2003;28:S217-23.


24. Suk SI, Lee SM, Chung ER, et al. Determination of distal fusion level with segmental pedicle screw fixation in single thoracic idiopathic scoliosis. Spine (Phila Pa 1976) 2003;28:484-91.


25. Potter BK, Rosner MK, Lehman RA Jr, et al. Reliability of end, neutral, and stable vertebrae identification in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2005;30:1658-63.


26. Parisini P, Di Silvestre M, Lolli F, et al. Selective thoracic surgery in the Lenke type 1A: King III and King IV type curves. Eur Spine J 2009;18 Suppl 1(Suppl 1):82-8.



27. Wang Y, Hansen ES, Høy K, et al. Distal adding-on phenomenon in Lenke 1A scoliosis: risk factor identification and treatment strategy comparison. Spine (Phila Pa 1976) 2011;36:1113-22.

28. Sarlak AY, Atmaca H, Kim WJ, et al. Radiographic features of the Lenke 1A curves to help to determine the optimum distal fusion level selection. Spine (Phila Pa 1976) 2011;36:1592-9.


29. Matsumoto M, Watanabe K, Hosogane N, et al. Postoperative distal adding-on and related factors in Lenke type 1A curve. Spine (Phila Pa 1976) 2013;38:737-44.


30. Lenke L, Newton P, Lehman R, et al. Radiographic results of selecting the touched vertebra as the lowest instrumented vertebra in Lenke 1A AIS curves at a minimum five-year follow up. Paper presented at: Scoliosis Research Society 49th Annual Meeting & Course 2014; 2014 Sep 10-13; Anchorage (AK), USA.
31. Qin X, Sun W, Xu L, et al. Selecting the last “substantially” touching vertebra as lowest instrumented vertebra in Lenke Type 1A curve: radiographic outcomes with a minimum of 2-year follow-up. Spine (Phila Pa 1976) 2016;41:E742-50.

32. Shen M, Li N, Luo M, et al. Comparison of SV and LSTV as the lowest instrumented vertebra in Lenke 1A adolescent idiopathic scoliosis: SV decreasing the distal adding-on phenomenon. Int J Clin Exp Med 2018;11:9520-7.
33. Qin X, He Z, Yin R, et al. Selecting the last substantially touching vertebra as lowest instrumented vertebra in Lenke type 2A-R and 2A-L curves. Spine (Phila Pa 1976) 2020;45:309-18.


34. Ding R, Liang J, Qiu G, et al. Evaluation of quality of life in adolescent idiopathic scoliosis with different distal fusion level: a comparison of L3 versus L4. J Spinal Disord Tech 2014;27:E155-61.

35. Sun Z, Qiu G, Zhao Y, et al. Lowest instrumented vertebrae selection for selective posterior fusion of moderate thoracolumbar/lumbar idiopathic scoliosis: lower-end vertebra or lower-end vertebra+1? Eur Spine J 2014;23:1251-7.



36. Ahonen M, Syvänen J, Helenius L, et al. Back pain and quality of life 10 years after segmental pedicle screw instrumentation for adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2023;48:665-71.


37. Marie-Hardy L, Besse M, Chatelain L, et al. Does the distal level really matter in the setting of health-related quality of life? Assessment of a series of adolescent idiopathic scoliosis patients at more than 7 years following surgery. Spine (Phila Pa 1976) 2022;47:E545-50.


38. Lander ST, Thirukumaran C, Saleh A, et al. Long-term health-related quality of life after harrington instrumentation and fusion for adolescent idiopathic scoliosis: a minimum 40-year follow-up. J Bone Joint Surg Am 2022;104:995-1003.

39. Kim SS, Lim DJ, Kim JH, et al. Determination of the distal fusion level in the management of thoracolumbar and lumbar adolescent idiopathic scoliosis using pedicle screw instrumentation. Asian Spine J 2014;8:804-12.



40. Chang DG, Yang JH, Suk SI, et al. Importance of distal fusion level in major thoracolumbar and lumbar adolescent idiopathic scoliosis treated by rod derotation and direct vertebral rotation following pedicle screw instrumentation. Spine (Phila Pa 1976) 2017;42:E890-8.


41. Lee CS, Ha JK, Hwang CJ, et al. Is it enough to stop distal fusion at L3 in adolescent idiopathic scoliosis with major thoracolumbar/lumbar curves? Eur Spine J 2016;25:3256-64.



42. Kim DH, Hyun SJ, Lee CH, et al. The last touched vertebra on supine radiographs can be the optimal lower instrumented vertebra in adolescent idiopathic scoliosis patients. Neurospine 2022;19:236-43.




43. Sarwahi V, Hasan S, Wendolowski S, et al. A newer way of determining LIV in AIS patients: rotation of the touched vertebrae. Spine (Phila Pa 1976) 2022;47:1321-7.



- TOOLS
-
METRICS

-
- 2 Web of Science
- 0 Crossref
- Scopus
- 1,403 View
- 187 Download
- Related articles in NS
-
Journal Impact Factor 3.2


























